Fig. 15.1
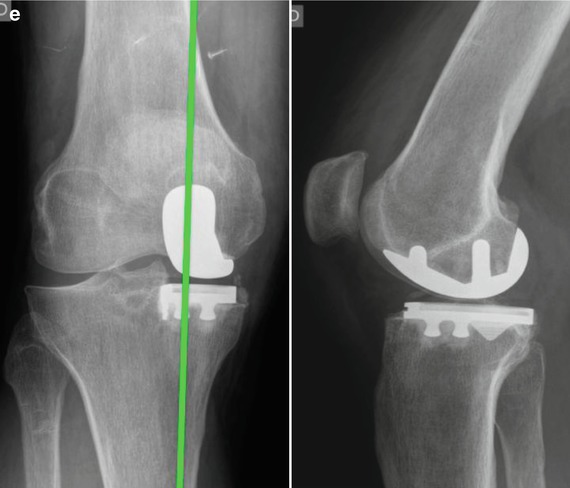
(a–e) Radiographs and clinical images of a 66-year-old man with a painful medial arthritis of the knee that is resistant to the medical treatment. A fixed-bearing UKA was performed in June 2014. (a) Preoperative radiological analysis. Showing frontal and sagittal view, stress radiographs of the right knee: painful osteoarthritis (OA) limited to one compartment of the knee (medial) associated with significant loss of joint space. (b) Before proceeding to the bone cuts, the first step is to bring the knee to 60° of flexion to evaluate the joint by checking the resistance of the ACL with an appropriate hook and evaluating the state of both the opposite tibiofemoral joint and the patellofemoral joint. (c) In our practice, the tibial cut is always performed first with the distal femoral cut. This system therefore provides two cuts in extension linked together. The extramedullary technique is based on the correction of the deformity of the leg in extension using an extramedullary rod that references the ankle and the femoral head. (d) View following cementation of the UKA prostheses. (e) On the postoperative X-ray, the ideal correction as measured on the postoperative full weight-bearing view will probably consist of a tibiofemoral axis crossing the knee between the tibial spines and the lateral third of the tibial medial plateau for a medial UKA. The lateral view of the knee is important also to control the slope of the tibial implant
The full correction of the deformity to neutral on stress radiographs performed with the patient supine using a dedicated knee stress system is also required. The angle between the mechanical axis of the femur and the anatomical axis of the femur should be calculated on the full-length X-ray as well as the mechanical axis of the lower limb. A varus or valgus deformity of the lower limb greater than 15° may represent a contraindication for UKA as the correction of such deformation may require soft tissue release which should not be performed when doing UKA.
If the ACL status is unclear during the clinical exam, magnetic resonance imaging may be useful to confirm that the ACL is intact. Performing an isolated UKA on a deficient ACL knee is possible when the patient is not reporting instability. In a recent paper reporting the results of a matched cohort of patients (with or without ACL), the Oxford team reported successful short-term results of the ACLD group, suggesting ACL deficiency may not always be a contraindication to Oxford UKA as previously thought. The authors however, as a conclusion of their paper, maintained their recommendation that ACL-deficient knee should be considered a contraindication until long-term data is available.
15.2.2 Age and Weight
Age and weight may still represent debatable issues for UKA as the procedure is often presented as an alternative to either osteotomy or TKA. As previously mentioned and according to the results of previously published series, we consider high tibial osteotomy as an attractive and effective joint-preserving procedure for patients under fifty with unicompartmental osteoarthritis and a varus knee [3]. However the risk of failure of HTO increases dramatically for patients with osteoarthritis rated Ahlback grade two or more, and in such cases we consider UKA even in younger patients [16, 17]. Thus, we recently reported very good survivorship in a group of patients under 50, despite greater polyethylene wear than seen in older patients which is also seen in this group following TKA [1, 16]. Early reports of UKA considered obesity a relative contraindication for UKA, but recent studies found no correlation between body weight and outcome, and we concur with the idea that wear is related to activity rather than weight [17]. Obesity itself is therefore not deemed a contraindication.
15.3 Surgical Techniques
15.3.1 Approach
The procedure can be performed under general or epidural anesthesia on a routine operating table. The knee is flexed 90° for skin incision, with or without tourniquet according to surgeon preference, with the foot resting on the table. A minimally invasive sub-vastus approach is performed either medial for the medial UKA or lateral for the lateral UKA. The approach extends proximally in the avascular sub-vastus layer along the septum and distally toward the tibial tuberosity to end 2 cm beneath the joint line. The length of the skin incision varies from 8 to 10 cm depending on skin elasticity. It is important to maintain proper visualization throughout the procedure, and this in part depends on the variation in tissue elasticity. The proximal part of the incision is more essential for the procedure, and two-thirds of the incision should be located above the joint line. Once the synovial cavity is opened, the part of the fat pad in the way of the condyle is excised to properly visualize the condyle, the ACL, and the corresponding tibial side of the tibial plateau. It is important to note that the principles of ligament balancing existing in TKA cannot be applied to UKA because the collateral ligaments should not be released in UKA. Before proceeding to the bone cuts, the first step is to bring the knee to 60° of flexion to evaluate the joint by checking the resistance of the ACL with an appropriate hook (Fig. 15.1b), evaluating the state of both the opposite tibiofemoral joint and the patellofemoral joint. The osteophytes are then removed from the intercondylar notch to avoid late impingement of the ACL.
