Shoulder pain in the throwing athlete can present at any age and in any level of sport and can lead to dysfunction. A thorough evaluation of the throwing athlete can often determine the cause of symptoms, which is frequently multifactorial. Although the pathophysiology leading to pain in the shoulder of the throwing athlete is not entirely known, nonoperative modalities remain the mainstay of treatment. In general, surgical intervention should be reserved as a last resort. Effective treatment often requires collaboration among trainers, players, physicians, and therapists to determine an appropriate course of action.
Key points
- •
Evaluation of the throwing athlete requires the ability to perform a thorough physical examination of the shoulder.
- •
The most common adaptive changes seen in the shoulder of overhead athletes include loss of shoulder rotation, a protracted position of the scapula, and relative weakness of external rotation.
- •
The most common arthroscopic findings in throwing athletes are superior labrum anterior posterior tears (SLAP lesions) and partial-thickness tears of the rotator cuff.
- •
Despite increased knowledge about the throwing shoulder, the cause of what generates pain is poorly understood.
- •
The major indication for surgical intervention is failure of nonoperative treatment.
Introduction
Shoulder pain in the throwing athlete can often be a challenge to manage, for a variety of reasons: (1) the pain typically occurs without trauma, and the mechanism is typically some obscure overuse; (2) a variety of conditions can contribute to the pain, but the cause remains unknown, (3) the treatment of pain in the throwing shoulder remains one of the most challenging tasks of the sports medicine physician; and (4) the amount of stress placed on the shoulder of the throwing athlete is high, and the results of treatment are not as predictable as the patient, family, trainer, coach, and doctor would like to think.
Most of the current literature on the throwing athlete focuses on the baseball pitcher, but much of the information can be applied to players of other sports that require rapid acceleration and deceleration of the upper extremity, such as tennis, softball, javelin, handball, water polo, and so forth. The primary scope of this article is to focus on understanding and evaluating shoulder pain in the throwing athlete. Specifically, we review (1) the biomechanical reasons that the throwing motion is so deleterious to the shoulder, (2) the historical and physical examination findings that help in the assessment, (3) the role of imaging in the evaluation of the shoulder of the throwing athlete, and (4) the treatment of these injuries. Although knowledge about these injuries continues to evolve, the results of treatment have come under increasing scrutiny with regard to returning athletes to participation in their sports.
Introduction
Shoulder pain in the throwing athlete can often be a challenge to manage, for a variety of reasons: (1) the pain typically occurs without trauma, and the mechanism is typically some obscure overuse; (2) a variety of conditions can contribute to the pain, but the cause remains unknown, (3) the treatment of pain in the throwing shoulder remains one of the most challenging tasks of the sports medicine physician; and (4) the amount of stress placed on the shoulder of the throwing athlete is high, and the results of treatment are not as predictable as the patient, family, trainer, coach, and doctor would like to think.
Most of the current literature on the throwing athlete focuses on the baseball pitcher, but much of the information can be applied to players of other sports that require rapid acceleration and deceleration of the upper extremity, such as tennis, softball, javelin, handball, water polo, and so forth. The primary scope of this article is to focus on understanding and evaluating shoulder pain in the throwing athlete. Specifically, we review (1) the biomechanical reasons that the throwing motion is so deleterious to the shoulder, (2) the historical and physical examination findings that help in the assessment, (3) the role of imaging in the evaluation of the shoulder of the throwing athlete, and (4) the treatment of these injuries. Although knowledge about these injuries continues to evolve, the results of treatment have come under increasing scrutiny with regard to returning athletes to participation in their sports.
Throwing biomechanics
The overhead throwing motion used in baseball generates a large amount of stress on one of the most vulnerable joints in the body. Injuries occur not just from the magnitude of the force but also from the number of repetitions involved. The internal rotation of the humerus during a pitch has been measured as high as 7000° per second. Elite pitchers repeat this high-stress cycle with nearly every throw. After ball release, the cycle must be reversed, and the forward inertia of the arm and body must be slowed to a stop.
