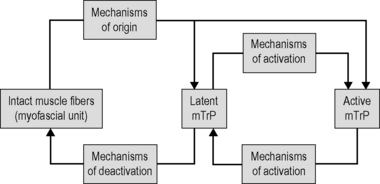
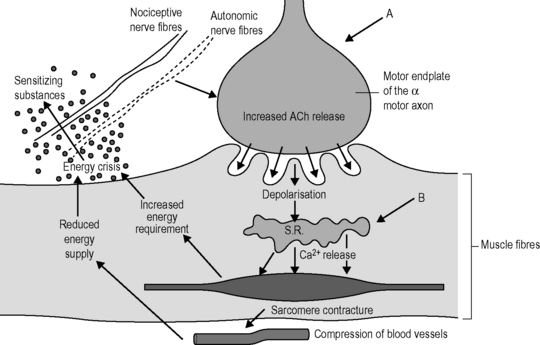
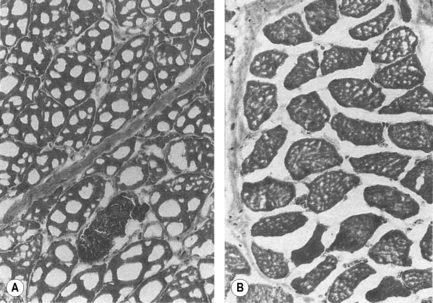
5.7 Trigger points as a fascia-related disorder Myofascial trigger points (mTrPs) are widespread and are frequently responsible for pain in the musculoskeletal system (Fishbain et al. 1986; Skootsky et al. 1989; Friction 1990; Gerwin 1995; Travell & Simons 1999; Jarrell 2004; Doggweiler-Wiygul 2004; Hwang et al. 2005; Anderson et al. 2006; Ardic et al. 2006; Borg-Stein & Wilkins 2006; Fernandez-de-las-Penas et al. 2006, 2007; Treaster et al. 2006; Ettlin et al. 2008; von Stülpnagel et al. 2009). In the original sense of the word, a trigger point (TrP) is a point from which symptoms known to the patient, mostly in the form of referred pain, are caused (or triggered). Various types of TrPs have been distinguished (Travell & Simons 1999; Gautschi 2010): • Active or latent TrPs. Active TrPs already demonstrate their characteristic pain pattern at rest or during physiological stress or movement. If an active TrP is provoked by using pressure or traction (stretching) or needling, this mechanical stimulation reproduces the pain (localized or referred) familiar to the patient. In contrast to this, latent TrPs are not spontaneously painful at rest or during physiological strain/exercise; latent TrPs are clinically silent. Not until it has been provoked by strenuous pressure can the pain – mostly referred pain – be triggered, although the patient is not familiar with this from his/her everyday experiences. Latent TrPs can demonstrate all the clinical properties of an active TrP – with one exception: It is not possible to reproduce the symptoms emanating from the latent TrP. • Depending on the manner and time of occurrence of a TrP, primary and secondary TrPs are differentiated into synergists and antagonists and satellite TrPs (arising in the referred pain zone of a primary TrP). • If a TrP is in the muscle tissue, it is described as a myofascial trigger point. If a TrP lies in a tendon, a ligament, or in the periosteum, etc., it is known, respectively, as a tendinous, ligamentary, or periosteal TrP. There is pathophysiological evidence of localized hypoxia in the center of an mTrP (Brückle et al. 1990), a changed EMG potential, which can be interpreted as a sign of the malfunction of motor endplates (Travell & Simons 1999), and characteristic changes in the biochemistry. In the immediate surroundings of an mTrP, the concentration of substance P and CGRP, bradykinin, serotonin, norepinephrine (noradrenaline), tumor necrosis factor-α (TNF-α), as well as interleukin (IL)-1β, IL-6, and IL-8 are markedly elevated, while the pH value is definitely reduced (Shah et al. 2005, 2008). The low pH value (5.4 instead of 6.6) and the two to four times increased concentration of pain and inflammatory mediators (compared to the reference tissue without active mTrPs) lead to a change in nociceptor activity in the sense of peripheral sensitization. Rigor complexes are histomorphologically recorded in the nucleus zone of mTrPs (myosin and actin filaments remain in maximally close position) with reactive overextension of the bordering sarcomeres (Simons & Stolov 1976) and intramuscular connective tissue changes (Feigl-Reitinger et al. 1998). The pathophysiological changes are like individual mosaic stones that fit together to form a picture. The factors which combine in the formation of mTrPs are summarized in the “energy crisis model” (Fig. 5.7.1) (Travell & Simons 1999; Mense et al. 2001). Fig. 5.7.1 • Model of energy crisis for the origin of mTrPs. From Travell & Simons, 1999, with permission. Dysfunctional motor endplates (characterized by low-threshold distribution of acetylcholine; Fig. 5.7.1, Arrow A) or traumatic damage to the sarcoplasmic reticulum (by strain, traumatic overextension, or direct injury of a muscle with partial rupture of the sarcoplasmic reticulum; Fig. 5.7.1, Arrow B) cause a permanent contraction of locally restricted muscle fiber sections (contraction knot). Contraction knots compress the local blood vessels and the reduced perfusion (local ischemia) causes a local oxygen deficit (hypoxia). The permanent contraction in the contraction knot is associated with an increased energy requirement (ATP) and leads to a locally restricted energy crisis (ATP deficiency) with the local hypoxia. The local ischemia leads to ischemically caused hypoxic tissue alterations with local inflammatory processes. Inflammatory processes run through regularly differing phases and end in each case with the formation of a connective tissue scar. The connective tissue draws together and prevents the decontraction of the shortened sarcomeres. This is the first chronification stage where there are myofascial pain problems (Dejung 2009). Connective tissue shortening and changes (pathological crosslinks) gather both intramuscular collagenic tissue (endomysium, perimysium) and muscle fascia and intermuscular collagenic tissue over time (i.e., with chronic myofascial pain syndromes). Histomorphological examination shows that in muscle tissues with mTrPs, the endomysial spaces between the individual muscle fibers are always narrower than in controls without mTrPs (Feigl-Reitinger et al. 1998; Fig. 5.7.2). Fig. 5.7.2 • In muscle tissue with mTrPs, the endomysial spaces are always narrower than in controls without mTrPs. Electron microscope image, enlarged 300 times. (A) Muscle tissue with mTrP: shrunken endomysium. (B) Control without mTrPs: endomysium normal. From Feigl-Reitinger