Chronic and acute shoulder pain and dysfunction are common complaints among patients. Shoulder pain may be the result of abnormality involving the rotator cuff, subacromial-subdeltoid bursa, biceps tendon, glenoid labrum, glenohumeral joint, acromioclavicular joint, sternoclavicular joint, or glenohumeral joint capsule. Ultrasound-guided (USG) procedures of the shoulder are well established for interventional management. Ultrasound provides the advantages of excellent soft tissue resolution, injection accuracy, low cost, accessibility, portability, lack of ionizing radiation, and the ability to perform real-time image-guided procedures. The purpose of this article is to review common indications and effective techniques for USG injections about the shoulder.
Key points
- •
Diagnosis and treatment of shoulder conditions can prove challenging, and ultrasound allows for precise diagnosis and potential treatment at point of care.
- •
Ultrasound guidance increases accuracy of injections about the shoulder.
- •
A detailed understanding of shoulder anatomy is required for safe and effective ultrasound-guided procedures about the shoulder.
Video content accompanies this article at http://www.pmr.theclinics.com .
Introduction
The shoulder complex is susceptible to a wide range of traumatic and atraumatic pathologic conditions. Secondary to the relatively superficial location of the anatomic structures of the shoulder, many clinicians use ultrasound (US) for diagnostic and interventional purposes about the shoulder. The increased use of US in the last decade is partially attributed to its portability, low cost compared with MRI, lack of ionizing radiation, and potential increased accuracy and efficacy of procedures versus using palpation guidance.
Multiple pathologic processes about the shoulder can be evaluated with US, including subacromial-subdeltoid (SASD) bursopathy, acromioclavicular joint (ACJ) and sternoclavicular joint (SCJ) arthropathy and synovitis, adhesive capsulitis, long head of the biceps brachii (LHBBT) tendinopathy and tenosynovitis, and rotator cuff (RTC) abnormality, including calcific tendinopathy. Both diagnostic and interventional US are operator-dependent modalities. As such, clinical experience and knowledge of anatomy are essential components to a proper diagnosis and accurate procedure.
In this article, an overview, including anatomy, indications, and techniques for common ultrasound-guided (USG) procedures about the shoulder, is provided.
General procedural setup key points
- •
A sterile procedural setup with sterile technique, probe covers, and sterile gel is recommended, but recognize that some clinicians may choose to only sterilize the needle puncture site.
- •
It is important to consider proper ergonomics before performing the procedure, including putting the US machine in front of the practitioner, proper patient positioning, and adjustments to table and chair heights.
- •
After obtaining an optimal preprocedural image of the target, marking the transducer edges with a surgical marking pen is recommended to allow for efficient reacquisition of the target image after sterile preparation. This procedure is especially useful for novice practitioners.
- •
Needle selection may vary per clinician preferences and patient factors. Selection of the smallest-gauge needle with the appropriate length for the desired injection is recommended. The needle gauges mentioned in this article are the authors’ preferences; in general, smaller gauges are more comfortable for the patient and are typically well visualized with US about the shoulder with good technique.
- •
Injection contents and respective amounts will vary between practitioners and depend on the goals of the procedure.
Introduction
The shoulder complex is susceptible to a wide range of traumatic and atraumatic pathologic conditions. Secondary to the relatively superficial location of the anatomic structures of the shoulder, many clinicians use ultrasound (US) for diagnostic and interventional purposes about the shoulder. The increased use of US in the last decade is partially attributed to its portability, low cost compared with MRI, lack of ionizing radiation, and potential increased accuracy and efficacy of procedures versus using palpation guidance.
Multiple pathologic processes about the shoulder can be evaluated with US, including subacromial-subdeltoid (SASD) bursopathy, acromioclavicular joint (ACJ) and sternoclavicular joint (SCJ) arthropathy and synovitis, adhesive capsulitis, long head of the biceps brachii (LHBBT) tendinopathy and tenosynovitis, and rotator cuff (RTC) abnormality, including calcific tendinopathy. Both diagnostic and interventional US are operator-dependent modalities. As such, clinical experience and knowledge of anatomy are essential components to a proper diagnosis and accurate procedure.
In this article, an overview, including anatomy, indications, and techniques for common ultrasound-guided (USG) procedures about the shoulder, is provided.
General procedural setup key points
- •
A sterile procedural setup with sterile technique, probe covers, and sterile gel is recommended, but recognize that some clinicians may choose to only sterilize the needle puncture site.
- •
It is important to consider proper ergonomics before performing the procedure, including putting the US machine in front of the practitioner, proper patient positioning, and adjustments to table and chair heights.
- •
After obtaining an optimal preprocedural image of the target, marking the transducer edges with a surgical marking pen is recommended to allow for efficient reacquisition of the target image after sterile preparation. This procedure is especially useful for novice practitioners.