The throwing motion is complex and involves using the lower extremities, the core muscles, and the upper extremity to generate the forces necessary to accelerate the ball. There is increasing appreciation that the forces transferred to the arm, which allow it to reach these velocities, are generated in large part by a coordinated transfer of torque from the legs to the trunk and to the distal parts of the extremity. This coordinated torque transfer is commonly referred to as the kinetic chain.
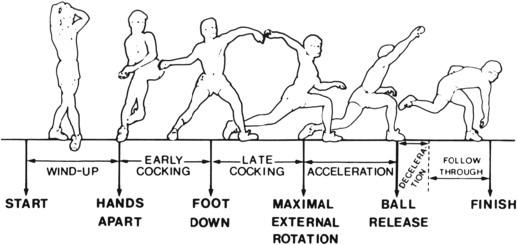
An overhead thrower must be able to have extreme shoulder range of motion (ROM) to assist with acceleration, yet have enough stability in the bony and soft tissues to prevent injury from the high forces generated in the pitching motion. Any disruption in this balance can lead to excess stress on 1 or multiple anatomic structures involved in the kinetic chain. Wilk and colleagues refer to these conflicting demands as the thrower’s paradox. The phases of throwing have been well documented in the literature ( Fig. 1 ). At the transition between late cocking and acceleration, external rotation of the shoulder in relationship to the torso has been reported to reach 165°, whereas normal external rotation in most nonathletes is approximately 90°.
In addition to the high angular velocities mentioned earlier, the magnitude of force across the shoulder during a baseball pitch can be high. An analysis of 40 professional pitchers calculated a 947 N (108% of body weight) distraction force across the shoulder joint. A similar study in collegiate pitchers calculated an average of 81% of body weight distraction force during fastballs. This difference is likely the result of differences in average pitch speed: professional pitchers, 143 km/h (89 mph); college pitchers, 125.5 km/h (78 mph). To counteract these high distraction forces, the deltoid and rotator cuff have been estimated to produce nearly 1090 N of compressive force, 400 N of posterior shear, and 97 N-m of horizontal abduction torque during the deceleration phase. It is postulated that these high forces place stress on the rotator cuff and the supporting structures of the shoulder, especially the superior labrum where the biceps tendon attaches. One theory is that this high distraction force creates shear forces in the rotator cuff tendons, causing them to begin to tear.
Anatomic adaptations
Several anatomic adaptations occur in the shoulder of overhead throwers in response to these high forces. Major changes such as increased musculature in the throwing arm, forward drooping of the shoulder (protracted scapula), and slight asymmetry of the shoulder were first described in tennis players, but they have been noted in athletes who perform overhead sports of any kind. In baseball, they have become common, and seem to be more prevalent in the dominant extremity when overhead throwing is started at a young age. However, it is controversial if these changes are adaptive or maladaptive: some suggest these changes are normal adaptations, whereas others think they can result in injury if not corrected.
Osseous Adaptations in the Humerus
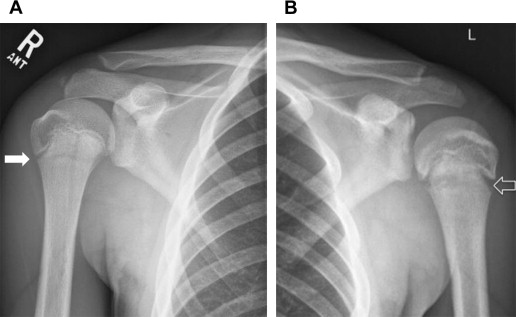
It has been believed that humeral torque in youth baseball pitchers contributes to deformation of the proximal epiphyseal cartilage. This deformation, in combination with repetitive stresses of throwing, has been implicated in the development of proximal humeral retrotorsion or epiphysiolysis (Little League shoulder) ( Fig. 2 ). Statistically significant side-to-side differences of humeral retrotorsion have been measured via ultrasonography in adolescent pitchers. This difference in humeral retrotorsion has also been found in college and professional baseball pitchers. The increased stress on the throwing arm has also been implicated in side-to-side bone mineral density differences in overhead athletes.
