Trocanteric Approaches for Primary THA
Nicholas Frisch
Craig D. Silverton
Total hip arthroplasty (THA) remains one of the most successful surgical procedures performed worldwide and the rate rises annually. Between 1990 and 2002 the rate of primary THA per 100,000 persons increased by 46% while the rate of revision THA increased by 60% (1). The demand for THA continues to increase and by 2030 the demand for primary THA has been projected to grow by 174% to 572,000 procedures annually compared to only 208,600 in 2005. The demand for revision THA has similarly been projected to grow by 673%, from 450,000 procedures in 2005 to 3.48 million by 2030 (2). As the demand increases and a growing number of patients undergo primary THA, it is clear that there will be an ever increasing number of revision procedures as well.
The use of trochanteric osteotomy has been a longstanding technique used to enhance the exposure of the hip joint. In the difficult primary total hip and revision hip cases, it provides relatively easy circumferential exposure of the hip joint; minimizes surgical time and decreases soft tissue trauma.
B.M. Wroblewski, a true disciple of Sir John Charnley, performs a trochanteric osteotomy on all primary hip replacements. This allows for an enhanced approach and higher likelihood of success in even the most difficult primary and revision cases. While this may be the case for a surgeon experienced in the use of trochanteric osteotomy, nonunion rates are typically two to three times higher for those surgeons without the experience. It is for this reason that it is important to understand when to use a trochanteric osteotomy, which technique is most appropriate for the specific patient, and how to ensure postoperative stability while minimizing complications.
Indications and Contraindications
According to Sir John Charnley, who was taught the method of trochanteric osteotomy by Sir Harry Platt, “If it could be guaranteed that the greater trochanter would unite within 3 weeks when reattached, and without imposing restrictions which would impede rehabilitation, few surgeons would fail to avail themselves of the easy and beautiful access to the hip joint provided by the lateral [transtrochanteric] approach” (3). Indeed, Charnley repeatedly emphasized the importance of using a technique that would provide appropriate exposure to prepare the bone and the importance of implanting the components in a way that could be easily accomplished by other surgeons. Few would deny that trochanteric osteotomy still provides the most extensile exposure of the hip joint.
There are a wide variety of indications for using a trochanteric osteotomy based on the surgeon’s ability and need to gain adequate access to the hip joint. Contemporary primary THA is typically approached through a minimally invasive anterior, posterior, or a modification of the direct lateral approach (Hardinge) (4). In a patient with an ankylosed hip, severe protrusion acetabuli, massive periarticular scar or heterotopic ossification (HO), internal or external rotation may not be possible. The use of a minimally invasive technique in these cases can be frustrating and result in a catastrophic spiral fracture of the femur. Trochanteric osteotomy in these cases gives the surgeon adequate exposure of the hip joint so that a complete capsulectomy can be performed and adequate exposure of the proximal femur is achievable. Patients with congenital dislocation of the hip and acetabular dysplasia may require trochanteric osteotomy for a complete exposure and lengthening of the shortened femur.
Deformities of the proximal femur and trochanter may be congenital, developmental, posttraumatic, or secondary to primary bone diseases such as Paget disease or fibrous dysplasia. Previous intertrochanteric or subtrochanteric fractures with malunion and rotatory deformity can make a standard exposure difficult, as can a previous arthrodesis or limited range of motion in the ipsilateral knee. Trochanteric osteotomy will greatly facilitate exposure and assists in proper orientation of the femoral component in these cases.
The primary indication for trochanteric osteotomy remains revision hip arthroplasty, where adequate exposure of the acetabulum and proximal femur frequently cannot be achieved with standard approaches. Performing any revision surgery without adequate exposure risks injury to the sciatic nerve, iatrogenic femur fracture, or avulsion of the abductors. In addition,
malposition of the components with eccentric reaming of the femoral canal is a common complication resulting in distal femoral perforation.
malposition of the components with eccentric reaming of the femoral canal is a common complication resulting in distal femoral perforation.