- •
Needle selection may vary per clinician preferences and patient factors. Selection of the smallest-gauge needle with the appropriate length for the desired injection is recommended. The needle gauges mentioned in this article are the authors’ preferences; in general, smaller gauges are more comfortable for the patient and are typically well visualized with US about the shoulder with good technique.
- •
Injection contents and respective amounts will vary between practitioners and depend on the goals of the procedure.
Subacromial/subdeltoid bursa
The SASD bursa is a potential synovial space that lies deep to the deltoid muscle, acromion, and the coracoacromial ligament, and superficial to the supraspinatus tendon, rotator interval (RI), greater tuberosity, and intertubercular groove. The SASD extends approximately 3 cm lateral over the deltoid shelf of the greater tuberosity of the humerus and is surrounded by peribursal fat, which is sonographically hyperechoic relative to the anechoic bursa. The normal bursa is about 1 mm in thickness and located just deep to the more superficial layer of peribursal fat.
SASD bursopathy, a condition that may be a primary or secondary cause of pain, is the most commonly reported finding on diagnostic US of the painful shoulder. Given its superficial location, the bursa is best visualized using a high-frequency (>10 MHz) linear-array transducer placed long axis to the supraspinatus tendon fibers. Sonographic findings of bursal enlargement with anechoic fluid or soft tissue hypertrophy are common in the setting of bursopathy and may be accompanied by hyperemia on color Doppler. These findings can be confirmed as symptomatic on physical examination with provocative maneuvers, such as the Neer and Hawkins impingement tests, and on dynamic US with painful bunching of the bursa under the acromion as the humerus is abducted.
It has been established that impingement of the SASD bursa can lead to bursopathy, which can be painful and debilitating, especially to patients who perform repetitive overhead activities. SASD bursal injections are commonly used for both diagnostic and therapeutic purposes. Cadaveric studies on palpation-guided (PG) injections report accuracy rates ranging from 29% to 83%. Two studies comparing the accuracy rate of USG injections versus PG injections demonstrated accuracy rates from 65% to 100% when using USG. It has been demonstrated that short- and long-term relief of shoulder pain secondary to subacromial impingement can be gained with SASD bursa injections.
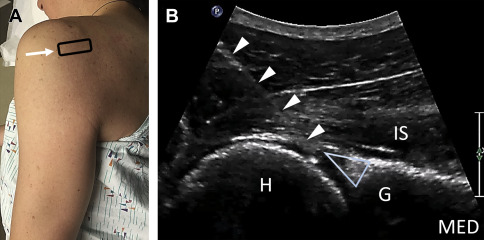
Authors′ preferred technique for ultrasound-guided subacromial-subdeltoid bursa injection
Positioning for the lateral approach to the SASD bursa involves placing the patient in the lateral decubitus position on the contralateral side ( Fig. 1 A ). A high-frequency (>10 MHz) linear-array transducer is placed long axis to the supraspinatus tendon (anatomic coronal plane) to visualize the SASD bursa. Once localized deep to the deltoid and peribursal fat, a 25-gauge 38-mm needle (or in larger patients, a 25-gauge 51-mm needle) is introduced in an in-plane lateral-to-medial fashion under direct USG to anesthetize the skin and needle path into the SASD bursa ( Fig. 1 B). A small amount of lidocaine can be used to confirm flow within the bursa. The syringe is exchanged, and after sonographic confirmation of needle tip placement, the SASD bursa is injected under direct USG with the desired amount of injectate (usually 3–5 mL) ( [CR] ).
Acromioclavicular joint
The ACJ is the articulation between the lateral hyaline-covered clavicle and the medial hyaline-covered acromion. The ACJ has a centrally located fibrocartilaginous disc, which can partially or completely separate the joint into medial and lateral joint cavities. The ACJ is stabilized by several important ligaments. Laterally, the ACJ is stabilized by the inferior and superior ACJ ligaments, the latter of which has contributing fibers from the coracoacromial ligament. Medially, the joint is stabilized by the coracoclavicular ligaments (conoid and trapezoid), which also limit vertical displacement of the clavicle relative to the acromion.
The ACJ is commonly affected by both idiopathic and posttraumatic disorders, and degenerative changes are also a common cause of pain. However, degenerative changes of the ACJ are also frequently seen in asymptomatic individuals over the age of 35 years. Given the high prevalence of ACJ degeneration in asymptomatic individuals, identification of the ACJ as the primary pain generator in individuals with shoulder pain can prove challenging. Physical examination maneuvers, pain referral patterns, and imaging findings have been shown to lack sensitivity and specificity when identifying the ACJ as the primary pain generator.