Altered proximal humeral anatomy is also believed to contribute to the change of position in the throwing shoulder’s total arc of motion (maximum external rotation to maximum internal rotation with the arm in 90° of abduction). The total arc of motion in most nonathletic individuals ranges from 160° to 180°. In throwing athletes, this arc is shifted posteriorly, allowing more external rotation and decreased internal rotation. This difference in the total arc of motion has been shown in asymptomatic throwing athletes at multiple levels, but it is unknown if it is a normal adaptation or if it is maladaptive.
Capsulolabral Adaptations
The anterior inferior glenohumeral ligament is an important restraint of external rotation with the arm in the throwing position. Adaptations secondary to repetitive stress can lead to lengthening of the capsule and allow increased external rotation. However, the role that this increased external rotation plays in the development of shoulder injuries is not known. Biomechanical studies have shown that the stress of throwing can transmit substantial forces to the biceps attachment at the superior glenoid, and this stress has been postulated as a cause of labral tears in the superior aspect of the shoulder.
Muscular Adaptations
In baseball, muscular adaptations about the shoulder girdle secondary to repetitive throwing and conditioning are more prevalent in pitchers than in position players. Hypertrophy of the muscles can be a normal response to increases in physiologic load, and pitchers can develop loss of external rotation strength. Although the reason for this development is unknown, it has been postulated that the throwing motion may create tension in the infraspinatus branch of the suprascapular nerve, resulting in infraspinatus weakness. Baseball players often have weaker external to internal rotation in their dominant arms compared with their nondominant arms, as measured by isokinetic strength devices. Nevertheless, their dominant arms often have stronger adduction and internal rotation than the opposite extremities.
Diagnostic approach
A painful throwing shoulder can often be confusing and frustrating for the examiner. There are 3 general areas that can contribute to this confusion: anatomy, diagnostic test results, and presenting symptoms. First, there are 4 joints or articulations that comprise the shoulder girdle: the acromioclavicular, sternoclavicular, scapulothoracic, and glenohumeral joints. Dysfunction in any of these structures can affect performance and cause pain. Furthermore, many of the affected structures are deep in the shoulder and difficult to palpate, making it challenging to localize the symptoms. Second, although multiple examination maneuvers are available, they are of varying degrees of helpfulness in determining the source of pain. Indirect examination maneuvers can often be inaccurate and misleading. In addition, multiple tests for specific diagnoses can be positive, because of the difficulty in examining just 1 structure at a time. Third, pain patterns in the shoulder are not specific. For example, an athlete can present with anterior shoulder pain that can result from causes such as rotator cuff tendinosis or partial or complete rotator cuff tears, biceps tendinosis, shoulder instability, frozen shoulder, superior labrum anterior and posterior (SLAP) lesions, or cervical radiculopathy. The other challenge in the examination of the throwing athlete is that although the most common lesions are partial rotator cuff tears or superior labrum tears, there can occasionally be a “zebra”, or uncommon, cause (eg, vascular occlusions, neurologic lesions, and thoracic outlet syndrome ) with a presentation similar to that of the more common conditions. Also, stress fractures of the humerus, glenoid, or scapula, although rare, can present with symptoms similar to those of other more common shoulder conditions and should be considered in the differential diagnosis.
However, a systematic approach, and some experience, can help the clinician become more familiar with which constellation of findings in these athletes is not normal.
Initial Evaluation
As with any complete evaluation, a thorough history of the thrower’s complaints must be the first step. Who was the first person who noticed an issue? Was it the athlete complaining of pain, or was it a coach, trainer, or family member who noticed? Often, the first complaint is a loss of velocity on the pitches or loss of control of the pitches. Occasionally, there is no decrease in performance because some throwers play through the pain. Was there an acute traumatic event or was it insidious in nature? The clinician should also ask if there has been any change in throwing technique or change in mechanics, such as from a change that the players try to initiate or a change that the coaches try to initiate. Irritation of the shoulder occurs commonly when players try a new pitch or if they try to get the shoulder into throwing shape too rapidly, and the development of pain after this typically is a reversible overuse and not supportive of a pathologic lesion. What were the elements of the recent use during sport (eg, pitch counts, frequency of games, and innings per season)? Especially in younger athletes, it is also important to determine if they participate in other sports, concurrently or during different seasons. The examiner must also determine when the throwing athlete has symptoms. For example, does the pain occur when the ball is released or is it more during the late cocking phase? Is the pain located in the front of the shoulder, back, or scapula, and is there any referral down the arm? Pain at night or at rest can be a reason for more concern. Does the thrower have any history of, or does the thrower currently have, instability or a feeling that the shoulder is sliding part of the way out of the socket? When a ball is thrown, is there any popping, catching, clicking, or locking? If there is, is it associated with pain? The examiner must also ask about neurovascular symptoms, including paresthesias, weakness, coldness, swelling of the extremity, and any color changes compared with the opposite side.
