(1)
Department of Orthopedic Surgery ASAN Medical Center, University of Ulsan College of Medicine, Seoul, Korea, Republic of South Korea
Abstract
If arthritis is confined to one compartment of the knee joint, it may be difficult to decide whether to perform unicompartmental knee arthroplasty (UK) or TKA. This is because widely varying results of UK have been reported in literature. There has been renewed interest in UK after Repicci introduced the minimally invasive techniques for UK. UK has certain advantages over TKA, and good results can be achieved in well-selected patients.
If arthritis is confined to one compartment of the knee joint, it may be difficult to decide whether to perform unicompartmental knee arthroplasty (UK) or TKA. This is because widely varying results of UK have been reported in the literature. There has been renewed interest in UK after Repicci introduced the minimally invasive techniques for UK. UK has certain advantages over TKA, and good results can be achieved in well-selected patients.
Generally, UK refers to medial or lateral unicondylar knee replacement, but patellofemoral arthroplasty (PFA) performed for patellofemoral arthritis can also be classified into unicompartmental arthroplasty. Hence, I have included patellofemoral arthroplasty in this chapter.
Although concomitant replacement of the medial compartment and the patellofemoral joint cannot be termed as unicompartmental knee arthroplasty in the strict sense, the basic concept for it came from unicompartmental knee arthroplasty. Hence, I have briefly described bicompartmental knee arthroplasty in the last section of this chapter.
6.1 Unicompartmental Knee Arthroplasty
6.1.1 Introduction
Arthritis confined to one compartment of the knee joint or a small chondral lesion in one compartment of the knee joint can be treated by chondroplasty, chondrocyte transplantation, osteochondral graft, high tibial osteotomy (HTO), UK, or TKA.
UK offers many advantages such as higher early success rate and good function since the healthy tissues are preserved. Recently better results have been reported due to the improvement in surgical techniques and development of new prostheses. The incidence of UK was 6–8 % of all TKAs performed in the USA in 2008.
6.1.1.1 UK vs. HTO
A comparison of UK with HTO revealed that HTO is indicated in relatively younger, more active, and heavier patients, whereas UK is indicated in relatively slender patients below 60 years of age or above 80 years of age and who are less active.
UK has a good initial success rate and has minimal complications, whereas HTO causes less improvement in pain and the prognosis following HTO worsens rapidly over time. However, the advantage of HTO is that it allows the patients to retain their own joints and achieve a better ROM postoperatively than that after UK. Bone graft or metal augmentation may not be required in revision of a failed HTO to TKA, although it is not easy to perform revision to TKA. Stukenborg et al. reported that the 10-year survival rate of UK was 77 % and that of HTO was 60 %.
6.1.1.2 UK vs. TKA
The advantage of UK in comparison with TKA is that healthy tissues are retained. As a result, UK provides more normal knee mechanics, and hence greater ROM and better proprioception can be expected. The operation time is shorter, and morbidity and length of hospital stay are reduced. However, aligning the axis is more difficult in UK than in TKA and malalignment may cause adverse effects on the adjacent part of the knee joint. Therefore, more skill is required for performing UK since the scope for an error is very narrow.
Many reports revealed that the clinical results of the two operations are similar. In terms of function, UK shows better results than TKA, yet TKA provides better pain relief and increased survival rate. Newman et al. reported that UK showed better results than TKA at the first 5-year follow-up. Noticewala et al. reported that the patients who underwent UK showed higher SF-12 physical and mental score component, and better WOMAC scores than TKA. However, Lyons et al. reported that even though UK showed higher postoperative scores, the changes of scores between UK and TKA is similar in both groups. It means that the preoperative status of UK patients is better than TKA. McAuley et al. demonstrated that revision after UK is easier than revision after TKA. However, Padgett et al. stated that when UK was performed as compartment replacement instead of surface replacement, 26 % of patients who underwent UK showed bone defects, and bone grafting or metal augmentation was needed in many cases, thereby making the revision a bit difficult to perform. Furthermore, Lai and Rand reported that the results of revision after UK were not any better than those after TKA due to the high incidence of loosening. In this respect, some authors are more in favor of TKA than UK (Fig. 6.1). However, the current techniques using surface replacement demonstrate that the results of conversion of failed UK to TKA are similar to those after primary TKA.
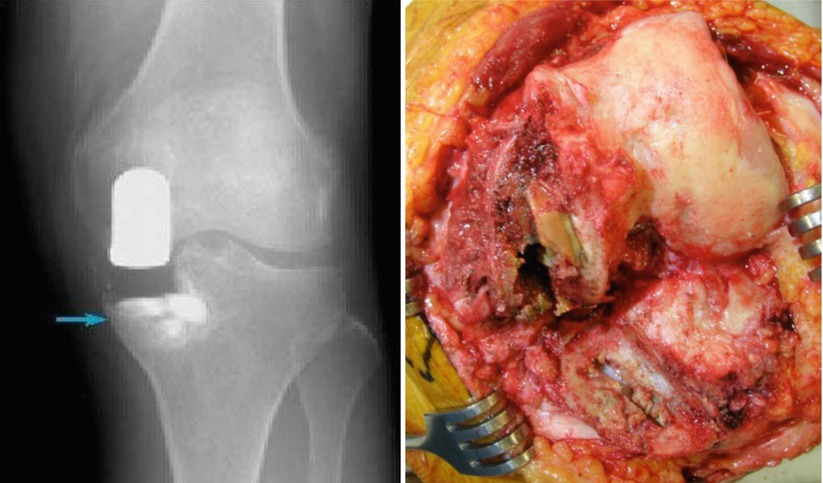
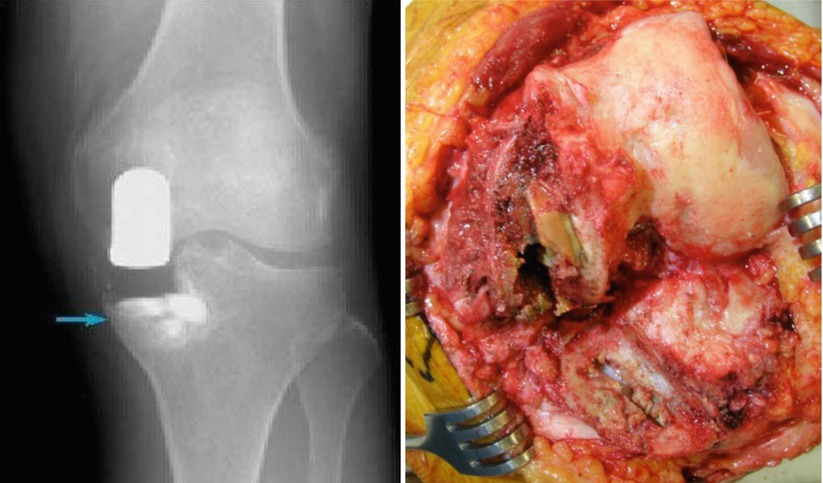
Fig. 6.1
Bone defect due to failure of unicondylar arthroplasty. Left: Bone defect in failed UK on X-ray as indicated by the arrow. Right: Intraoperative finding
6.1.2 Implant
6.1.2.1 History
Historically, the first modern UK was designed by McKeever in the 1950s; it was a type of hemiarthroplasty of the tibial surface with metals and the main cause of failure was loss of the femoral cartilage. In 1970s, Marmor solved this problem by performing femoral resurfacing simultaneously and this was the first type of cemented UK. The femoral part was made of stainless steel and the tibial part was totally made of PE (polyethylene). It was designed so as to retain as much bone as possible. The new version of the St. George Sledge type has a biconvex metal femoral component and a PE tibial component.