As a very superficial structure, the ACJ is best visualized using a high-frequency (>10 MHz) linear-array transducer placed long axis (anatomic coronal plane) to the clavicle and acromion. A hypoechoic intra-articular disc may be visualized within the joint as well as up to 3 mm of physiologic anechoic joint capsule distension. Common US findings of abnormality at the ACJ include widening or instability of the joint (ACJ separation), cortical irregularities, joint effusion with synovitis or capsular distension, and possible ganglion cysts ( Fig. 2 B, C ).
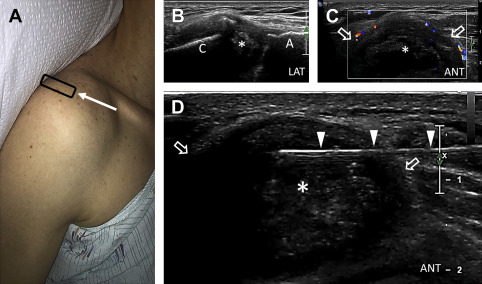
Some investigators have suggested the use of injections to help diagnose and assist in clinical decision-making in patients with apparent ACJ pain. Despite its superficial location, the accuracy of PG ACJ injections has been reportedly low, with accuracy rates ranging from 40% to 72%. Conversely, USG injections have reported accuracy rates of 90% to 100% in both clinical and cadaveric studies.
Authors′ preferred technique for ultrasound-guided acromioclavicular joint injection
For the anterior in-plane approach to the ACJ, the patient is placed in the supine position with a few pillows under the upper back or the head of the examination table elevated ( Fig. 2 A). A high-frequency (>10 MHz) linear-array transducer is placed short axis to the clavicle and moved laterally until the bony acoustic landmarks of the clavicle disappear ( Fig. 2 A, C, D). Once the ACJ is localized using the technique above, a 27-gauge 32-mm needle is introduced in an in-plane anterior-to-posterior fashion under direct USG to anesthetize the skin and needle path into the ACJ (see Fig. 2 D). Following correct placement, the syringe is exchanged, positioning is reconfirmed sonographically, and the ACJ is injected under USG with the desired amount of injectate (usually <1 mL) ( [CR] ). Care must be taken to avoid excess distension of the joint because this can result in pain after the procedure. Given the relatively small size of the joint, clinicians should be cognizant of the procedural goals, whether diagnostic or therapeutic. This injection can also be performed with an out-of-plane approach similar to that described later in the SCJ injection section of this article.
Sternoclavicular joint injections
The SCJ is composed of the hyaline-covered sternal end of the clavicle and the hyaline-covered clavicular notch of the manubrium and first rib, separated by an intra-articular disc. It represents the only articulation between the axial skeleton and the upper limb. The SCJ is stabilized medially by the anterior and posterior sternoclavicular ligaments and laterally by the interclavicular and costoclavicular ligaments. Additional stability is provided by a complete or incomplete intra-articular disc, which is contiguous with both the sternoclavicular and the interclavicular ligaments.
Although uncommon, the SCJ can be a clinically important source of shoulder pain. The SCJ can be affected by both idiopathic and posttraumatic arthritis, dislocation or subluxation, synovitis-acne-pustulosis-hyperostosis-osteitis, avascular necrosis (Friedrich disease), rheumatic arthritis, and crystalline arthropathies. The pain referral pattern for the SCJ is widespread and often nonspecific. Furthermore, degeneration of the SCJ and intra-articular disc is common with advanced aged and often asymptomatic. Therefore, it can be clinically challenging to determine if the SCJ is the primary pain generator in a patient presenting with shoulder or even anterior neck pain.
As another superficial structure, the SCJ is best visualized using a high-frequency (>10 MHz) linear-array transducer placed long axis to the clavicle (short axis to the joint). A hypoechoic intra-articular disc may be visualized within the joint, which can be accentuated by increasing the gain. Common pathologic findings on US evaluation include cortical irregularities, capsular distension, and hyperemia on low-flow color Doppler in the case of synovitis ( Fig. 3 B ).
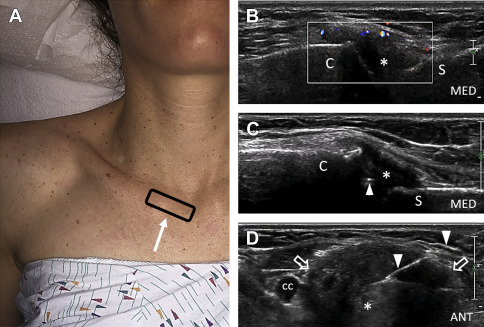
Some clinicians have advocated for the use of diagnostic and therapeutic injections into the SCJ to assist in clinical decision-making and to treat symptomatic patients. PG injections of the SCJ have a reported accuracy rate of 74% to 78%. Clinicians have also used fluoroscopic and computed tomographic guidance for injection and aspiration of the SCJ with reported good clinical outcomes. In one cadaveric study, the USG success rate was 100% using an out-of-plane technique.
