, Antonio Cesarani2 and Guido Brugnoni3
(1)
“Don Carlo Gnocchi” Foundation, Milano, Italy
(2)
UOC Audiologia Dip. Scienze Cliniche e Comunità, Università degli Studi di Milano, Milano, Italy
(3)
Istituto Auxologico Italiano, Milano, Italy
Abstract
Vestibular unilateral hypofunction is a consequence of the primary damage to the vestibular structures. Incorrect or incomplete compensation can cause secondary and tertiary damages. Natural compensatory phenomena require, without any kind of treatment, a period ranging from 6 to 8 months to reach a good functional recovery. Rehabilitation is the specific treatment of unilateral vestibular hypofunction. In fact, in all these cases with unilateral hypofunction, only the phenomena of the central regulation – the compensation – are able to render these patients free from symptoms and to manage their impairment, avoiding disability. The key impairment is due to head dynamic unsteadiness, postural instability and dynamic disequilibrium with fear of new vertigo attacks. Treatment must be pointed to (1) increase extensor tone on the affected side; (2) increase antigravitary paravertebral tone; (3) restore correct ankle–hip strategies dynamic; (4) restore control of head stabilization during movement; (5) restore eye–head coordination; (6) avoid disorientation and transition to phobic postural vertigo.
Vestibular unilateral hypofunction is a consequence of the primary damage to the vestibular structures. Incorrect or incomplete compensation can cause secondary and tertiary damages. Natural compensatory phenomena require, without any kind of treatment, a period ranging from 6 to 8 months to reach a good functional recovery. This kind of recovery is not always sufficient to allow performing even everyday life activities in a natural, unconscious and easy manner. Some activities are still difficult such as turning the head rapidly or changing positions of the body, and, frequently, transient vertigo attacks and subcontinuos unsteadiness are observed. Even after some years following an acute episode of vertigo, compensation can turn into transient failure and cause vertigo or dizziness or unsteadiness (VDU).
Incomplete vestibular compensation of any kind of vestibular lesion causes impairment of the most common daily life activities in every patient, but, at least in some subjects, chronic VDU may lead to specific disability and handicap. Disability may be correlated to specific job activities but, more generally, chronic VDU may impact on common life activities through disturbances of the vestibulo-perceptual (VP) system. Cortical vestibular networks presumably mediate perception of whole-body motion. As with all psychophysical systems, decisions (“in which direction am I moving?”) are based on the detection of signals (stimuli), such as semicircular canal afferent information, against a background of activity, or noise. As with other psychophysical systems, the VP system has a defined threshold at which a signal becomes recognized relative to the noise level [1, 2]. For the vestibular system, humans possess higher perceptual than VOR thresholds [3]. These higher perceptual thresholds in humans probably reflect the cortical processing of vestibular signals during decision making in direction recognition tasks [4]. Significant cortical changes are observed in patients following acute vestibular lesions [5, 6].
The relationship between vestibular function and feelings of unreality was recognized decades ago, when Schilder emphasized its connection with depersonalization [7]. This tendency for abnormal vestibular stimulation to provoke feelings of unreality has also been found in normal healthy subjects undergoing calorics [8, 9]; furthermore, false perceptions of orientation may be a consequence of vestibular disorders [10]. Cousins et al. [11] in fact, provided the functional evidence that higher-order mechanisms, ultimately involving the cerebral cortex, are engaged early in vestibular compensation and vertigo suppression. They showed that vestibulo-perceptual function is significantly affected by vestibular neuritis: VP thresholds are raised and asymmetrical, whereas VP supra-threshold time constants are shortened but symmetrical. In this way, a bilateral suppression of supra-threshold vestibular perception is obtained; this suppression may act as a protective mechanism against vertigo but lead to chronic impairment and disability sometimes with anxiety, panic attack, depersonalization/derealization until phobic postural vertigo (see Chap. 13) [12]. The disorientation due to deficient sensory integration could contribute to derealization that occurs in vestibular patients because their distorted vestibular signals create a misleading frame of spatial reference which mismatches with the other senses, as proposed by [13].
The perceptual dampening is probably the neurophysio-pathological phenomenon that can lead to the transition that a patient with acute vestibular neuritis underwent to phobic postural vertigo within months after disease onset [14].
The following protocol can be adopted also to treat dizziness in Ménière patients (see Chap. 10) during intercritical period. Vertigo attacks cannot be prevented by rehabilitation but often patients complain both sporadic vertigo attacks and continuous unsteadiness. This condition can be treated as a vestibular unilateral hypofunction.
Rehabilitation is the specific treatment of unilateral vestibular hypofunction. In fact, despite the cause of hypofunction being known, as after the operation of neurinoma, after an attack of neuronitis, in the postcommotional syndrome, or even when viral or vascular aetiology is confirmed, improvement of the dizziness cannot always be obtained by acting upon these etiologic factors or by administration of some symptomatic drugs. In all these cases with unilateral hypofunction, only the phenomena of the central regulation – the compensation – are able to render these patients free from symptoms and to manage their impairment, avoiding disability.
Generally speaking, the key impairment is due to head dynamic unsteadiness, postural instability and dynamic disequilibrium with fear of new vertigo attacks.