Brigham added metal bars on the inner side of the femoral prosthesis for ensuring rotational stability and increased the width of the femoral prosthesis to reduce the incidence of subsidence. The tibial component was made of metal-backed PE. However, it was proved later that the metal-backed PE increased the wear rate. The Oxford type was developed in the late 1970s. In this type, the mobile congruous design of PE in the shape of a meniscus was adopted so as to reduce the wear and loosening. There are other types such as Miller–Galante and Repicci UK (Fig. 6.2).


Fig. 6.2
Various types of unicompartmental knee prostheses. (a) Marmor modular knee, (b) George Sledge unicompartmental replacement, (c) Oxford unicompartmental meniscal knee replacement, (d) Repicci II, (e) Miller-Galante unicompartmental prosthesis
6.1.2.2 Design
The design of the prosthesis varies according to the degree of conformity, whether it is fixed bearing or mobile bearing and whether it has an all-poly or a metal-backed PE tibial component.
With respect to conformity, the incidence of loosening increases as the conformity increases and the incidence of wear increases as the conformity decreases after UK, which is similar to that after TKA. The design with round femoral condyles and flat tibia increases the stress concentration, thereby increasing the wear rate, and causes joint instability as a result of gradual weakening of the ACL (anterior cruciate ligament), which further increases the wear rate. Since a smaller diameter of the posterior condyle and a flat PE tend to increase the wear rate, most of the current designs have a larger diameter of the posterior condyle with an adequate degree of conformity to the PE. Earlier designs had a narrower femoral prosthesis, thereby causing subsidence, whereas in the current designs, the width of the femoral prosthesis is maximized so that it can cover the articular surface as much as possible.
Mobile-bearing PE was developed so as to decrease the wear and loosening. This design has more advantages compared to the fixed-bearing design. The added advantage of mobile-bearing PE in UK is that it allows for resurfacing, which reduces the amount of bone resection as well. However, the drawbacks of this design are that the operation is more difficult to perform, more resection of the anterior portion of the tibia is required, the PE may not move, and joint instability such as PE dislocation can occur.
Cementless type of UK has been designed, but micromotion of the prosthesis makes bony ingrowth difficult. Therefore, the cemented type of prosthesis is currently preferred.
Femoral Component
The design of the femoral component varies according to the width, the curvature of condyles, and the method used to reinforce the fixation of the prosthesis. The current design aims to restore anatomy of the posterior condyle so as to cover the posterior condyle fully and to taper the anterior femoral edge below the subchondral bone so as to reduce the chances of patellar impingement.
For fixation, a fin, pod, or lug is used. For rotational stability, some designs have two lugs, a metal bar or a cruciform groove (Fig. 6.3). In general, relatively small fixation lugs appear to be sufficient as long as there are two lugs or some type of a fin is present to ensure rotational stability.
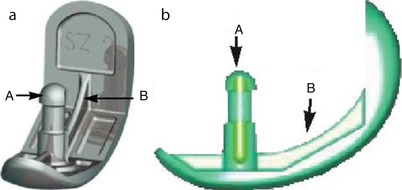
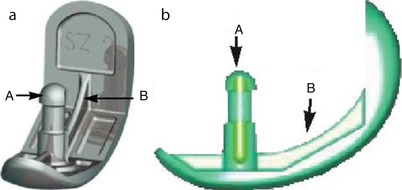
Fig. 6.3
The design for improving fixation of the femoral prosthesis. It has a lug (a) and a fin (b)
Tibial Component
The shape of the tibial component should be as anatomical as possible. Even with the use of theoretically optimized designs, a maximum of 76 % of the implant edge lay on cortical bone. Hence, personalized implants will play an important role in the future.
The earlier form of the tibial component was all-poly tibial component, and metal-backed PE was developed later. Metal-backed PE has the advantage of even load distribution, and the PE is exchangeable when it has worn out. On the other hand, the drawback of metal-backed PE is that the PE has to be thinner. There are many debates between the advantages and drawbacks of all-poly and metal-backed PE. The thickness of PE should be at least 6 mm at the thinnest portion regardless of the type of PE so as to reduce the wear. If the PE is thinner than 6 mm, it not only increases the wear rate, but the wear particles are also precipitated in the cartilage of other parts of the joint, causing progression of arthritis.