In addition to all the pain-specific questions, the clinician should enquire about the history of attempted treatments and any medications used, including performance-enhancing supplements. Often, players take a variety of over-the-counter antiinflammatory agents, and it is important to establish the doses because those too large or too small can have different effects. Any history of injections, rehabilitation protocols, or treatments can be helpful in the evaluation because the success or failure of such treatments can help determine the severity of the injury. Another point to establish is what the thrower’s aspirations and goals are at that time. Is the thrower in high school? Planning on playing in college? Close to the postseason? Typically, 6 to 9 months of recovery are required after surgical procedures around the shoulder, which can affect the decision-making process.
Physical Examination
The shoulder examination varies by individual examiner, and the following is our preferred order for evaluating throwing athletes.
- •
First, inspect the entire shoulder girdle. The clinician must be able to see both shoulders and the upper back. Men must remove their shirts; women should use a sports bra or an examination gown that leaves the shoulders bare ( Fig. 3 ). Any deformity or asymmetry in the shoulder girdle should be noted. Special attention should be paid to atrophy in the periscapular musculature. If the injury is traumatic, the examiner should look for swelling or ecchymosis.

Fig. 3
When examining the shoulders, it is imperative that the patient’s bilateral shoulders are completely visible. Men should not wear a shirt or t-shirt. Women should wear a sports bra or a gown that exposes the shoulders. This photograph shows a patient whose winging was missed because her shoulders were not adequately exposed initially.
- •
Second, evaluate shoulder ROM. It is important to inspect active ROM of both shoulders from in front of and behind the patient. The clinician can evaluate for scapular dyskinesis or asymmetry of scapular motion by viewing the patient from behind as the arm is elevated. ROM in multiple planes should be assessed:
- ○
External rotation with the arm at the side
- ○
External rotation at 90° of abduction
- ○
Active internal rotation up the back and with the arm at 90° of abduction
- ○
Passive evaluation if there is any side-to-side difference or restriction
- ○
- •
Third, compare rotator cuff and other periscapular muscle strength of the affected side with that of the contralateral side.
- •
Fourth, perform distal neurovascular and cervical spine examinations.
- •
Fifth, palpate the bony prominences and soft tissue of the shoulder to determine points of tenderness or crepitus. This procedure is performed before special examinations or provocative maneuvers that might cause the patient discomfort.
Imaging
When evaluating a painful shoulder in an overhead athlete, it is recommended that conventional radiographs be obtained as the initial imaging study. Conventional radiographs are especially helpful in adolescent athletes, who have open growth plates. In this population, the condition known as Little League shoulder shows widening of the growth plate of the proximal humerus compared with the other extremity ( Fig. 2 ). The recommended radiograph series is an anteroposterior view with the shoulder in internal rotation, an anteroposterior view with the arm in external rotation (also called a Grashey view or true anteroposterior view of the shoulder), and an axillary view. A scapular Y view offers little important information and is no longer recommended.
If the conventional radiographs are normal and further evaluation is considered important, then, the next best imaging study is magnetic resonance arthrography with gadolinium. Studies have shown that this imaging study has better sensitivity and specificity for labrum lesion and partial tears of the rotator cuff than magnetic resonance imaging without arthrography. The presence of lesions does not necessarily mean a surgical procedure is necessary; SLAP tears or partial rotator cuff tears are often detected in asymptomatic shoulders.
Ultrasonography can be a good screening test for rotator cuff conditions, but it may not be as useful for detecting superior labrum disease. Although ultrasonography is helpful at delineating biceps disease, isolated biceps tendon issues beyond the confines of the joint (ie, in the bicipital groove) are unusual in throwing athletes.