Authors′ preferred technique for ultrasound-guided sternoclavicular joint injection
For the anterior out-of-plane approach to the SCJ, the patient is placed in the supine position with a few pillows under the upper back or the head of the bed elevated ( Fig. 3 A). Often, the clavicle at the SCJ lies superficial to the manubrium, creating a step-off that can be used as an anatomic landmark for locating the joint via palpation before transducer placement. A high-frequency (>10 MHz) linear-array transducer is placed long axis to the SCJ, placing the center of the joint in the center of the transducer (see Fig. 3 A). Occasionally, in the setting of severe abnormality, passive shoulder motion may be used to dynamically move the clavicle relative to the manubrium to help identify the joint. Frequently, the joint will become more conspicuous by rotating the transducer slightly clockwise or counterclockwise. Color Doppler can be used to locate the common carotid artery, which lies deep to the SCJ and theoretically could be injured with needle misplacement ( Fig. 3 D). Once the SCJ is localized, a 25- to 27-gauge 25- to 38-mm needle is introduced via an out-of-plane anterior-to-posterior approach under direct USG to anesthetize the skin and needle track ( Fig. 3 C). Before injection, the clinician may rotate the transducer 90° to the long-axis view of the needle to assess depth and positioning (see Fig. 3 D). Following proper placement within the SCJ, the syringe is exchanged; the needle position is sonographically reconfirmed, and the SCJ is injected with the desired amount of injectate (usually <1 mL) ( [CR] ). As with the ACJ injection described previously, care must be taken to avoid overdistension of the joint, and the goals of the injection must be considered because of the relatively small joint space.
Glenohumeral joint
The glenohumeral joint (GHJ) is composed of a hyaline-covered spherical humeral head that articulates with the essentially flat hyaline-covered glenoid fossa. The glenoid labrum, which is composed of fibrocartilage, increases the depth and width of the shallow glenoid fossa as well as GHJ stability. There are several joint recesses associated with the GHJ, including the LHBBT sheath, the axillary recess, and the subscapular recess.
Secondary to its increased range of motion and the relative incongruence between the glenoid fossa and the humeral head, the GHJ is prone to instability and abnormality. The GHJ can be affected posttraumatically as a result of a dislocation or subluxation, with resultant labral injury, or a chronic RTC tear resulting in RTC arthropathy. It can also be affected idiopathically as a result of osteoarthritis or from inflammatory causes, such as rheumatoid arthritis and adhesive capsulitis. Adhesive capsulitis is a common disease process affecting up to 3% to 5% of the population and up to 20% of patients with diabetes. Although the pathophysiology of the disease is not well understood, it is thought to result from an inflammatory condition in the GHJ capsule that eventually results in decreased capsular volume and glenohumeral range of motion.
The GHJ is best visualized via a posterior acoustic window with a low-frequency (<10 MHz) curvilinear-array transducer placed short axis to the joint in the oblique axial plane. Common US findings in patients with GHJ abnormality include cortical irregularities, joint effusions, labral tears, and osteophytes.
In those patients that fail conservative measures, such as physical therapy and oral anti-inflammatory/analgesic medication, intra-articular GHJ injection may be indicated. Multiple publications have demonstrated the accuracy rate of PG GHJ injections, ranging between 50% and 96% in the cadaveric setting and 10% and 100% in the clinical setting. The PG anterior approach was generally found to be more accurate than the posterior approach. Both the anterior and the posterior USG approaches are well-described, with reported accuracy rates of 93% in a cadaveric model and 97% to 100% in a clinical setting. There is emerging evidence in favor of the anterior approach at the RI for the treatment of adhesive capsulitis, with higher rates of capsular distension on magnetic resonance arthrography.
Authors′ preferred technique for ultrasound-guided glenohumeral joint injection
Posterior Approach
For the posterior in-plane injection of the GHJ, the patient is positioned side-lying with the affected limb up, occasionally with a bolster under the arm for comfort ( Fig. 4 A ). A low-frequency (<10 MHz) curvilinear-array transducer is placed long axis to the fibers of the infraspinatus in the anatomic axial oblique plane to the GHJ (see Fig. 4 A). Occasionally in the setting of severe abnormality, passive shoulder motion may be used to dynamically move the humerus relative to the glenoid to make the joint space more conspicuous. A 22- to 25-gauge 51- to 64-mm needle is introduced via an in-plane posterolateral approach under direct USG to anesthetize the skin and needle track into the GHJ ( Fig. 4 B). Care should be taken to avoid puncture of the glenoid labrum during the procedure, because this can be painful. After obtaining proper positioning, the syringe is exchanged; position is reconfirmed, and the GHJ is then injected with the desired amount of injectate (usually 4–5 mL) ( [CR] ).