Ulnar Collateral Ligament Reconstruction
Introduction
Ulnar Collateral Ligament Anatomy
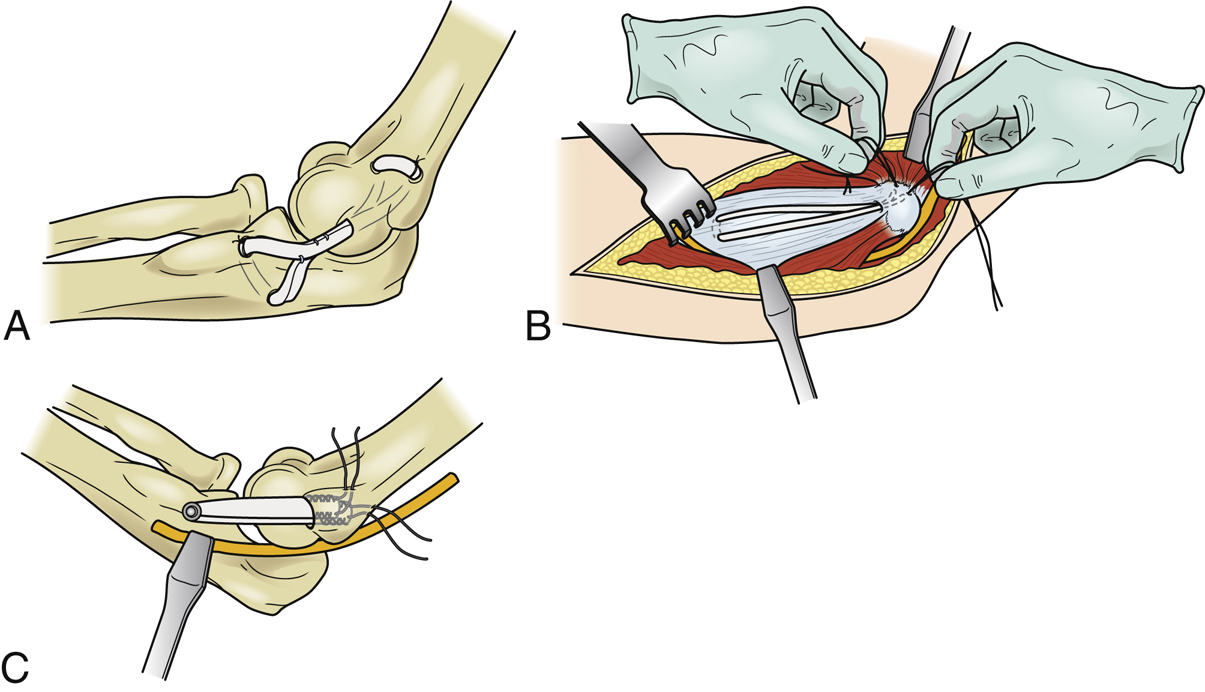
Figure 1Illustrations show elbow ulnar collateral ligament reconstruction techniques. A, The figure-of-8 graft configuration as described by Jobe et al. B, Graft configuration using the docking technique. C, A hybrid technique of interference screw fixation on the ulna and the docking technique in the humerus, also referred to as the DANE TJ technique.
The UCL originates at the inferior surface of the medial epicondyle of the humerus and inserts onto the sublime tubercle of ulna
History of UCL Reconstruction (Figure 1)
The Jobe technique returned athletes to their previous level of play; as originally described, it involved the submuscular transposition of the ulnar nerve, elevation of the flexor-pronator mass to expose the tunnel sites, and figure-of-8 graft configuration through a tunnel on the ulnar side and three large holes in the medial epicondyle
Author preference is the docking technique, a muscle-splitting approach using a single bony tunnel with two small converging holes, which simplifies graft tensioning and reduces the risk of medial epicondyle fractures
| Video 9.1 Ulnar Collateral Ligament Reconstruction Using the Docking Technique. Joshua S. Dines, MD; David W. Altcheck, MD (5 min) |
An alternate hybrid technique is called the DANE TJ technique
Patient Selection
Indications
Medial-side elbow pain with UCL insufficiency that prevents patient from competing at the normal level
During history, examiner must ask about the location of pain and presence of ulnar nerve symptoms
Radiographs may show calcification in ligament, bone spurs, or avulsion fractures
MRI can confirm UCL insufficiency and identify associated injuries, including flexor-pronator tears, loose bodies, and cartilage injury
Contraindications
The use of biologics to augment conservative treatment has improved outcomes, particularly in partial tears
Athlete with no plans or options to continue playing the same sport
Patient who is unwilling or unable to complete a lengthy rehabilitation
Procedure
Preoperative Planning
Determine type of graft
Most common are the gracilis and palmaris longus tendons
Less common are the split flexor carpi radialis, toe extensor, and plantaris tendon
Arthroscopy should be used in patients with preoperative physical and imaging findings consistent with valgus extension overload
Ulnar nerve transposition is not indicated unless persistent preoperative paresthesias, motor symptoms, or nerve subluxation are present
Patient Positioning/Special Equipment
Supine position with arm draped free on arm board
Equipment includes a nonsterile tourniquet, No. 1 nonabsorbable suture, suture shuttle, and 1.5-mm, 3.5-mm, 4-mm, and 4.5-mm burrs; if a fracture of the sublime tubercle is present or in revision cases, a Bio-Tenodesis screw (Arthrex) or EndoButton (Smith & Nephew) may be required for graft fixation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