et al., 1998, with permission. Local ischemia acts as a nociceptive stimulus and leads to the release of sensitizing substances; myofascial pain is thus ischemic pain (Dejung 2009). Disorders directly induced by mTrPs reveal themselves in the form of: • Pain (local and referred) with manifold qualities (dragging, stabbing, burning, or dull, definitely delimited or diffuse, superficial or “deep in the joint”, etc.). The trigger point activity is sometimes expressed in the form of paresthesia, dysesthesia or hypoesthesia (tingling, burning, feeling “as if restricted by a tight cuff” or feeling “something is swollen”, numbness, etc.). • Motor function disturbance: reflex muscle weakness and muscle weakness caused by pain without atrophy and intramuscular and intermuscular coordination disorders are directly caused by mTrPs (Travell & Simons 1999; Lucas et al. 2004; Ivanichev 2007). • Autonomic and trophic disorders: frequently deriving from the autonomic phenomena of mTrPs (Travell & Simons 1999). They can become apparent in any number of ways, both in the area of the trigger point itself and in the area of the referred pain: Increase of skin temperature in the area of the mTrP, changes to the skin temperature and metabolism in the area of the referred pain, increased sweat secretion, nausea or dizziness, etc. They are interpreted as reflex responses of the sympathetic nervous system (Dejung 2009). • Disorder of intramuscular and intermuscular coordination: economy of movement is prevented by taut bands and connective tissue changes. As a result, this leads to poor posture and strain of the muscles and joints. • Restricted movement: taut bands lead to shortening of the muscles, which in turn leads to reduced mobility and articular dysfunction (Lewit 2007). Fascia adhesions between neighboring muscles often cause drastically restricted mobility. • Perfusion disorders: if the taut bands compress the blood vessels, this leads to perfusion disorders (formation of edema) and trophic/metabolic disorders. • Neuromuscular entrapment: neural structures perforate the muscles at many sites. If the muscle fibers at these sites are tense as a result of mTrPs, they exercise pressure on the nerve structure. The nerve tissue is less well perfused and this leads to symptoms in the supply area of the neural structure (dysesthesia, weakness, metabolic disorder/trophism). • Irritation of deep sensitivity, proprioception and nociception: connective tissue dysfunction alters the flow of impulses which come from the receptors which lie in the connective tissue of the muscle. • Peripheral chronification: connective tissue contractions overlie and fix the rigor complex, which means peripheral chronification of myofascial pain. Manual palpation is the most commonly used method of identifying mTrPs in everyday clinical practice. Diagnosis by palpation is based on three main criteria (Travell & Simons 1999): • Identification of the taut band belonging to the mTrP. • Finding the most tender spot along the taut band. • Reproduction of the pain pattern and other symptoms recognized by the patient on mechanical provocation of the mTrP (pressure, traction, needling). The reliability of the clinical diagnosis of mTrPs has been tested in various studies. It was revealed that the intertest reliability of the identification of mTrPs varies a great deal and indeed depends on the knowledge and experience of the therapist. The kappa values differ a great deal depending on the study and they range from poor reproducibility (k = 0.35) for nontrained and/or inexperienced therapists (Nice et al. 1992; Wolfe et al. 1992) to moderate (Njoo & van der Does 1994; Hsieh et al. 2000) and excellent reproducibility (k = 0.8) for specifically trained therapists and those experienced in palpation (Gerwin et al. 1997; Al-Shenqiti & Oldham 2005; Bron et al. 2007; Licht et al. 2007). At the center of trigger point pathology lies a locally pronounced hypoxia (in particular an energy crisis; Fig. 5.7.1). Various causes can lead to oxygen deficiency and reduced energy (ATP deficiency) in the muscle tissue and as a result to persistent rigor complexes respectively contraction knots. The most common etiological factors can be summarized in the following categories: • Direct trauma (e.g., immediate muscle injury as a direct result of violence in sport, accidents, etc.). • Acute overextension of the muscles (e.g., caused by sport or accident). • Acute strain (e.g., caused by sport or accident). • Chronic strain of the muscles (e.g., caused by posture, repetitive movements at work or in training, long-term contraction in approximate position, eccentric muscle activity, stress-induced strain, etc.). • Trigger point activity in other muscles (trigger point chains with secondary TrPs or satellite TrPs). The above etiological factors frequently lead initially to the occurrence of latent TrPs, which are clinically silent. Latent TrPs can be activated by the further effect of mechanisms of origin but also by contributory factors such as cold, wet, draught, stress, etc. which do not demonstrate a damaging effect in healthy muscle tissue (so-called mechanisms of activation; Fig. 5.7.3). Active TrPs for their part can be retransformed by deactivation processes (such as rest, the body’s own regeneration processes, therapy) to latent TrPs or healthy muscle tissue (Fig. 5.7.3).
Trigger points (TrP)
Pathophysiology
Clinical symptoms
Diagnosis
Etiology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Trigger points as a fascia-related disorder