Fig. 14.1
CT scan showing a rare injury pattern with a capitellar shear fracture and complete triceps tendon rupture from a snowboarding accident (Courtesy of MoRe Foundation)
Partial ruptures are underdiagnosed for different reasons. Not all patients seek medical care as pain may be tolerable or intermittent and there is no obvious deformity. A delayed presentation is typical as these patients will often have good elbow function and range of motion with the sole symptom being pain on resisted extension. These patients may not seek medical advice for months or even years after the index injury and some may not be seen until a full rupture occurs [4].
The clinical examination is important and will typically vary with the extent of the rupture, possible associated lesions, and the time from the index injury. In acute ruptures, a posterior swelling, bruising, or ecchymosis can be seen on inspection. In chronic, complete ruptures, two problems are apparent. Besides decreased extension strength, these patients often complain of the asymmetrical appearance of both arms from atrophy or retraction of the muscle belly. Especially in muscular patients, this deformity may be pronounced.
The physical exam of the elbow starts with a general examination of the elbow. Range of motion will, in the absence of associated trauma, typically be normal. Passive flexion is often painful as the ruptured tendon in acute lesions will get stretched with increasing flexion. Extension is typically decreased bilaterally in weight lifters due to biceps hypertrophy.
In a complete rupture, it will be difficult or impossible for the patient to extent the arm against gravity or against resistance. In most cases, the lateral and/or medial triceps expansions will still be intact and the patient will have at least some extension force. It is important to compare both sides as some patients may still have considerable extension strength even with a full-thickness tear. This is especially the case in chronic ruptures.
Triceps strength is tested by extending the arm. This leads to weakness in resistance compared to the other side. It is important to start with the elbow fully flexed (flexion beyond 90°) as this will detect an isolated rupture of the deep triceps insertion.
A modified Thompson test has been described, where the muscle belly is squeezed and no resultant extension of the forearm results [6].
Palpation should always be performed with the triceps both relaxed and contracted. Sometimes, there is a palpable gap in the tendon, especially in complete, full-thickness ruptures of the tendon proper. However, palpation will be painful and the patient may not tolerate deep palpation. A hematoma may fill the gap and this may falsely feel like a soft tissue swelling rather than a ruptured tendon.
In a partial tear, no gap may be palpable as superficial fibers will still be intact and cover the defect (Fig. 14.2). In chronic lesions, even in complete ruptures, the gap in the tendon will often have filled with scar tissue (Fig. 14.3).
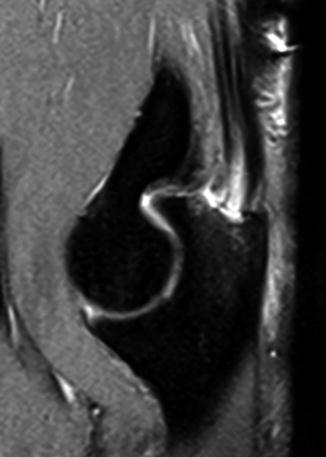

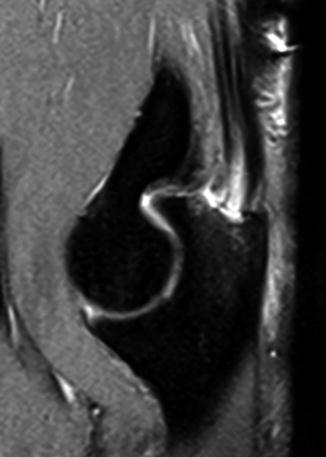
Fig. 14.2
MRI scan showing a partial rupture at the deep layer of the triceps tendon (Courtesy of MoRe Foundation)

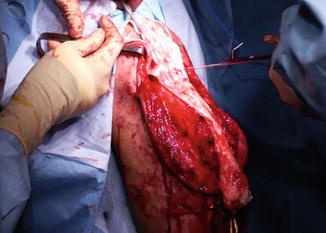
Fig. 14.3
Intraoperative view of a chronic triceps tendon rupture. Notice how the gap is filled by scar tissue in an attempt to heal the tear (Courtesy of MoRe Foundation)
14.3 Imaging
Plain radiographs can show the presence of flecks of avulsed bone from the olecranon. This is pathognomonic for this lesion and is called the “flake sign” (Fig. 14.4). Radiographs are also used to rule out associated lesions or signs of chronic triceps tendon overuse, such as the commonly found traction spur (Fig. 14.5). Bony associated lesions can further be examined using a CT scan, but this is not necessary for isolated triceps tendon lesions (Fig. 14.1).