15.3.2 Tibial Cut and Femoral Distal Cut
It is important to remember that in UKA the proper tension of the ligaments will be restored while filling the gap left by the worn cartilage with the unicompartmental components, and therefore UKA is a so-called resurfacing procedure.
In our practice, the tibial cut is always performed first along with the distal femoral cut (Fig. 15.1c). Thus this system provides two linked cuts in extension. The extramedullary technique is based on the correction of the deformity of the leg in extension using an extramedullary rod that references the ankle and the femoral head. The guide is placed distally around the ankle with the axis of the guide lying slightly medial to the center of the ankle joint. The proximal part of the guide is resting on the anterior tibia pointing toward the axis of the tibial spines. The diaphyseal part of the guide is parallel to the anterior tibial crest, and the anteroposterior position of the guide is adjusted distally to reproduce the natural tibial slope, usually between 5° and 7° of the posterior slope. The sagittal tibial cut is performed to complete the tibial resection. This can be done using one of the sagittal marks provided by the guide or made as a freehand cut. Particular care should be taken to protect the ACL.
15.3.3 Rotational Alignment of the Femoral Cuts
The next challenge concerns the remainder of the femoral cuts (posterior cut and chamfers), which will then be completed using the appropriate cutting block. The rotation setup of the cutting block is the crucial point of the procedure. The basic principle to set rotation is to consider that the midpoint of the femoral component should align with the midpoint of the tibial component both in flexion and in extension. The first landmark is obtained in extension: the distal femoral surface is marked to correspond with the midpoint of the tibial plateau. The center hole of the femoral cutting guide is then aligned with this mark with a pin fixing the anterior part of the cutting guide. The size of the cutting block is determined once this femoral finishing guide is positioned on the distal femoral cut, seeking the best compromise between an anatomically centered position on the femoral condyle and a long axis perpendicular to the resected tibial plateau. The top of this finishing guide should be localized 1–2 mm above the deepest layer of the cartilage to avoid potential impingement between the femoral implant and the patella. The knee is then flexed, and the rotation of the distal part of the femoral cutting guide is adapted to align the middle of the femoral guide with the midpoint of the tibia. Spacer blocks can be used at this step to make sure that the femoral guide is parallel to the tibial plateau. The control of the mediolateral position of the femoral cutting guide, which determines the position of the final implant, is crucial. The medial part of the femoral guide should be aligned with the medial wall of the notch. Once the posterior cut and the chamfers have been made and the cutting guide is removed, removal of any posterior osteophytes is necessary using a curved osteotome to increase the range of flexion and avoid any posterior impingement with the polyethylene in high flexion.
15.3.4 Tibial Finishing and Trials
The size of the tibial tray should now be determined, resulting in the best compromise between maximal tibial coverage and overhang, which might induce pain. The anteroposterior size of the tibial plateau sometimes differs from the mediolateral one, especially for female knees; thus, different sizing trials are necessary to find the best compromise. It is important to keep the depth of the tibial cut as conservative as possible to take advantage of the strength of the tibial cortex and the increased area of contact proximally. The knee is then brought into maximal flexion and internally rotated. The final preparation of the tibia is completed with the appropriate guide with the underlying keel impacted in the subchondral bone. The flexion-extension gaps should then be tested with the trial components in place and inserting a trial polyethylene liner. It is important to search for any impingement of the femur against the spine eminence in extension due to a lack of external rotation in flexion. Once this has been verified, it is important to look for a 2-mm protective laxity checked close to full extension to avoid any overcorrection of the deformity leading to progression of osteoarthritis in the medial compartment. In lateral UKA, the polyethylene insert is often thicker than for the medial side in cases of femoral dysplasia, even if the principle of under correction of the deformity for all cases of lateral UKA remains the basis for successful long-term results. All components should be cemented for better fixation because long-term results suggest that loosening is not a common mode of failure with modern cemented, metal-backed components. The tibial component is cemented first with the knee in full flexion and internally rotated to improve the exposure of the lateral compartment. Once the femoral implant has been cemented, bringing the knee close to extension helps to remove any posterior cement. Finally, the polyethylene can be inserted in flexion after cleaning and drying the tibial implant (Fig. 15.1d).
The ideal correction as measured on the postoperative full weight-bearing view will probably consist of a tibiofemoral axis crossing the knee between the tibial spines and the lateral third of the medial tibial plateau for a medial UKA (Fig. 15.1e) [18–24].