Currently, designs that minimize bone resection through surface replacement have been developed in order to make revision easier. In these designs, the thickness of PE has been reduced, and this causes the same problems as those with the use of metal-backed PE (Fig. 6.4).
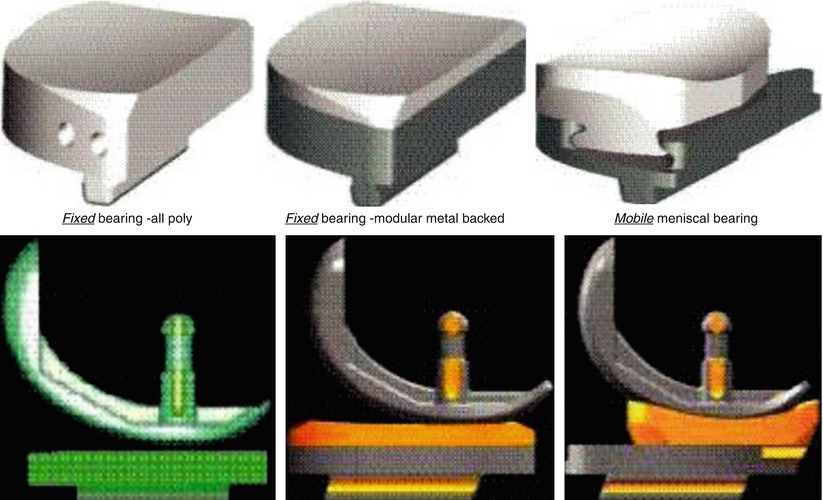
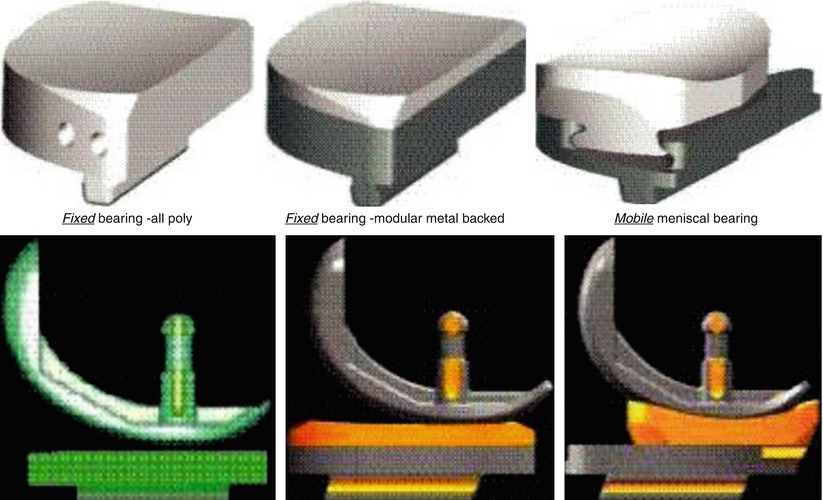
Fig. 6.4
Various types of tibial prostheses
Mobile-bearing PE has been designed to reduce the wear and loosening.
6.1.3 Indications
UK has been indicated in aged patients with unicompartmental arthritis who are slim and relatively inactive. However, the indications for UK can be widened by dividing the patients into two groups. The first group comprises of the relatively younger and nonobese patients who regard the UK as the first operation that will be followed by a subsequent arthroplasty. The second group comprises of the patients above 80 years of age with life expectancy of less than 10 years, who can benefit from the short operation time, early recovery, and low morbidity. Spontaneous osteonecrosis of the knee (SPONK) which is the necrosis confined to the subchondral bone on MRI can be a good indication for UK. Laskin demonstrated that UK could be performed in about 15 % of the patients requiring TKA.
The preoperative ROM should be at least between 10° and 90°, the medial collateral ligament should be intact, and there should not be more than 5° of varus deformity or 10° of valgus deformity on standing X-ray.
If the joint has subluxation of 3 mm or more or there is a so-called kissing lesion (Fig. 6.5 ) wherein the femoral notch and the tibial spine overlap due to instability of the femorotibial joint, it should not be considered as an indication for UK. However, some surgeons perform UK in spite of the kissing lesion.


Fig. 6.5
Kissing lesion (arrow)
Dennis et al. emphasized the importance of the ACL in UK. If the function of the ACL is inadequate, it has an adverse effect on UK and causes weakening of the muscle power or loss of function progressively. It also causes wear in the anterior portion of the prosthesis due to load concentration on this part on weight bearing. In terms of the mechanical aspect, Argenson expressed the same opinion stating that a healthy ACL is needed to maintain normal knee function. In his research using videofluoroscopy, he showed that −0.8 mm of femoral rollback occurred after medial resurfacing and −2.5 mm of femoral rollback occurred after lateral resurfacing in the ACL-deficient patients. Goodfellow et al. also reported that unhealthy or injured ACL contributed to a failure rate that was greater than ten times. Therefore, if there is instability of the collateral ligament or ACL on anterior–posterior and varus–valgus stress X-rays, it is a contraindication for UK.
There are different theoretical perspectives on the patellar lesion with respect to the indication for UK. Generally it is accepted that UK is not indicated if there is exposed patellar subchondral bone, although minimal chondromalacia is not a big problem. However, Beard et al. and Kang et al. reported that the results were not very different even for severe patellar arthritis if there was no bone defect.
UK is known to be a relatively contraindicated in patients with rheumatoid arthritis or other inflammatory arthritis because they have progressive inflammatory changes in the other compartment and it may be associated with relaxation of the ligament tissues. Although UK is relatively contraindicated in obese patients, a recent study has found no correlation between weight and outcomes. Since the wear is more related to activity than to weight, obesity itself may not be a contraindication. Some surgeons do not recommend lateral compartment arthroplasty in obese patients since the result is not as good as that of medial arthroplasty.
UK is contraindicated in patients with osteonecrosis because they are mostly young and loss of fixation may occur due to extensive bone necrosis (Fig. 6.6).