Fig. 14.4
Plain radiograph showing the flake sign. This is pathognomonic for an acute triceps tendon avulsion (Courtesy of MoRe Foundation)

Fig. 14.5
Signs of chronic triceps tendon overuse. (a) A traction spur is commonly found in chronic overuse of the triceps tendon (Courtesy of MoRe Foundation). (b) Clear calcification of the triceps tendon insertion leading to a high-grade partial rupture (Courtesy of MoRe Foundation)
An ultrasound (Fig. 14.6) can confirm the diagnosis if a triceps tendon rupture is suspected [12].
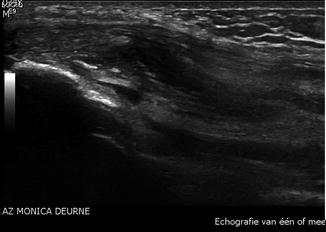
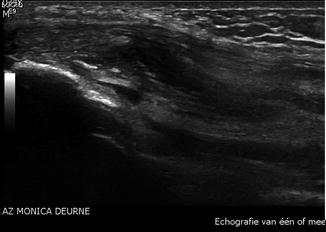
Fig. 14.6
Ultrasound scan showing a partial triceps tendon tear (Courtesy of MoRe Foundation)
Magnetic resonance imaging (MRI; Fig. 14.7) is often not necessary to confirm the diagnosis, but in chronic cases or partial ruptures (Fig. 14.2), MRI is of value in the diagnosis and localization of the tear [13, 14]. It is also used to quantify the extent of the tear and is very helpful in the possible need for triceps repair at the preoperative planning. Classically, on the MRI, a fluid-filled gap can be seen where the muscle is retracted. The triceps muscle belly may not have the tendency to migrate proximally as the lateral and/or medial triceps expansions are often intact, despite a full-thickness rupture of the tendon proper.


Fig. 14.7
MRI scan showing a complete full-thickness rupture of the triceps tendon with moderate retraction (Courtesy of MoRe Foundation)
14.4 Treatment Options
Treatment of triceps tendon ruptures depends on different criteria such as the extent of the rupture and/or the activity level of the patient [22].
Ruptures involving greater than 50 % of the tendon, as shown on MRI, are recommended for early surgical repair to prevent late functional disability [10, 23]. With partial ruptures up to 50 % of the tendon and in the absence of an extension lag, surgical repair is controversial [24] and depends mainly on the functional impairment to the patient. If an extension lag is present, surgical repair is recommended [25–28].
Results of conservative treatment are unclear and often unpredictable. Nonoperative treatment may involve splinting with elbow immobilization for 3–6 weeks at 30° of flexion [29] followed by a training program specifically tailored to the athlete.
Even with a partial rupture, a surgical procedure can be proposed. This to avoid the evolution to complete rupture and functional degradation but other factors also play a role, such as the timing in the season or remaining goals in the athlete’s career.
When the triceps rupture is associated with fracture of the radial head, or rupture of the medial collateral ligament, surgery is indicated [6].
14.5 Surgical Technique
Anesthesia can be general or regional with a supraclavicular block. The patient is placed in prone position or lateral decubitus, with the arm over a support. A tourniquet can be installed but is often not inflated in order to increase the chance of reducing the tendon back to its insertion on the bone.
A posterior incision is made, centered over the olecranon. The length of the incision depends on the retracted position of the tendon. The olecranon is debrided of any residual tendon tissue, scar tissue, or fibrosis to create a bleeding surface in order to promote healing of the tendon to the bone interface (Fig. 14.8). A non-resorbable no. 2 suture is used to securely suture the tendon on both the lateral and medial sides. A 2.5 mm drill is used to create bone tunnels in the proximal ulna. A suture retriever can be used to shuttle the sutures through the bone and the sutures are tied proximally, taking care to bury the knot and not to leave it directly on the subcutaneous border of the ulna, as this may cause pain. Alternatively or additionally (Fig. 14.9), one or multiple strong bone anchors can be used [30], depending on the preference of the surgeon. In this case, a knotless repair [31] can be done or the sutures are tied proximally and buried in the triceps muscle, to avoid irritation.