Common conditions
Glenohumeral Internal Rotation Deficit
Description
Posterior capsular tightness is believed to be a contributor to internal derangements of the shoulder in the throwing shoulder. The large distraction force during follow-through has been implicated in the development of posterior capsular contractures. When the posterior capsule is contracted, there may be a tendency to shift the head superiorly and posteriorly. Internal and external rotation is typically measured with the patient supine. The examiner stabilizes the scapula to prevent scapulothoracic motion, bilateral glenohumeral motion alone is measured ( Fig. 4 ) with a hand-held goniometer, and the measurements are compared. Typically, the throwing shoulder has greater external rotation and less internal rotation than the nonthrowing shoulder. Although there is some controversy about the degree of loss of internal rotation that defines glenohumeral internal rotation deficit (GIRD), the most commonly quoted criterion is more than 20° of loss of internal rotation, or less than 10% of the total ROM, of the contralateral arm.

The mainstay of treatment of GIRD is initial posterior capsular stretches, known as sleeper stretches ( Fig. 5 ), which alone have been reported to provide a more than 90% success rate for symptomatic players with GIRD. If the nonoperative management fails, the athlete may need referral to a surgeon for selective capsular release. However, to our knowledge, the success of a surgical approach to this problem has not been reported, and this treatment remains controversial.
Examination
The technique described earlier should be used. Typically, the athletic trainer or the physical therapist makes these measurements, but it is best if the individual who makes the first measurements also makes each subsequent measurement to minimize interobserver error. The accuracy of measuring shoulder ROM with goniometers has an intraobserver reliability of 87% to 99% but a lower interobserver reliability rate (horizontal abduction, adduction, extension, and internal rotation: 26% to 55%; flexion, abduction, and external rotation: 84% to 90%). However, these measurements are likely accurate only to within 5°, even with a goniometer. Throwing athletes should have screening for GIRD before the start of the season and be reevaluated if they develop any pain or issues throughout the course of the season.
SLAP Lesions
Description
The amount of literature addressing SLAP lesions in the overhead throwing athlete is substantial. This lesion, in which the biceps attachments to the bone (superior glenoid tubercle) and to the superior labrum are disrupted, is one of the most common in overhead athletes. The athlete often reports a loss of throwing velocity and pain in the shoulder. The attachment of the biceps tendon is primarily to the bone of the superior glenoid tubercle just above the glenoid rim. The remaining portion of the biceps tendon splays out anteriorly and posteriorly and is continuous with the superior labrum, which is attached to the glenoid along its periphery ( Fig. 6 ). The definition of what is a SLAP lesion may vary from surgeon to surgeon, but there is some evidence that experienced surgeons can agree on whether a SLAP lesion is or is not present.
Pathophysiology
There is controversy about the cause of superior labrum lesions seen in overhead athletes. The superior labrum and biceps anchor are subjected to a high compressive force when the arm is in maximum abduction and external rotation during the throwing motion, and some clinicians think that the labrum is physiologically impinged between the humeral head and the glenoid at this point of the throwing motion, which has been called internal impingement. However, the highest distraction forces on the biceps tendon and superior labrum occur at ball release and follow-through. It is not known which of these forces creates SLAP lesions, but they are common in the throwing shoulder.
Examination
The literature describes multiple examination maneuvers for the diagnosis of SLAP lesions, but the clinical usefulness of these tests remains controversial. Many of the tests were derived with the concept that the labrum functioned similarly to a meniscus in a knee. Some tests describe a positive result with a click during the examination maneuver, but clicks have been described in 5% of patients with and without SLAP lesions. Despite this finding, 1 study suggested that the presence of a click or a pop increased the accuracy of the examination maneuvers for labral tears, but that study did not restrict the labrum tears to SLAP lesions only.