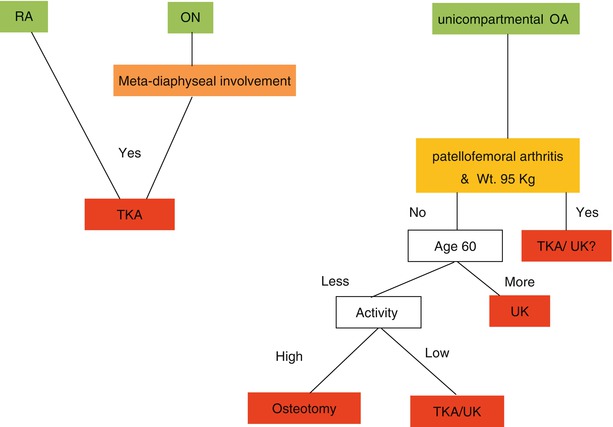
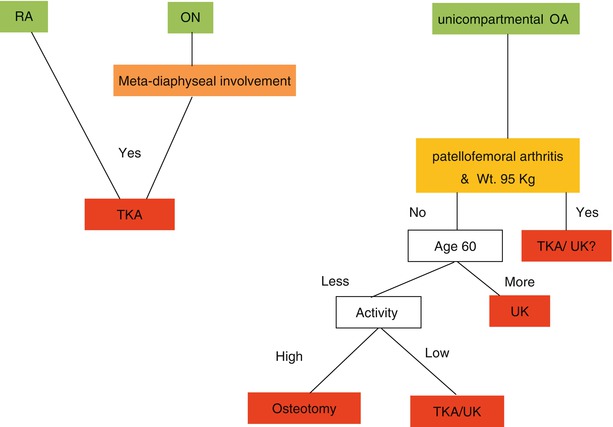
Fig. 6.6
Algorithm for indications of unicondylar arthroplasty
6.1.4 Surgical Technique
6.1.4.1 Approach
Although the ordinary TKA approach can be used, minimally invasive surgery (MIS) is currently recommended. In case of medial replacement, a parapatellar skin incision measuring about 7–8 cm is made starting from about 1 cm proximal to the superior pole of the patella and extending to the tibial tuberosity or about 2 cm distal to the joint line. Although a lateral skin incision is often made for lateral UK, a midline incision may be chosen considering the possibility of a subsequent TKA that might be performed in the future.
Arthrotomy is done paramedially and the quadriceps tendon is often spared (Fig. 6.7).


Fig. 6.7
Skin incision for MIS in UK (Courtesy of MH Song)
When opening the knee joint, care should be taken so as not to damage the ACL, medial collateral ligament, and the anterior horn of the lateral meniscus.
If there are pathology on anterior or posterior cruciate ligaments, there is medial–lateral instability, or if there is severe arthritis of the unreplaced part of the knee joint or of the patellofemoral joint, TKA should be performed instead of UK. The arthritis in the unreplaced part of the knee joint should not be greater than grade II and patellofemoral arthritis should not be greater than grade IV.
Author’s Opinion

Good results can be expected after minimally invasive UK if the patients are selected carefully and the operation is done by an experienced surgeon. Since alignment and soft tissue balancing are important, minimally invasive UK is recommended for balancing the soft tissues naturally.
However, minimally invasive UK has some accompanying problems; the operation is wholly dependent on the comfort level and experience of the surgeons in working on the posterior side due to limited exposure. Hence, a learning curve is needed for performing minimally invasive UK. However, I think faster recovery and less morbidity override these drawbacks.
6.1.4.2 Soft Tissue Procedure
The meniscus should be resected, and the spur in the intercondylar notch, in the periphery of the tibia and femur, should be removed. In medial replacement, it is possible to achieve a certain level of passive correction of the varus deformity by removing the spur on the medial side of the tibia (Fig. 6.8).
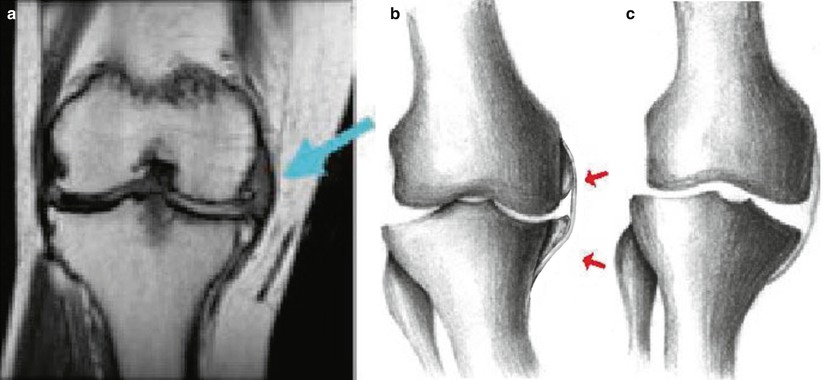
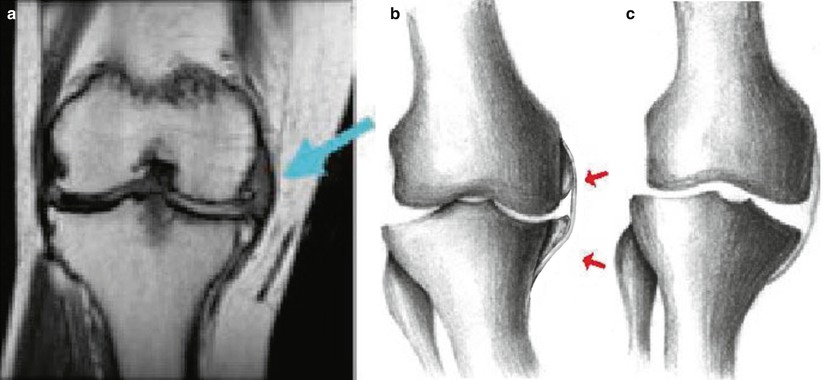
Fig. 6.8
The influence of the spur on the medial side on ligament balancing. (a) Influence of the spur on the collateral ligament on MRI, (b) illustration, (c) effect of collateral ligament release after removal of the spur
The principles of ligament balancing followed in TKA cannot be applied to UK. The medial collateral ligament should be released till the retractor can just be inserted. If the medial collateral ligament needs to be released to a greater extent, it can cause joint instability and progressive arthritis of the unreplaced, i.e., lateral part of the knee joint. Hence, TKA should be considered instead of UK if the medial collateral ligament needs to be released to a greater extent because of the varus deformity.