Weight bearing is recommended immediately postoperatively. Painless, active manual range of motion physiotherapy is performed the day after surgery.
15.4 Results of Modern UKA
15.4.1 Mobile-Bearing UKA
Mobile-bearing UKA, using a specific design (Oxford; Biomet, Warsaw, Ind), has shown a recent increase in use. The challenges with a mobile-bearing design include technical issues of ligament balancing with the potential risk of bearing dislocation. Murray et al. [25] reported 98 % cumulative prosthetic survivorship at 10-year follow-up. Price et al. [26], using the same implant, found a 15-year survivorship of up to 92 %. However, they noted a high frequency of complete radiolucent lines around the tibial component in half of the tibial components. Other studies suggest contradictory results with similar mobile-bearing implants. Vorlat et al. [27] reported an 84 % survival of 149 consecutive Oxford knees at 5.5 years. In the United States Investigative Device Exemption study, 125 Oxford UKAs were followed at 8 sites [28], and the authors found at 7 years only 80.6 % of survivorship, with a clinical success rate of only 74.2 %. In the current literature, we found 3 comparison studies evaluating fixed-bearing versus mobile-bearing designs. Confalonieri et al. [29] found no statistical difference in outcome. Gleeson et al. [30] found three bearing dislocations in the mobile-bearing group and four additional revisions (versus three revisions in the fixed-bearing group). To summarize these studies, the functional results of both implants are similar, and comparative studies show no consensus between mobile-bearing and fixed-bearing designs with regard to function, success, or recovery. We prefer to use a fixed-bearing design as mobile-bearing designs still present a potential risk of bearing dislocation.
15.4.2 Fixed-Bearing UKA
To confirm our suspicions regarding mobile-bearing designs, we presented in 2011 our results in terms of survivorship of fixed- versus mobile-bearing UKA in young patients [31]. We retrospectively reviewed 75 patients (79 knees) with a fixed-bearing UKA and 72 patients (77 knees) with a mobile-bearing UKA operated on between 1989 and 1992. The mean age of the patients was 63 years; gender and body mass index (26 kg/m(2)) were comparable in the two groups. We obtained Knee Society function and radiographic scores and determined survivorship. The minimum follow-up was 15 years (mean, 17.2 ± 4.8 years; range, 15–21.2 years). Radiographically, the number of overcorrections and the number of radiolucencies were statistically higher in the mobile-bearing group (69 % versus 24 %), but at final follow-up, considering revision for any reason, 12 of 77 (15 %) UKAs were revised (for aseptic loosening, dislocation, and arthritis progression) in the mobile-bearing group and 10 of 79 (12 %) in the fixed-bearing group (for wear and arthritis progression). This difference did not reach significance.
Factors such as wear, joint load, and the type of prosthesis must be taken into account for each patient [17, 32–34]. Based on our results and previous reports, decreasing wear seems to be the main factor in improving the long-term results of a UKA [17, 35]. Two major symptoms could be observed when polyethylene wear occurred, medial knee pain without signs of inflammation and progressive nontraumatic coronal instability. There was no clinical or biological sign of infection. Physical examination is important to confirm the development of coronal instability in these patients. When these symptoms occurred, we performed weight bearing and varus and valgus stress radiographs to confirm wear and look for osteolysis. Usually, exchange of the polyethylene insert is a viable option when no evidence of infection, loosening, or osteolysis has been found. In all other cases a revision of the UKA should be discussed with the patient.
15.4.3 Lateral UKA
Midterm and long-term studies suggest reasonable outcome at 10 years with survivorship greater than 95 % of UKA performed for medial osteoarthritis or osteonecrosis [14], but limited long-term follow-up data are available for lateral UKA in the literature [36–38]. The authors of one small series of UKA in the lateral compartment reported only one failure out of 19 patients at 89 months of follow-up [38]. Anatomic and biomechanical characteristics are different in either of the knee’s femorotibial compartments, and similar surgical treatment may not provide reproducible results when applied to a different compartment [36–38]. UKA in the lateral compartment is technically more challenging and 10 times less performed than medial UKA, (representing less than 1 % of all knee arthroplasty procedures) [39]. Our published series of 39 lateral UKA demonstrated reasonable clinical and radiographic results, with survivorship at 10 and 16 years comparable to the survivorship obtained for medial UKA. Sah and Scott [38, 40] reported no revision at 5 years in a group of 49 knees implanted with lateral UKA. However, Gunther et al. [37] reported a 21 % failure rate using the mobile-bearing Oxford unicompartmental prosthesis in the lateral compartment with a 10 % rate of bearing dislocation. This difference with the commonly reported high-functioning long-term outcomes using the same implant for the medial compartment may be explained by the amount of femoral translation of the lateral condyle, while the medial side remains fairly stationary [37]. When studying the in vivo kinematics of patients implanted with either a medial or lateral UKA, we showed an important posterior femoral translation of the lateral condyle during flexion compared to the medial condyle [41, 42].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