The active compression (O’Brien) test is one of the more commonly used tests for evaluating SLAP lesions. Although it is a popular test, studies have shown that its sensitivity and specificity for SLAP lesions are modest at best and cannot be relied on to make the diagnosis. The test is performed with the patient standing and in 90° of forward elevation with the arm adducted 10° across the body ( Fig. 7 ). For part 1 of the test, the elbow is in a position of maximal extension and the thumb should point down. The examiner applies a downward inferior force, and the patient is asked to resist this force. If the patient has pain with this maneuver, the location of the pain for a SLAP lesion should be deep in the shoulder. Care should be taken to ascertain the location of the pain, because this test is positive for multiple conditions, especially in patients with acromioclavicular joint disease. For part 2 of the test, the patient has the arm in the same position but the palm is turned up and the maneuver is repeated. The production of pain in the palm-up position than in the thumb-down position is a positive test for a SLAP lesion. The presence of a painful click with the thumb down but not with the palm up is also considered a positive test. This test has been extensively studied and has been shown not to be highly accurate for SLAP tears.
Another test, which is also controversial, is the dynamic shear test. This test is performed with the examiner behind a standing patient and the patient’s arm in abduction and external rotation ( Fig. 8 ). The examiner elevates the arm between 70° and 120° while pushing the humeral head anteriorly. A positive test is achieved when the patient reports pain in the posterior and superior shoulder in this ROM. One study suggested that a slightly modified version of this test had a likelihood ratio of 30 and was an excellent test for making the diagnosis of SLAP lesions. However, another study found that it was not effective in making that diagnosis. This test should be used with caution in patients who might have shoulder instability, because it could potentially dislocate the shoulder.
Several studies have shown that no single physical examination maneuver is sensitive and specific for SLAP lesions. Multiple examination techniques may increase diagnostic accuracy in the office. As mentioned earlier in the section on imaging, MR arthrography can be helpful in identifying labral disease. The most reliable way to diagnose a SLAP lesion is with a diagnostic arthroscopy, but this procedure should be reserved for patients who have undergone appropriate rehabilitation unsuccessfully and continue to be symptomatic.
Prognosis
The best treatment of SLAP lesions remains unknown. Nonoperative treatment with rest, frequent icing, nonsteroidal antiinflammatory drugs, and addressing GIRD or scapular imbalances are accepted treatments. When nonoperative treatment fails, the consensus is that operative intervention should be considered. Failure of nonoperative treatment can be defined as the inability to return to the previous level of play and a strong suspicion that the SLAP tear is responsible for the athlete’s symptoms. Although initial reports with repair of the most common SLAP lesions (type II) found that up to 87% of athletes with repair of a type II SLAP lesion return to play, more recent studies have not proved those results to be accurate. A recent meta-analysis concluded that the results of type II SLAP repair in the subset of overhead athletes are inconclusive and different from those for nonoverhead athletes.
Rotator Cuff Lesions
Description
Rotator cuff disease, a frequent occurrence in the symptomatic throwing athlete, includes painful rotator cuff tendinosis, a partial rotator cuff tear, and (less commonly) a full-thickness rotator cuff tear. Night pain can also be a common finding when the shoulder is inflamed, and when severe, the pain may refer down to the elbow or hand. A common site of rotator cuff disease in the throwing athlete is the posterior half of the supraspinatus and anterosuperior half of the infraspinatus. In the case of a partial-thickness tear, rest, rehabilitation, and consideration of a shoulder injection can be helpful. Although a discussion of biologics such as platelet-rich plasma is beyond the scope of this article, they can be considered in lieu of corticosteroids in the presence of tendinosis or tears. More high-quality studies are needed to determine its efficacy. If nonoperative treatment of partial tears fails, operative repair is an option; it may have a success rate as high as an 89% return-to-play rate in college and professional throwers. However, operative intervention for full-thickness rotator cuff tears in throwing athletes does not have as good a prognosis. Mazoue and Andrews reported that only 1 of 12 (8%) professional baseball players who had repair of a full-thickness rotator cuff tear were able to return to the same level of competition.
Examination
Testing for the rotator cuff can be categorized into strength testing and impingement testing. The supraspinatus muscle is most effectively tested by what is called the Jobe test. It is performed with the patient’s arm elevated to 90° of abduction in the scapular plane ( Fig. 9 ). The examiner then provides an inferiorly directed force against patient resistance. The initial report by Jobe and Moynes suggested that the best position for testing was with the thumb down, but it can often be painful for patients. Subsequent study has shown that the Jobe test can be performed with the thumb up or in a neutral position.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