6.1.4.3 Osteotomy
Osteotomy can either be performed first on the femur or on the tibia.
If osteotomy is performed first on the femur, an intramedullary guide is used for femoral osteotomy. On the other hand, if osteotomy is performed first on the tibia, spacer block is used for femoral osteotomy in relation to tibial osteotomy. Whiteside suggested that the use of an intramedullary guide on the femoral side is more accurate than the extramedullary one and yields higher reproducibility. In any case, an attempt should be made to preserve as much bone as possible. The femur should be aligned with the mechanical axis in extension and it should be perpendicular to the tibia in flexion. Overcorrection should be avoided at any cost. Some authors recommend undercorrection because 4°–7° valgus femorotibial angle according to the mechanical axis imposes excess load on the lateral side.
If the femur is resected first, reamer for an intramedullary guide is inserted just above the intercondylar notch where the PCL is attached. The knee is flexed by 90° and the intramedullary guide which is attached the distal femoral cutting guide is inserted such that the guide is parallel to the tibial cutting surface or perpendicular to the tibial axis (Fig. 6.9).


Fig. 6.9
Guide for performing femoral osteotomy
For distal resection, gradual resection is done by every millimeter up to the first 6 mm with the angle adjusted preoperatively, and an additional 2 mm can be resected if the valgus angle exceeds 6°. This technique can help to increase the extension gap and decrease the valgus deformity without performing additional osteotomy of the tibia. However, Scuderi recommended more tibial resection as more distal resection of the femur only exaggerates the deformity and increases the chances of loosening. Posterior condyle should be resected as much as possible so that the posterior space is not too narrow.
The A–P size of the implant is important; a larger implant should be chosen if the size of the implant is in between sizes; however, about 1 mm of cutting surface of the articular portion should be left uncovered (Fig. 6.10). Therefore, it is recommended to do osteotomy with the larger implant size first. The prosthesis should fully cover the distal articular surface so that the articular cartilage does not articulate with the tibial component on weight bearing, and the junction between the articular cartilage and the prosthesis should be smooth so that the patella can move smoothly. Intraoperative reference of coverage is the “tide mark,” which is the junction of the anterior and distal femoral condyles (Fig. 6.11). However, it is recommended to use a slightly smaller femoral prosthesis for lateral replacement as larger prosthesis can cause more problems in the patellofemoral joint.