Although the advantages of trochanteric osteotomy in difficult primary THA and in revision cases are numerous, nonunion or malunion of the trochanter remains a challenge and unfortunately is the most common complication. Trochanteric osteotomy is therefore contraindicated in patients with inadequate bone stock and deficiency in the trochanter bed that would make reapproximation of the trochanteric fragment not possible. Similarly, in any patient who has had radiation to the site or who is at high risk for HO and may require radiation postoperatively, trochanteric osteotomy would be relatively contraindicated. Finally, cementless ingrowth prostheses that require large metaphyseal filling and leave only a thin shell of bone in the trochanteric area after broaching may be contraindicated.
Trochanteric Osteotomy Techniques
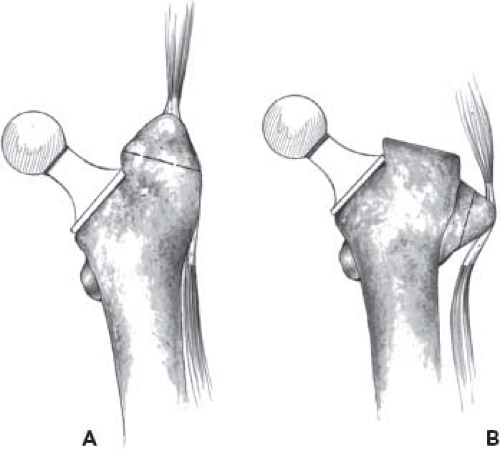
The classic trochanteric osteotomy as initially recommended by Charnley still provides the best access to the difficult primary or revision hip. A flat cut was made across the trochanter and retracted proximal, exposing the hip joint. The trochanteric fragment was then lateralized and placed distal to its original bed. This technique allowed several advantages, including the use of a short-necked prosthesis that decreased the lever arm of the femoral neck and transmitted forces to the upper shaft of the femur while allowing the abductors to be properly tensioned, potentially reducing the incidence of postoperative dislocation (3).
We will describe the classic osteotomy popularized by Charnley, followed by several alternative osteotomy approaches that can be utilized as needed for a variety of surgical indications.
Chevron Trochanteric Osteotomy
Charnley described a classic trochanteric osteotomy that was a flat cut; then transferred distally and secured in place. It did not take long for surgeons to recognize the inherent instability of a flat-cut trochanteric osteotomy and in 1954 a pair of French surgeons Debeyre and Duliveux began using what the Swiss popularized as a “dihedral self-stabilizing” osteotomy (5,6,7). There are several obvious advantages to this: (1) enhanced rotational stability, (2) increased
bone contact area, and (3) easier anatomic replacement of the trochanter.
bone contact area, and (3) easier anatomic replacement of the trochanter.
Weber (6) compared a group of 138 patients, of whom 69 had conventional flat osteotomies and 69 underwent a biplane (chevron) osteotomy. He found a pseudoarthrosis rate of 11% in the conventional group compared to a rate of 1.5% in the biplane group. Berry and Müller (8) reported on 53 primary total hip arthroplasties and 74 revisions utilizing this chevron osteotomy with single-wire fixation and noted rates of trochanteric union of 98% and 97% respectively. Wroblewski and Shelley (9) reported an equally excellent 98% union rate in 222 arthroplasties of which 50% were revisions.
