Triflange Acetabular Components for Complex Revision Cases
Patient Selection
Revision hip arthroplasty in the setting of massive acetabular bone loss. Most of these patients will have already undergone two or more acetabular revisions
Physical examination should include prior surgical incisions and a thorough neurovascular examination
Infection should always be ruled out using inflammatory markers and aspiration of the hip
Other patient-specific factors that should be evaluated include nutrition status and an anemia workup if the hematocrit is less than 30. Two particular subsets of patients have been noted to have higher complication rates
Elderly patients with malnutrition
Untreated or undiagnosed patients with anemia
Triflange acetabular components are commonly used as a salvage type procedure. Classic indications include Paprosky type 3B defects, pelvic discontinuity, and salvage of prior failed porous metal augments, structural allografts, or cup/cage constructs
Preoperative Imaging
AP pelvis—the majority of information can be obtained from this radiograph
Judet views of the pelvis—improves visualization of the anterior and posterior columns
CT scan with 3D reconstructions—this is used to create a 1:1 bone model
It is important to note that bone adjacent to osteolytic lesions and prior structural allografts may appear functional on imaging but lack structural viability
The Design and Production Process
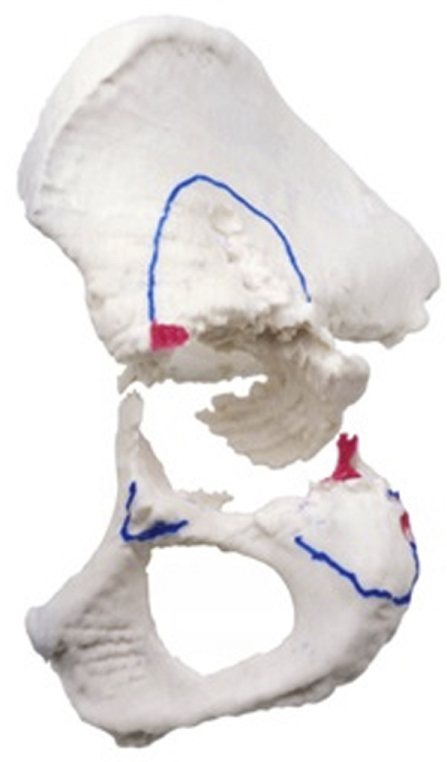
Figure 1Photograph showing an actual CT model of a patient with a pelvic discontinuity. The red marking are areas of bone removal. The flange locations are marked by the surgeon.
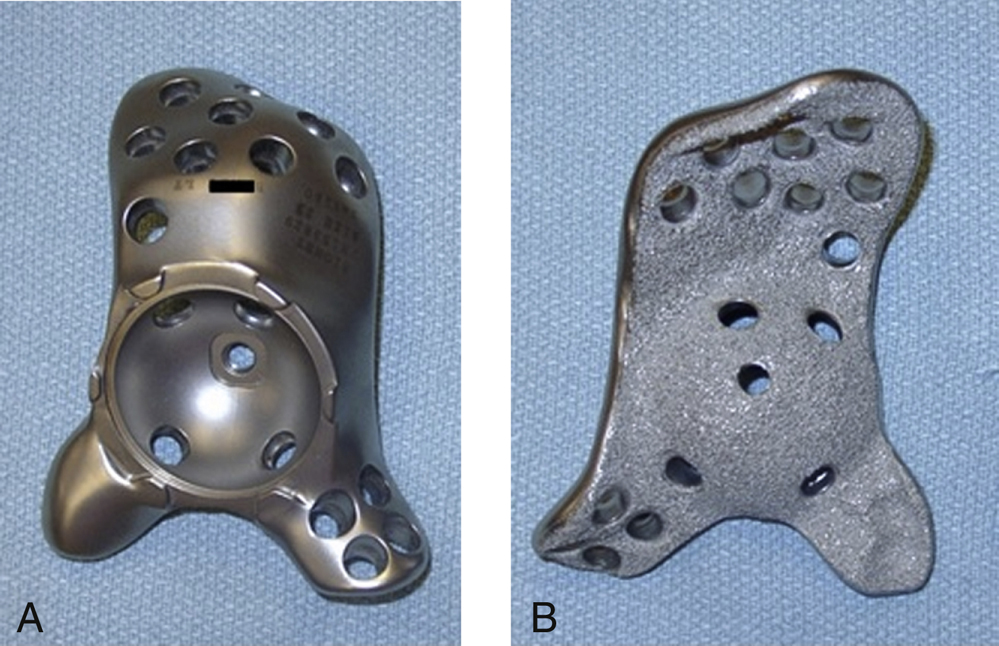
Figure 2 Aand B, Photographs showing the front and back of a triflange component. Note the ingrowth surface.
The total process from start to finish for the construction of a triflange component takes approximately 8 to 16 weeks
Thin slice CT scan is done per implant manufacturer protocol, typically 2 mm slices
The CT scan is then used to create a 1:1 hemipelvis model (Figure 1)
The surgeon marks the regions on the model for flange placement. The minimum flange thickness is 6 mm
Iliac flange provides the majority of the surface area for support of the implant. In general, a larger iliac flange is required in cases with greater bone loss. Most implants include two rows of 3 to 4 screws each in the iliac flange
Ischial flange has a lateral and posterior surface for flange orientation. Ischial screw pullout is a known complication and can be minimized by using 3 to 4 screws, locking screws, or bone cement in lytic lesions to improve fixation. The ischial flange must be rounded to avoid damage to the sciatic nerve
Pubic flange acts as a reference point. The author prefers to not use any screw fixation in the iliac flange
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