Fig. 14.8
Intraoperative view of an acute triceps tendon rupture (Courtesy of MoRe Foundation)

Fig. 14.9
Hybrid fixation of a full-thickness triceps tendon tear, using bone tunnels and anchors
Once the repair has been done, it is important to test the tension-free mobility of the elbow and the integrity and strength of the repair (Fig. 14.10). Gapping may occur with further flexion of the elbow and the surgeon should decide if reinforcement of the repair is necessary at this stage or if the elbow needs to be protected by restricting the amount of flexion for a period of time postoperatively.


Fig. 14.10
Intraoperative testing of the strength of the fixation will determine the immediate postoperative protocol. No gapping was found in this patient and the patient was allowed to mobilize the elbow as tolerated in a compressive bandage to protect the wound (Courtesy of MoRe Foundation)
In chronic cases, a direct repair may be possible and is the preferred technique [10]. The incision and approach to the tendon are not different in the chronic setting. Usually, there is no clear palpable or visible gap between the olecranon and the triceps stump, as it is filled with scar tissue. It may be difficult to determine the demarcation between scar tissue and viable triceps tendon. Careful debridement of scar tissue is necessary to obtain healthy tendon for repair. The tendon is mobilized and the elbow is positioned in extension to facilitate the primary repair. The tendon is then repaired to bone, as described above. If it is not possible to bring the retracted tendon back to bone or if too much tension is needed or failure of the repair occurs when the elbow is tested from extension to flexion, the repair is augmented with a graft. Both auto- and allograft tendons [32–34], as well as synthetic grafts [35], have been used to augment the repair. A hamstring or palmaris longus graft can be used and woven through the triceps stump and attached to the proximal ulna [32, 33].
Our preference is to use an Achilles tendon allograft [10]. The advantage of this graft is that the fan-shaped graft resembles the anatomy of the triceps tendon (Fig. 14.11). The Achilles tendon can cover the defect that may remain after maximal mobilization of the triceps tendon stump. The elbow is held in extension and the triceps is temporarily fixed as close as possible to the olecranon, in order to tension the muscle. The graft is then placed over the triceps muscle, musculotendinous junction, and the tendon. The graft covers the remaining defect between the triceps stump and the olecranon and is draped over the proximal ulna. Non-resorbable no. 2 sutures are used to suture the graft to the triceps. We use medial, central, and lateral rows of sutures. It is important not only to make sure that the graft is securely fixed for the strength of the repair but also to avoid hematoma or seroma formation between the graft and the tendon, jeopardizing ingrowth of the graft. There are essentially two different methods to fix the Achilles tendon distally to the olecranon. The calcaneal bone block at the distal end of the graft can be shaped to fit over the proximal ulna and can be fixed with cerclage wires. This has the advantage of bone-to-bone contact, which may offer a stronger fixation. Unfortunately, even with an excellent fit, the bone graft is quite bulky and may cause problems, due to its direct subcutaneous position. We reserve this option for patients with poor bone stock or bone loss, such as rheumatoid patients or following arthroplasty of the elbow, and have not used this method in athletes. In most traumatic triceps tendon ruptures in this group, the bone of the proximal ulna is of sufficient quality to allow for fixation of the graft through bone tunnels or with bone anchors, as previously described. Reconstructions or augmented repairs have been shown to be stronger than direct repairs in a cadaveric study [36] and can lead to a good clinical outcome in the general population, despite the poor quality of the chronically ruptured tendon and the potential for residual elbow stiffness [10]. However, better peak strength and a shorter time to recovery have been reported in repairs compared to reconstructions and are certainly preferable in this group of high-demand patients [10].