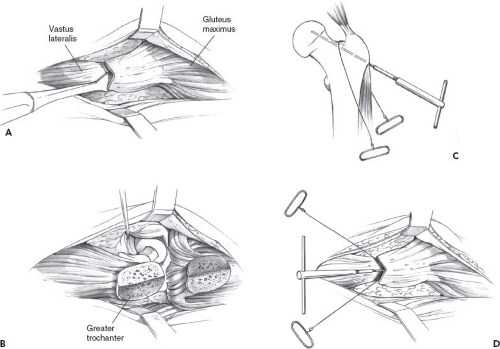
Technique: The chevron (biplane) osteotomy begins with a standard posterior or lateral incision. The external rotators are tagged and retracted posteriorly, protecting the sciatic nerve. The osteotomy is planned 4 to 5 cm distal to the proximal tip of the greater trochanter and the vastus lateralis origin is divided approximately 1 cm distal to its insertion to allow a cuff of tissue to remain for a repair. The anterior and posterior limbs of the osteotomy are equal in size and are cut at an angle of about 30 degrees from the parasagittal plane, forming a biplanar surface that is convex laterally. This cut can be made with an oscillating saw or a straight osteotome (Fig. 6.1A,B). Special chevron-shaped osteotomes are popular with surgeons who routinely use this approach (10). Another option is to pass a 4-mm smooth Steinmann pin into the center of the trochanter, starting just below the vastus ridge and directing it at about 45 degrees to the shaft of the femur (9). A Gigli saw is then passed into the notch between the superior aspect of the femoral neck and the trochanter. The saw lies proximal to the Steinmann pin and is directed distally, cutting anteriorly and posteriorly, creating a two-plane osteotomy (Fig. 6.1C,D). Regardless of the technique used to make the cut, the resulting configuration resembles the roof of a Swiss chalet. The fragment can now be retracted cephalad and held with retractors or Steinmann pins. Without the trochanter in place for tensioning of the abductors, extensive leg lengthening can occur and must be considered.
Reattachment of the trochanteric fragment can be accomplished using a variety of techniques, most commonly with wires or cables. Although each type of fixation offers a slightly different set of advantages and disadvantages that will be discussed later, it appears that the self-stabilizing effect of this dihedral osteotomy is actually the key to successful fixation. However, in the case of revision THA the self-stabilizing effect may be negated in the presence of a poor trochanteric bed or substantial bone loss. As such, additional fixation techniques may then be required.
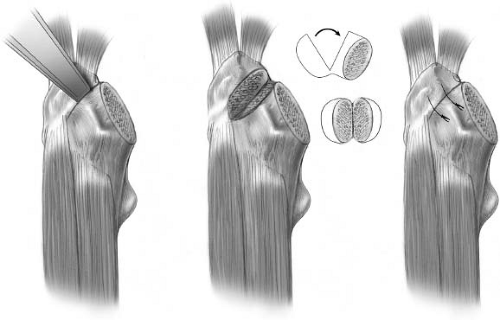
Trochanteric Slide
The technique now known as the trochanteric slide was first described by English in 1975 (11). Dissatisfied with the classic techniques of trochanteric detachment used by Ollier and Charnley, English et al. (12,13) developed a new method of trochanter detachment in an attempt to convert the tensile forces placed across the detached fragment of bone into compressive forces (Fig. 6.2). McFarland and Osborne (1954) were the first to describe keeping the tendinous portions of the gluteus medius and vastus lateralis intact during a posterior exposure of the hip (14). They did not osteotomize the trochanter but instead peeled the insertions of the gluteus medius and vastus lateralis off with a sharp chisel or knife (Fig. 6.3A,B). English modified McFarland’s technique so that a part of the origin of the vastus lateralis muscle remained attached to the trochanteric fragment. Leaving the gluteal and vastus muscle attachments in combination with the short external rotators, English felt this musculotendinous sleeve would create a compressive force on the osteotomy site, preventing migration and encouraging rapid union (Fig. 6.2). After the osteotomy, the detached fragment is turned on edge and held forward and the hip is dislocated in a posterior direction. In his report on 222 primary arthroplasties, of which 120 involved standard wire techniques for reattachment of the trochanter and 102 involved a bolt and bone graft, English (11) reported that the rates of nonunion were 4.3% and 2.5%, respectively.