Treatment must be pointed to:
1.
Increase extensor tone on the affected side
2.
Increase antigravitary paravertebral tone
3.
Restore correct ankle–hip strategies dynamic
4.
Restore control of head stabilization during movement
5.
Restore eye–head coordination
6.1 Exercises in the Gymnasium
6.1.1 First Week
1.
Relaxation exercises such as control of breathing with improving consciousness of abdomen or thoracic breathing. A simple exercise consists in deep inhalation followed, after few seconds, by a forced exhalation pronouncing the word “one”. This exercise is repeated 8–10 times.
2.
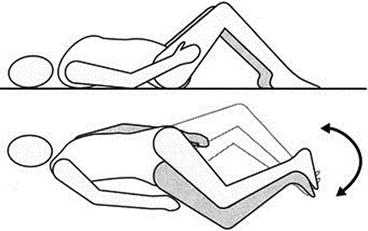
The patient holds her/his right knee against the chest, then she/he extends her/his leg and holds her/his left knee against the chest. When she/he holds the knee against the chest, she/he gently applies traction to the flexed leg with the hands (Fig. 6.1a, b).
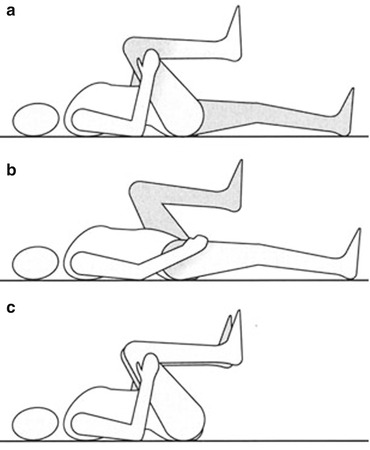
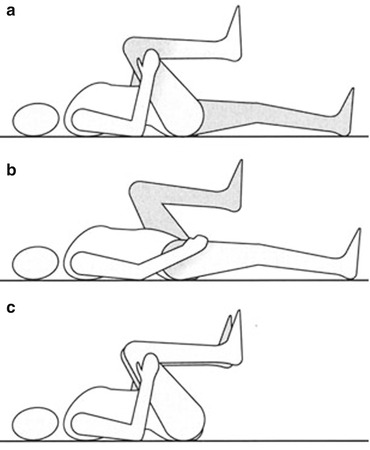
Fig. 6.1
(a–c) Exercises holding the knees against the chest (Originally published in Cesarani and Alpini [15] published by Springer © 1999)
3.
The patient holds her/his two knees to the chest while simultaneously helping, gently, with the hands (Fig. 6.1c).
4.
5.
The patient lifts her/his pelvis while simultaneously holding her/his arms extended over her/his head. She/he then repositions her/his arms along the body while lowering her/his pelvis (Fig. 6.3).
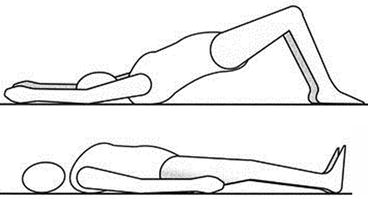
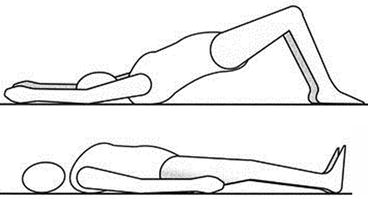
Fig. 6.3
Patient lifts the pelvis and then returns to the supine position (Originally published in Cesarani and Alpini [15] published by Springer © 1999)
6.
In the quadrupedal position, the patient inhales and arches her/his back (hyperkyphosis) while holding her/his head between her/his arms. She/he then exhales, flexing the head and rotating the pelvis in hyperlordosis (Fig. 6.4).
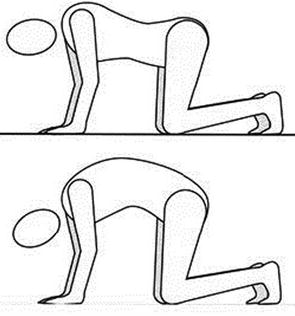
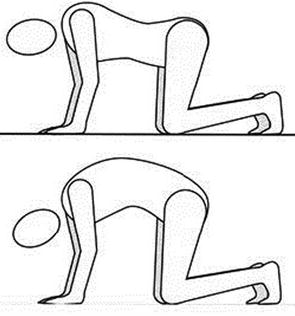
Fig. 6.4
Patient arches the dorsal spine (Originally published in Cesarani and Alpini [15] published by Springer © 1999)
7.
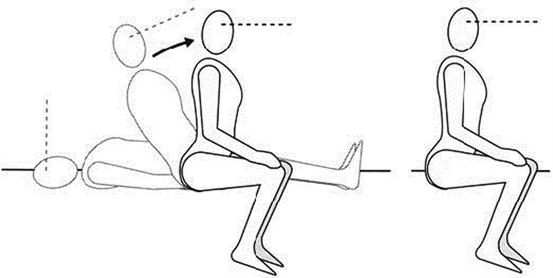
From supine position, the patient passes to the sitting position, fixating a point straight in front of her/him (Fig. 6.5).