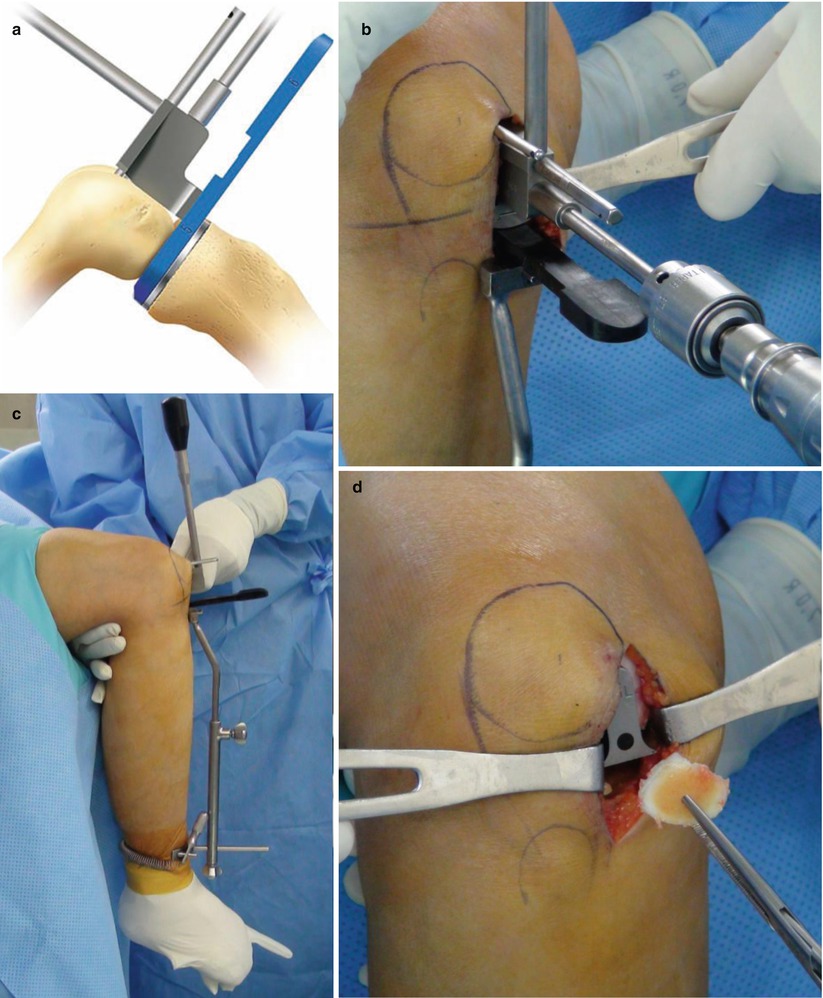
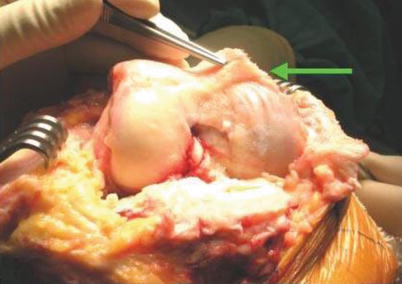
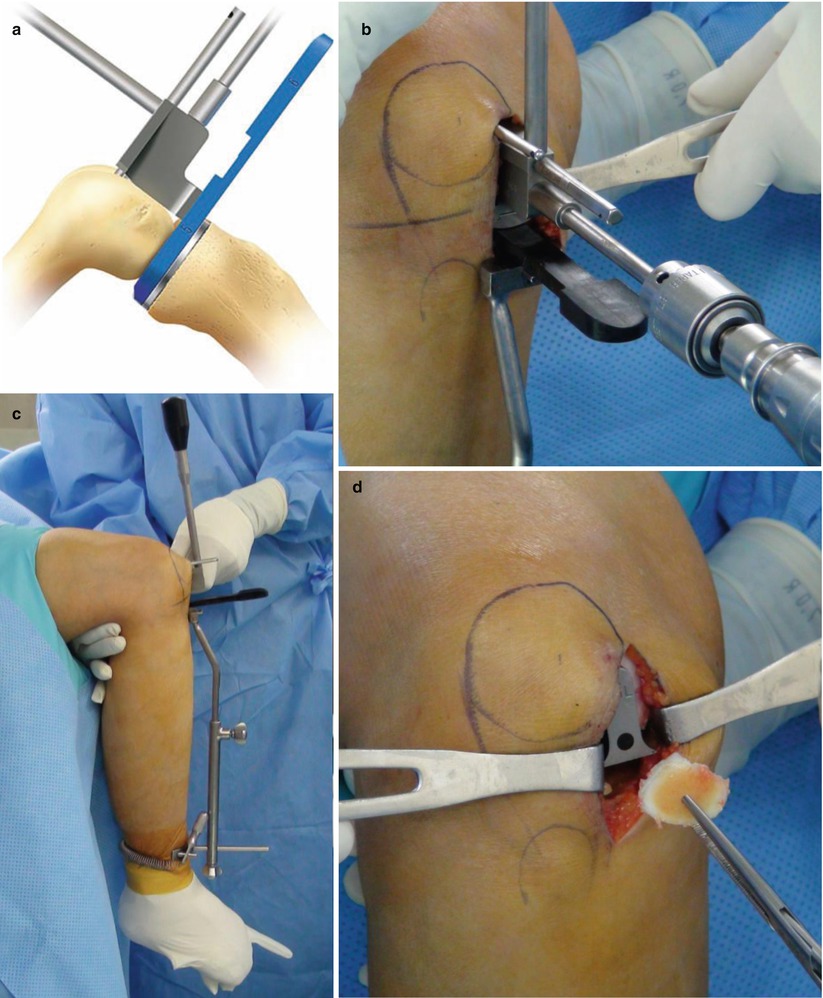
Fig. 6.10
Posterior femoral osteotomy (Courtesy of MH Song/ Biomet, Warsaw, IN). (a, b) Posterior cutting instrument in place. (c) Checking the alignment with the posterior cutting instrument. (d) Removing the bone fragment after posterior cutting
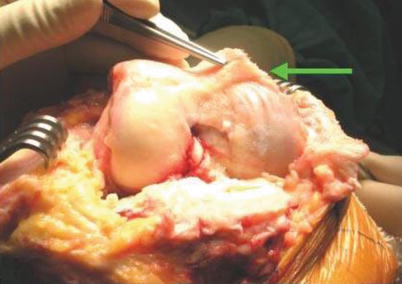
Fig. 6.11
Tide mark
The femoral prosthesis should not protrude distally so as not to interfere with patellar tracking. This technical error is commonly caused by performing too little distal osteotomy and malpositioning of the prosthesis. The femoral prosthesis should be placed in the center of the tibial prosthesis upon extension, and then the femoral slope is matched with that of the tibia.
If the femoral prosthesis is too close to the intercondylar notch, there will be medial subluxation of the tibia, thereby causing edge loading on PE, or there will be impingement of the femur on the tibial spine. To prevent this occurrence, the femoral prosthesis can be shifted on the medial side for medial UK, and the tibial prosthesis can be shifted slightly on the medial side for lateral UK. The trial implant which can cover the most of the bone leaving a 1 mm of exposed bone is inserted.
To set the rotation, the joint is gradually extended from 90° of flexion to flexion angles of 60°, 30°, and 0°. Rotational alignment is closely related to the wear in UK. So the prosthesis should be slightly externally rotated, but this should not be more than 5° (Fig. 6.12).
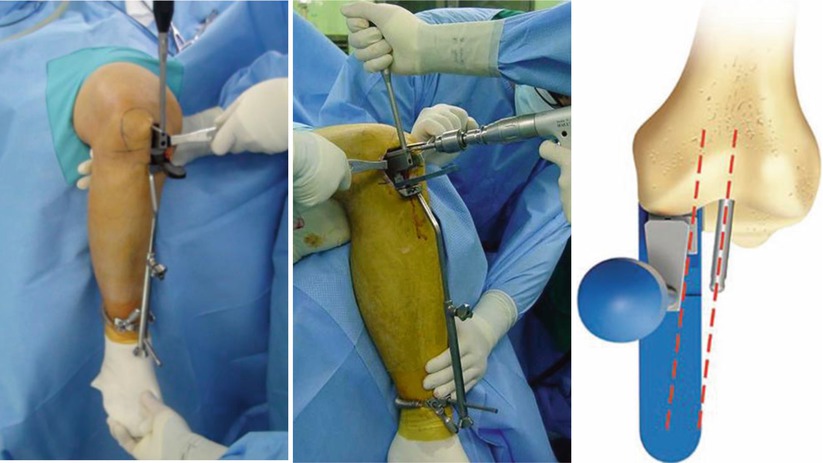
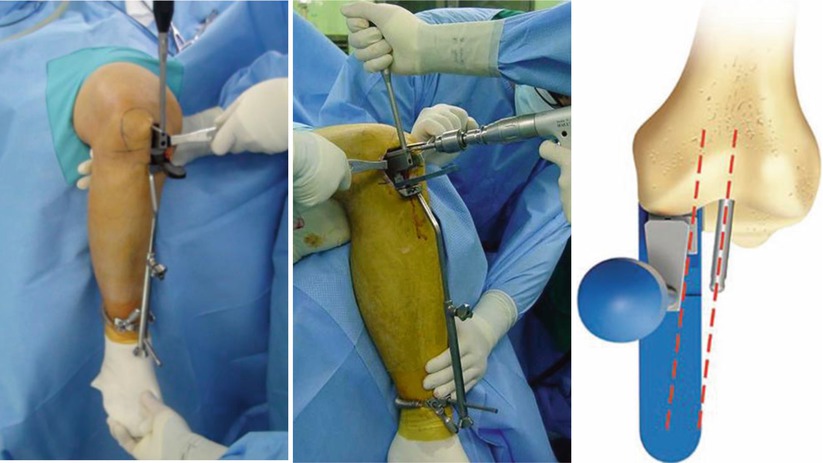
Fig. 6.12
Size and rotation of the femoral prosthesis (Courtesy of MH Song/ Biomet, Warsaw, IN)
Tibial resection is performed using an extramedullary guide and the procedures are the same as those used for TKA. The medial osteotomy is done until the subchondral bone is resected at the deepest point, and in the lateral UK, 8–10 mm of bone is resected. During osteotomy, overcorrection is not recommended as it can cause subluxation of the joint and progressive arthritis in the unreplaced part of the knee joint.