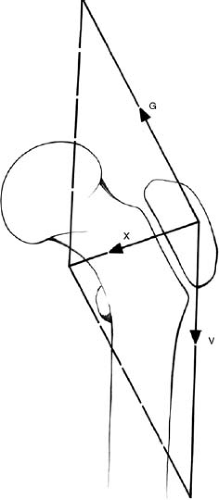 Figure 6.2. Leaving the gluteal (G) and vastus (V) muscles attached produces a medial component (X) that exerts a compressive force on the plane of osteotomy (English). |
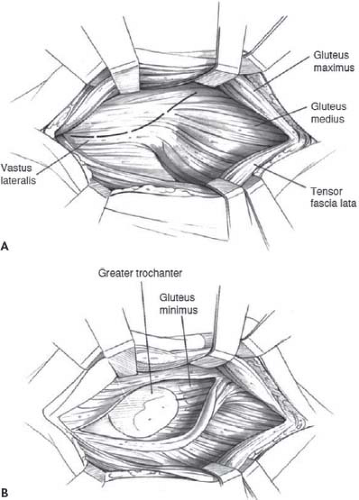 Figure 6.3. A,B: Posterior exposure of the hip joint, keeping the tendinous portions of the gluteus medius and vastus lateralis intact (McFarland). |
Fulkerson et al. modified this technique slightly by reflecting the gluteus medius and minimus laterally while developing a plane between these two muscles and the anterior head of the origin of the vastus lateralis (Fig. 6.4) (15). The osteotomy is then made from this anterior approach, keeping the gluteal and vastus muscles attached to the trochanter
along with the short external rotators. The authors felt that retracting the trochanteric fragment and its attached muscles posteriorly instead of anteriorly, as described by English, allowed the femoral canal to be approached more easily and accurately.
along with the short external rotators. The authors felt that retracting the trochanteric fragment and its attached muscles posteriorly instead of anteriorly, as described by English, allowed the femoral canal to be approached more easily and accurately.
As the need for greater exposure during revision hip surgery increased in the 1980s techniques for facilitating improved exposures began to emerge. Glassman et al. (16) described the sliding trochanteric osteotomy or anterior trochanteric slide. This technique is similar to the original description by English, but the external rotators are divided close to their insertion and preserved for reattachment after reapproximation of the trochanter. Glassman et al. originally reported on 90 hip arthroplasties, 88 of which were revisions, and noted a 10% nonunion rate. Seven hips had wire breakage and an abductor lurch was seen in 28%. There were no early or late dislocations after a mean follow-up of 21 months. A more recent report by Glassman et al. of 129 revision procedures in which a sliding trochanteric osteotomy was utilized, they noted a nonunion rate of 14%, a 21% incidence of broken wires, a 5% rate of postoperative dislocation, and a persistent abductor lurch in 19% of patients (17).
Using the same technique as Glassman, Lindgen and Svenson noted a 2% incidence of nonunion and only one case of a postoperative dislocation in 189 total hip arthroplasties (39 revisions) (18). Romero and associates performed a study on 22 consecutive revision operations using this anterior trochanteric slide osteotomy and found that abductor moment arm and muscle length were increased significantly, improving abductor biomechanics (19). The improved biomechanics acted to protect against trochanteric migration. A modified anterior trochanteric slide osteotomy suggested by Ackerman and Trousdale, creates a triplanar osteotomy which leaves an anterior vertical ridge of bone intact that resists the anterior forces on the osteotomy. The authors believe that this modification will allow for enhanced inherent stability and a decreased rate of nonunion (20).
Another modification of the trochanteric slide involves a step cut to prevent migration and limit motion at the osteotomy side. Leunig et al. compared a standard flat-cut slide osteotomy to a new variation called the step-cut osteotomy. Utilizing composite bones and cadaveric specimens, they found the trochanteric step osteotomy to be a more stable construct and theoretically could decrease the rate of nonunion and postoperative reduced weight-bearing period (21).
The striking advantage of this technique over the classic Charnley trochanteric osteotomy is the continuity of the vastus with the gluteus medius and the prevention of the migration of the trochanteric fragment.
Technique
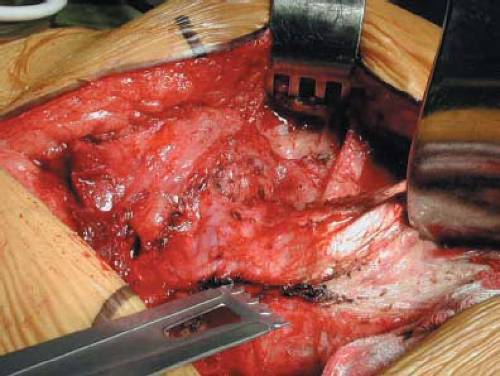
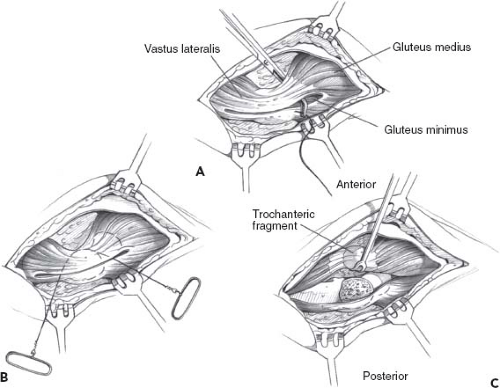
A standard posterior approach is used, centered over the greater trochanter. The fascia lata is divided into anterior and posterior flaps and the approach follows the course of the gluteus maximus fibers proximally. The interval between the gluteus medius and the tensor fascia is developed anteriorly, exposing the joint capsule which is incised. Internally rotating the femur, the gluteus minimus and medius are identified just above the piriformis tendon and the entire muscle mass of the gluteus medius is isolated bluntly from the underlying hip capsule working posteriorly to anteriorly. The external rotators are now isolated, tagged and divided. They are retracted in a posterior direction. The vastus lateralis is longitudinally incised at a point 10 to 15 cm distal to the vastus ridge and 1 cm anterior to the lateral intermuscular septum. The muscle is now elevated subperiosteal from the anterior and lateral shaft of the femur and held forward with a retractor (Fig. 6.5). The osteotomy is performed with an oscillating saw beginning just posterolateral to the insertion of the gluteus medius, so that a 1-cm-thick piece of the trochanter is removed proximally and this tapers to about 0.5 cm just distal to the vastus ridge (Fig 6.6C). The gluteus
minimus should remain attached to the proximal femur. Should the gluteus minimus remain connected to the osteotomized trochanter, this may tend to tether the fragment anteriorly. After repair of the trochanter, this tethering effect may be a problem during external rotation of the femur, but its tendinous insertion can easily be released should this occur. The trochanter, in continuity with the gluteus medius and vastus lateralis, can now be retracted anteriorly, exposing the joint capsule (Fig. 6.6A,B). An alternative method involves leaving the external rotators and piriformis intact on the posterior trochanter and beginning the osteotomy just lateral to their insertion. This has the advantage of leaving an intact posterior capsule and muscle sling that theoretically may prevent any posterior instability.
minimus should remain attached to the proximal femur. Should the gluteus minimus remain connected to the osteotomized trochanter, this may tend to tether the fragment anteriorly. After repair of the trochanter, this tethering effect may be a problem during external rotation of the femur, but its tendinous insertion can easily be released should this occur. The trochanter, in continuity with the gluteus medius and vastus lateralis, can now be retracted anteriorly, exposing the joint capsule (Fig. 6.6A,B). An alternative method involves leaving the external rotators and piriformis intact on the posterior trochanter and beginning the osteotomy just lateral to their insertion. This has the advantage of leaving an intact posterior capsule and muscle sling that theoretically may prevent any posterior instability.