Each surgeon has a different opinion about the degree of osteotomy, but undercorrection by 2°–3° is recommended by most surgeons so that the mechanical axis passes through the medial one-third of the medial condyle (Fig. 6.13). Gulati et al. demonstrated that a mild varus deformity does not significantly affect the clinical results or survival rate. However, a varus deformity greater than 5° increases the possibility of a rotational deformity and increases the wear rate and cartilage damage in the lateral condyle.
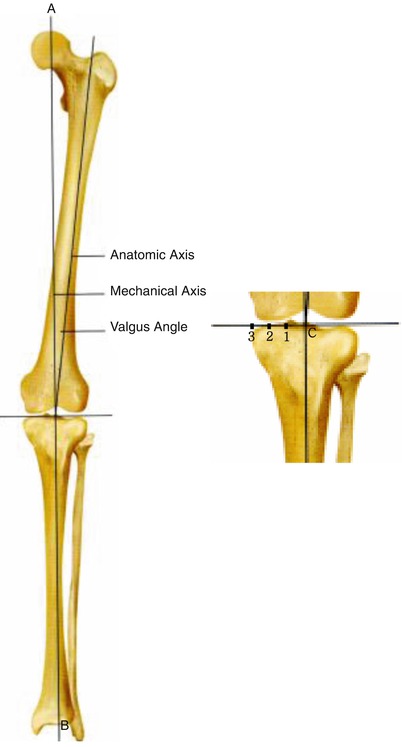
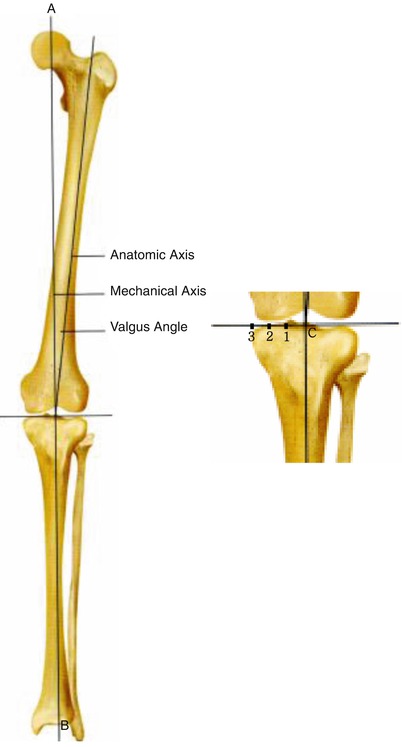
Fig. 6.13
The ideal point at which the mechanical axis drops on the tibial plateau. (a, b) Mechanical axis, best zone: The point at which the mechanical axis of the femur meets the tibial plateau at the point between center (c) and medial 1/3
Anterior–posterior slope should be between 0° and 10°; however, a 3°–5° slope is preferable according to the preoperative slope.
Vertical osteotomy is done as close to the tibial spine as possible, but up to a point where the cruciate ligaments are not injured (Fig. 6.14).