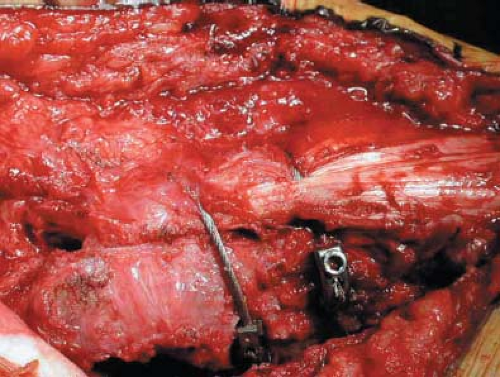
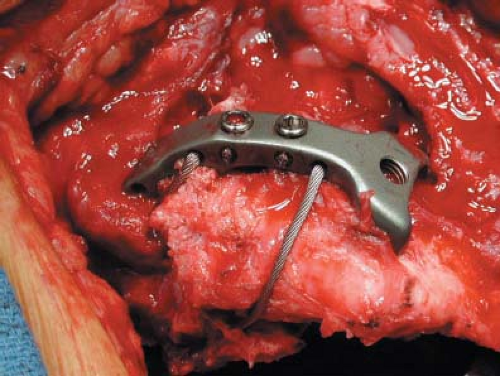
Repair of the sliding osteotomy is traditionally accomplished with two 16- or 18-gauge wires passed through a single drill hole in the lesser trochanter. The use of 1.6-mm cables, no. 5 Ticron sutures, or polymer cables has been used with success (Fig. 6.7). Two corresponding holes (one superior and one inferior) are drilled in the anterior and posterior cortex of the proximal femur and the trochanteric bed. Wires or cables should not be placed around the neck of the prosthesis. Excessive hardware or trochanteric grip devices are generally not necessary unless significant lengthening occurs and reapproximation to the original bed is not possible (Fig. 6.8). Thakur et al. (22) described a novel method of reattachment of the trochanteric fragment with a three-cable configuration. The addition of the third cable below the lesser trochanter provided superior stability when compared to the standard Dall-Miles two-cable construct (Fig. 6.9). In cases where the risk of nonunion is high or the trochanteric bed is compromised, the use of this technique may be of benefit however no clinical results have been reported.
No special precautions are necessary postoperatively. The patient is allowed to be weight bearing as tolerated based on the stability of the prosthetic components and method of fixation.
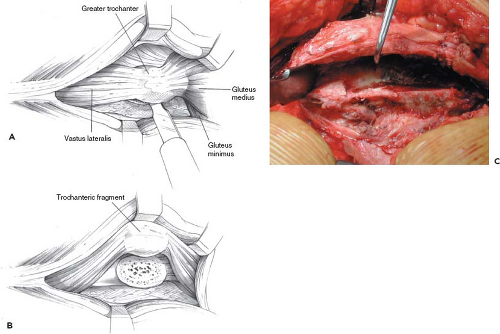
Partial Trochanteric Osteotomy
Anterior trochanteric osteotomy has the advantage of preserving the continuity of the gluteus medius and vastus lateralis attachments anteriorly with a portion of the trochanter and leaving the posterior part of the gluteus medius intact. This transgluteal approach is a modification of the technique described by Hardinge (4). Because the Hardinge direct lateral approach utilizes soft tissue intervals only, Dall questioned the integrity and strength of this tendinous reattachment. He felt that a bone-on-bone repair was superior, with minimal risk of nonunion. Dall reported on this technique in 69 primary total hip arthroplasties and noted no cases of nonunion, bursitis, or abductor lurches (23). This modification of the Hardinge has also been called the Liverpool approach.
A modification of this technique involves leaving the gluteus medius insertion intact and only taking the insertion of the gluteus minimus and vastus lateralis. The advocates of this modification (Ganz) claim a more rapid recovery of abductor power and gait. They also claim that by not splitting the gluteus medius tendon, the risk of damaging the superior gluteal nerve is decreased. This technique allows for preservation of the gluteus medius on the greater trochanter and of the trochanteric blood supply (24). Exposure may be more difficult with this modification; however, occasionally the gluteus minimus tendon is scarred and contracted. In these cases, the minimus is released to prevent a tethering affect on the fragment.
Technique
In Dall’s technique, the insertion of the gluteus medius and vastus lateralis is divided midway between the anterior and posterior margins of the greater trochanter, extending not more than 2 cm above the tip of the trochanter. The anterior margin of the gluteus medius is identified, and curved forceps are passed behind the gluteus medius and minimus and over the anterior capsule, exiting the original incision in the gluteus medius tendon. A Gigli saw is passed deep to the vastus lateralis and gluteus medius and minimus, with both ends exiting the original incision (Fig. 6.10). Partial trochanteric osteotomy is performed with the hip adducted, slightly flexed, and internally rotated. The tendency to take a very small fragment of bone is avoided by starting the saw cut in as posterior a direction as possible. A roughly triangular part of the anterior half of the greater trochanter is obtained, which carries with it the continuity of the anterior half of the gluteus medius with the vastus lateralis as well as the insertion of the gluteus minimus. The hip is now dislocated anteriorly.