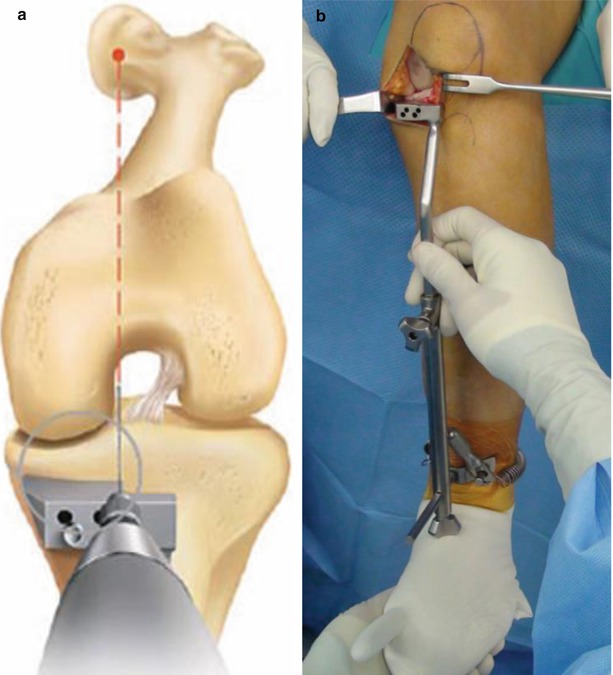
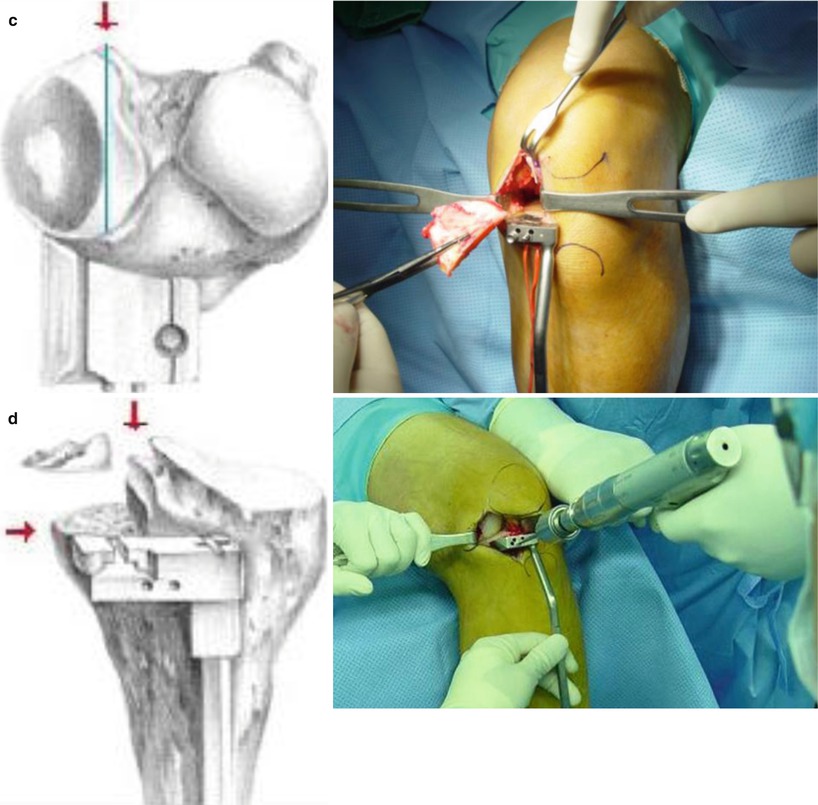
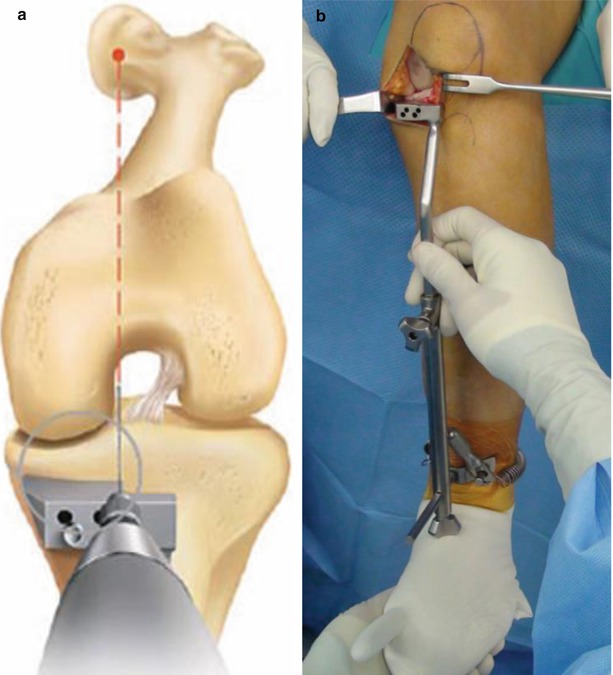
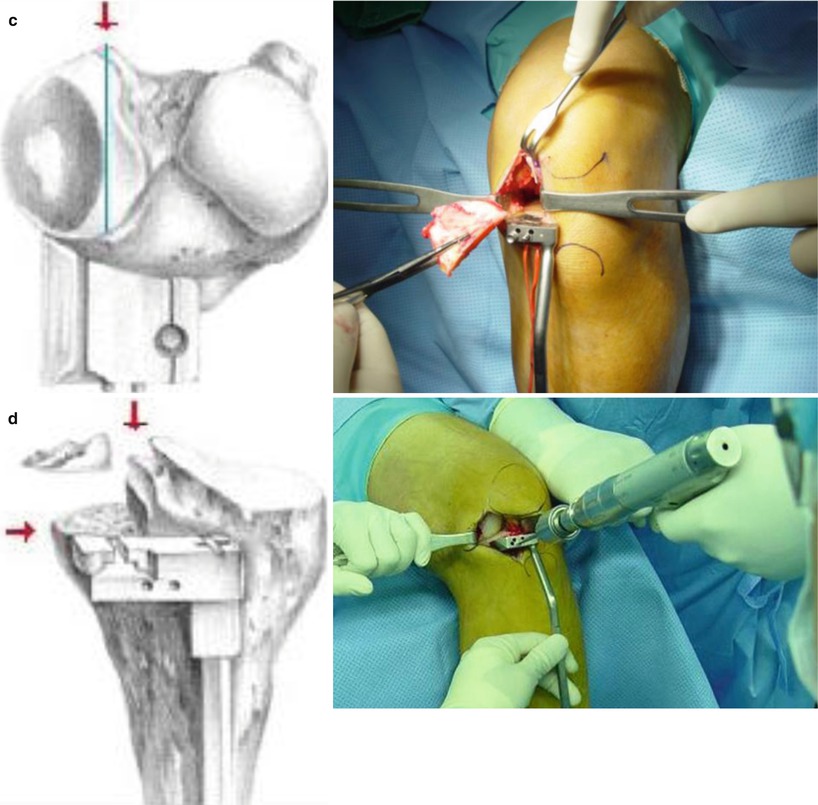
Fig. 6.14




Tibial osteotomy (Courtesy of MH Song/ Biomet, Warsaw, IN). The diagrams of this page show the aligning method (a) and fixation of cutting guide (b). The left diagrams of next page show the overview of tibial osteotomy (c, d). The right photograph shows the operative procedure of osteotomy for the alignment and tibial osteotomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