Following reduction of the hip, the fragment will lay in its bed without difficulty. This stable osteotomy can be approximated in many different ways. It is attached with no. 5 sutures, cables, or monofilament wires. Excessive hardware or trochanteric grip devices are not necessary. The use of two cables, wires, or sutures is sufficient. Drill holes in the fragment and through the lateral cortex are sufficient. The hardware should not be placed around the neck of the prosthesis. After fixation of the fragment, a repeat of the extremes of motion should be done to ensure adequate stability of the hip and make sure no impingement of the anterior trochanter occurs.
Harris et al. reported on a similar technique that they described as an oblique trochanteric osteotomy. The short external rotators are left attached to the femur and a posterior cut is made superficial to the intertrochanteric ridge. A wider anterior cut is performed that contains the insertion of both the gluteus medius and gluteus minimus (25).
Menon et al. (26) performed a study of 100 cemented primary THAs, of which 50 were performed using an anterior osteotomy of the greater trochanter (modified Liverpool technique, similar to Dall) and 50 utilizing a Charnley transtrochanteric approach. A positive Trendelenburg gait was found in 18% of the anterior osteotomy group and 22% of the Charnley group. Nonunion with migration of greater than 3 cm occurred in 8% and 10% of the groups, respectively. In addition, 85% of patients with a Charnley-type approach had trochanteric pain or bursitis. The authors attributed this to the use of the Dall-Miles cable-grip device and placement of the surgical scar over the reattached portion of the greater trochanter.
Several other techniques for partial trochanteric osteotomies have been described in the literature, including the Stracathro technique (Fig. 6.11) and the horizontal and vertical osteotomies (Fig 6.12) (14,27,28,29). The illustrations demonstrate the variations in each surgical technique. In general, however, they have been replaced by the aforementioned techniques or the extended trochanteric osteotomy (ETO) described below.
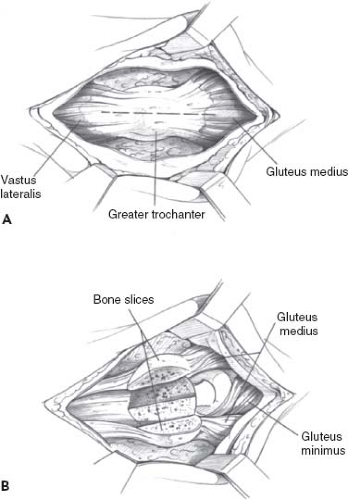 Figure 6.11. A,B: Elevating anterior and posterior slices of the trochanter with the insertions of the gluteus medius and vastus lateralis provides easy access to the hip joint (Stracathro). |
Extended Trochanteric Femoral Osteotomy
The surgeon faced with removal of well-fixed femoral implants during revision THA can find this to be an extremely difficult, time-consuming, and occasionally disastrous undertaking. The exposure afforded by a standard trochanteric osteotomy gives minimal access to ingrowth surfaces of cementless implants or the bone–cement interface of a cemented stem. Cement remaining distal to the prosthesis tip usually requires removal prior to reimplantation. Traditional attempts to remove these implants and the distal cement plug involved flexible osteotomes, high-speed burrs, ultrasonic devices, and cement removal guides. Each of these may cause damage to existing bone stock, with perforations of the femoral cortex, eccentric reaming, and occasionally total loss of continuity of the trochanteric portion of the femur with the remaining proximal femoral tube.
In 1991 Cameron described the use of a trochanteric osteotomy with distal extension to remove a square-shouldered Moore cementless implant that had subsided and drifted laterally (30). He felt that removal of the prosthesis in this situation would result in avulsion of the greater trochanter and the use of a classic trochanteric osteotomy would leave an unacceptable bed for trochanteric reattachment.
Cameron begins the osteotomy with a standard posterior or anterolateral exposure, extending from the tip of the trochanter to a variable point distal to the vastus tubercle where the horizontal osteotomy is made. The trochanteric fragment then includes one-quarter to one-third of the circumference of the femur, while retaining the gluteus medius and minimus attachments. After completion of the revision, the trochanteric fragment is held in place with cerclage wires and reinforced, if necessary, with cortical allograft struts.
Emerson and Head utilized a similar technique, for revision of cemented femoral components (31). They reported on 21 extended trochanteric osteotomies with no cases of trochanteric migration or broken wires. Four of the osteotomies had delayed healing, but all had united by 6 months postoperatively.
Utilizing the original technique by McFarland and Osborne and modifying the technique described by Cameron, Paprosky et al. described a technique, now commonly referred to as the ETO, in which an intact muscle-osseous sleeve composed of a portion of the anterolateral proximal femur is removed with the greater trochanter, gluteus medius, and vastus lateralis (32). This technique involves the creation of an osteotomy of the greater trochanter that includes a variable length of femoral diaphyseal bone levered open on an anterolateral hinge of muscle and periosteum. Advantages are a wide exposure that facilitates the removal of existing implants, correction of femoral deformity, and implantation of revision components while allowing the surgeon to efficiently reconstitute bone stock deficiency (Fig. 6.13). The ETO heals predictably and further allows for appropriate tensioning of the abductor mechanism to decrease postoperative instability.
The indications for use of an ETO are numerous and essentially include the removal of any well-fixed cemented or cementless femoral implant. It is the only approach that avoids severe damage to the proximal femur when a well-fixed, fully porous-coated stem requires removal. Even in cases of loose cemented femoral components, the direct access to the femoral canal it affords greatly expedites the removal of retained cement. The abductor-vastus sleeve remains intact during this exposure similar to the trochanteric slide. This assures blood supply to the fragment and the vastus lateralis assists in controlling proximal migration of the fragment. The ETO is also indicated in cases of varus remodeling of the femur, which is present in approximately one-third of failed femoral components. In these cases, the ETO allows for deformity correction and facilitates the implantation of revision components.
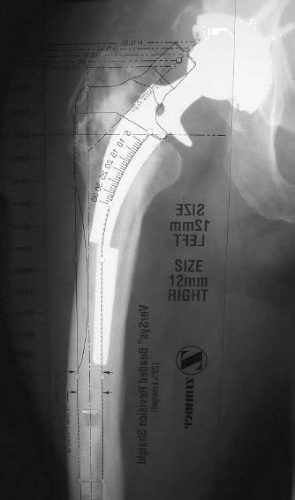
Preoperative planning is critical to the performance of an ETO to ensure adequate length for safely removing well-fixed components and correcting deformity while maintaining adequate femoral isthmus for distal fixation (Fig. 6.14). The distal extent of the osteotomy should be carefully determined preoperatively; the length will depend on the amount of
femoral access required to remove retained cement or, in the case of cementless components, disrupt the bone–cement–prosthesis interface. A minimum of 4 to 5 cm of intact endosteal canal must be present on the distal extent of the osteotomy for obtaining an appropriate interference fit for the revision femoral component.
femoral access required to remove retained cement or, in the case of cementless components, disrupt the bone–cement–prosthesis interface. A minimum of 4 to 5 cm of intact endosteal canal must be present on the distal extent of the osteotomy for obtaining an appropriate interference fit for the revision femoral component.
Our preferred method for femoral reconstruction with an ETO is to use a fully porous-coated, diaphyseal-fitting femoral component. These devices have been associated with outstanding long-term results in the setting of revision THA and the surgical technique is straightforward and applicable to the vast majority of revision situations (33). The use of tapered long stem revision components (Wagner style) are now being used following an ETO due to their flexibility and ease of use. Many are modular which allows the surgeon to adjust offset and version while obtaining adequate distal fixation. Long-term results on this technique will be needed to verify its usefulness in the setting of an ETO. For the patient with a large ectatic proximal femur, the use of impaction grafting was popularized by the surgeons in England (34). Combining this bone grafting technique with an ETO, we studied the biomechanical suitability of this construct and found it to be stable (35




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree