Fig. 15.1
(a) Posterior aspect of the elbow, showing the triceps brachii muscle and a clearly represented triceps aponeurosis. The asterisk indicates the olecranon whereas the double-headed arrow shows the lateral expansion of the aponeurosis. The white arrow points at the long head of the triceps (b); the triceps aponeurosis was detached and reflected (surgical blade) and the common tendon was revealed, as indicated by the surgical clamp. The arrow indicates the lateral head of the triceps, whereas the asterisk indicates the anconeus muscle. The finger indicates the long head of the triceps brachii, which is located medially to the tendon
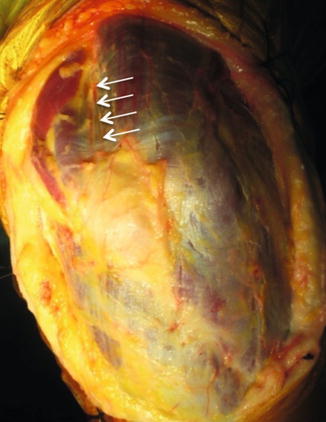
Fig. 15.2
Posterior aspect of the elbow showing absence of the triceps aponeurosis. The superficial muscle fibers of the lateral and long head are easily distinguishable. The arrows indicate the site of the common tendon of the triceps, covered by the muscle fibers
The triceps insertion is a wide area or footprint rather than a focal point on the olecranon. In a cadaveric study, the triceps footprint was found to cover a large area of the supero-posterior aspect of the olecranon, with a mean surface ranging from 466 to 646 mm2; moreover, it was found to start 12 mm distal to the tip of the olecranon and to overlap with the posterior capsule [10]. The tendon width at the insertion was greater than that of the olecranon, which indicates that the distal triceps does not end at a specific insertion point, but extends well distal to the olecranon tip and includes the medial, lateral, and posterior borders of the olecranon.
The extensor mechanism of the elbow comprises two components: the triceps tendon itself (the confluence of the tendon from all three heads inserting on the olecranon) and the lateral and medial triceps expansions. The mean length and width of the distal tendon at the level of insertion are reported to be 20.52 mm (SD 2.02) and 22.65 mm (SD 2.40), respectively [10]. The lateral triceps expansion fans out laterally from fibers of the triceps and blends into the fascia of the anconeus muscle, the extensor carpi ulnaris muscle, and the posterior border of the ulna; the triceps expansion also inserts on the antebrachial fascia of the forearm distally [11]. The expansion length from a line between both epicondyles to its insertion is 4.02 cm (range 2.3–6.0 cm) [12]. Owing to its wide lateral insertion, the triceps expansion often needs to be concomitantly repaired in cases of triceps rupture. Although the triceps seems to be able to compensate for injuries to the triceps expansion (e.g., by sacrificing the triceps expansion in the classic intra-articular olecranon osteotomy exposure), the triceps expansion does not fully compensate for injuries to the triceps (e.g., triceps avulsion). The insertion of the medial aspect of the triceps expansion is located on the posterior crest of the ulna, adjacent to the medial head [13]. Hypertrophy of the medial head of the triceps muscle may cause ulnar nerve impingement, a condition occasionally observed in weightlifters [13]. The distal portion of the medial head has a distinct muscle belly, while the deep insertion is muscular with a small amount of tendon [11]. Upon gross examination, the tendon of the medial head of the triceps is smaller and deeper to the tendon of long and lateral heads. There is invariably a thin fascial layer that separates the long and lateral heads from the deeper medial head. This fascial plane has been clearly defined, and dissection can easily be accomplished. The deep tendon is readily identifiable after the overlying conjoined tendon of the long and lateral heads of the triceps has been divided longitudinally. However, upon histological analysis, no separation between the deep and superficial tendons is observed at their insertion on the olecranon [11].
The triceps is innervated by the radial nerve (C6–C8). The main function of the triceps is to extend the forearm at the ulno-humeral joint. However, since it originates at the infraglenoid tuberosity, the long head of the triceps is also believed to contribute to arm adduction and extension. The overall muscle-tendon length of the triceps is critical to its motor function; indeed, a biomechanical study has shown that a 2 cm length reduction between its origin and insertion may result in a 40 % loss in extension strength [14]. Gerbeaux et al. investigated the lever arm of the triceps muscle in cadaveric specimens [15]. Adopting the long head of the triceps as their model, they showed that the lever arm value of the triceps ranged from a maximum of about 0.5 radians (45°) to a minimum of about 2 radians (180°). This finding suggests that the triceps lever arm is greatest when the elbow is fully flexed. Although in this cadaveric model the triceps was fixed, it is noteworthy that the scapular insertion of the long head of the triceps provides a greater degree of freedom, producing a potentially more dynamic system in vivo. The length of the triceps lever arm suggests that it exerts the greatest strength in flexion, though it should be borne in mind that the separation of individual sarcomeric units substantially weakens the triceps when it is stretched; the triceps thus exerts more power when the elbow is closer to full extension [8].
15.3 Etiology and Mechanism of Injury
Considerable force is required before a normal triceps tendon ruptures. Direct posterior force on the elbow and weightlifting are two common mechanisms [4, 16–20]. Other documented causes include swinging a baseball bat, motor vehicle accidents, seizures, pitching, volleyball serving, punching, and hammering [21–28]. If direct trauma is excluded, the biomechanics of injury are similar in each of these mechanisms. Uncoordinated contraction of the triceps against the flexed elbow, combined with a deceleration-like impact, overloads the tendon eccentrically [2, 5, 7, 16, 17, 20, 21, 25, 29–31]. Although the tendon can withstand three times tetanic contraction [32], various factors may alter its structural integrity and reduce its maximum load capacity [16, 21]. Distal triceps tendon ruptures may even occur spontaneously or following minimal trauma in patients with concomitant significant systemic or local pathological conditions. Pathological changes that weaken the tendon are believed to be the underlying mechanism in almost all tendon ruptures. The vast majority of reports have associated triceps tendon rupture with anabolic steroid use or steroid treatment, hyperparathyroidism, renal osteodystrophy, hypocalcemic tetany, Marfan syndrome, osteogenesis imperfecta, rheumatoid arthritis, lupus, or type I diabetes [2, 4, 7, 16, 19, 21, 29, 31, 33–35]. Connective tissue degeneration due to ciprofloxacin is also reported to increase the likelihood of tendon rupture [7]. Professional football players and body builders are believed to have a higher risk of rupture than the general population, possibly owing to their training regimen, the use of locally injected steroids in case of olecranon bursitis, and the violent nature of the sport itself [2]. Adolescent athletes with incompletely fused or recently fused physes are also susceptible to triceps tendon rupture, though this is an extremely rare event [5].
15.4 History and Physical Examination
A history of eccentric loading in flexion against the triceps contracture (e.g., fall or weightlifting) associated with acute pain and weakness provides the most reliable diagnosis. The patient presents with pain and swelling over the posterior aspect of the elbow, though the pain is frequently not dysfunctional. As a consequence, patients may underestimate the severity of the trauma after the acute event and wait several weeks before going to see the orthopedic surgeon, complaining of reduced strength and persistent pain.
In the acute setting, the physical examination reveals tenderness, swelling, muscle spasm, and ecchymosis. Although a defect proximal to the olecranon may be palpable, this is not a common finding in partial tears and obese patients [36]. The inability to actively extend against gravity is a pathognomonic sign of complete rupture. However, complete tears do not always result in the inability to actively extend against resistance owing to an intact lateral expansion or a compensating anconeus muscle [36, 37]. In such cases, assessing the reduction in strength against gravity or resistance starting from maximum elbow flexion is mandatory.
Viegas has recommended the use of a modified Thompson squeeze test as a clinical diagnostic tool [38]. During this passive extension test, the patient lies prone with the elbow at the edge of the examination table. The forearm is then allowed to hang over the edge of the table so that it is flexed at 90° in a relaxed position. When the examiner firmly squeezes the triceps muscle in a patient with complete disruption of the triceps tendon and the lateral expansion as well, he will not observe a passive extension of the elbow. No study has yet demonstrated the sensitivity and specificity of this diagnostic test.
In an unpublished study, Giannicola proposed a new diagnostic test for triceps tendon rupture called the “posterior hook test.” This test is similar to the hook test described by O’Driscoll et al. for distal biceps tendon avulsion [39]. To perform the posterior hook test, the patient stands with the examiner behind him. The patient is the asked to contract and relax the triceps muscle with the forearm fully extended. The examiner’s index finger is inserted into the superomedial side of the olecranon, laterally to the ulnar nerve in an attempt to hook the medial portion of triceps tendon. In contrast to O’Driscoll’s test, in the posterior hook test, it is impossible to insert the finger beneath the tendon during the triceps contraction in healthy patients; indeed, the examiner will encounter a cord-like structure belonging to the triceps tendon that prevents the index finger from sliding in a medial-to-lateral direction along the humeral bone surface. By contrast, in patients with a triceps tendon tear, this cord-like structure is not encountered and the examiner’s finger can reach the central and lateral bone surfaces of the distal humerus. The clinical tests preferred by the authors are showed in Fig. 15.3.
Fig. 15.3
Clinical test used for the diagnosis of triceps tendon tear. (a) In case of distal triceps tendon rupture, a palpable defect proximal to the olecranon may be apparent. This evidence of rupture is called “gap sign.” (b) The “Viegas squeezing sign.” (c) The inability to actively extend against gravity is usually a sign of complete rupture, with involvement of the lateral expansion, whereas (d) the ability to actively extend against gravity associated with the inability to extend against resistance may be a sign of partial rupture. (e) The “posterior hook sign”
Diagnostic difficulties, low clinical suspicion, and underestimation of injury severity may result in delayed diagnosis and surgical intervention, with consequent prolonged disability [16, 36]. Diagnosis of triceps tendon rupture requires a high degree of suspicion; indeed, in one recent study, almost 50 % of acute triceps ruptures were found to have been initially misdiagnosed [16]. Concerning chronic tears, the most common complaints are pain, mild extension lag, and weakness. In such cases the lack of swelling and acute pain enhance the reliability of the clinical examination.
15.5 Imaging
AP and lateral radiographs of the affected elbow should always be performed. The lateral radiograph may show the presence of small olecranon avulsion fragments, which is referred to as the “flake sign” and is considered almost pathognomonic of a triceps tendon rupture (Fig. 15.4a) [5, 31]. Similarly, the presence of dystrophic calcification or heterotopic ossification (an indirect sign of tendon degeneration) at the level of triceps tendon insertion should be interpreted as a sign of probable triceps rupture (Fig. 15.4b). When Giannicola et al. analyzed the tendons from ten patients with a triceps tear, they found metaplastic bone tissue within the tendon in 20 % of cases. In particular, the histological analysis revealed a microscopic picture of enthesopathy characterized by degenerative changes, including thinning, fragmentation and tearing of collagen fibers, increased cellularity, and vascularization and focal areas of ossification along with chronic inflammatory infiltrates (Fig. 15.5).
Fig. 15.4
(a) Standard LL radiograph showing a small avulsion fragment from the olecranon (arrow) named “flake sign.” (b) Figure showing the presence of dystrophic calcification in the context of the triceps tendon, which represents a sign of tendon degeneration
Fig. 15.5
Histological sections of a ruptured tendon showing (a) increased cellularity and vascularization along with chronic inflammatory infiltrates and (b) the presence of metaplastic osseous and cartilaginous inclusions
MRI and ultrasonography may prove useful in challenging cases and in preoperative planning to determine the location and extent of the tear [40–42]. Axial and sagittal MRI is considered the gold standard because it accurately demonstrates the integrity of the triceps tendon [2, 16, 43, 44]. Furthermore, MRI can distinguish between both partial and complete rupture and superficial and deep tears of the triceps tendon and can assess retraction degree of completely torn tendon. Partial rupture is characterized by a small fluid-filled defect within the distal triceps tendon (bright area on T2-weighted images), with edema extending to the surrounding subcutaneous tissues. Complete rupture of the triceps tendon is instead characterized by a large fluid-filled gap between the distal end of the triceps tendon and the olecranon process [42]. The distal edge of the torn tendon is retracted and yields heterogeneous signal intensity. In the authors’ clinical experience, T2-weighted images on the sagittal plane performed with the elbow flexed at about 90° are the sequences that provide the most reliable diagnosis.
15.6 Associated Lesions
The association between triceps tears and concomitant injuries has been described by several authors. The most frequent concomitant lesion is the radial head fracture, probably owing to the similar underlying mechanism of injury [45–47]. Levy et al. have described a series of 15 patients in whom this association was present and have found that the mechanism of trauma in the majority of patients (12/15) was a fall on an outstretched arm without direct injury to the elbow [45, 46]. Recently, Yoon et al. described a case series of four patients with particular triad injury consisting of triceps avulsion, radial head fracture, and medial collateral ligament lesion [47]. Other associated lesions include ulnar collateral ligament laxity [48], ulnar nerve compression through hematoma [18], radial nerve compression through compartment syndrome [25], wrist fracture [19], ulnar collateral ligament avulsion with flexor/pronator group injury [17], and distal humerus fracture [32].
15.7 Classification
No shared classification system for distal triceps rupture has been previously recognized. We used the Giannicola’s classification (Fig. 15.6) [49], which describes these injuries according to (1) the location of the tear (muscle belly, musculotendinous junction, tendinous body, tendon-bone insertion); (2) the depth of the tendinous lesion (superficial with the isolated involvement of lateral and long edges, deep with isolated involvement of medial edge and a combination of both); (3) the degree of the tendinous or/and muscular tear (complete or partial); and (4) the involvement of the lateral expansion (intact or torn).
Fig. 15.6
Figure showing Giannicola’s classification of triceps ruptures: (a) the tear may occur at the level of the muscle belly, musculotendinous junction, midsubstance of the tendon, or insertion; (b) the depth of the tendinous lesion may involve the superficial layer with the isolated tear of the lateral and long head tendon (superficial tear); (c) the deeper layer (medial head) may be involved alone (deep tear) or (d) in association with the superficial tendinous layer (full-thickness tear); the degree of the tendinous or/and muscular tear allows triceps lesions to be divided into either (e) partial or (f) complete tears; and (g) the extension of the lesion to the lateral expansion categorizes the tears with or without the involvement of lateral expansion
The majority of published studies have described triceps tears only as a partial or complete rupture in the muscle belly, musculotendinous junction, or tendinous insertion, thereby preventing any reliable comparison of the outcomes. A more standard classification should be adopted in future studies to allow diagnostic and therapeutic guidelines to be drawn up.
In a particular subset of patients with triceps tear, a portion of the olecranon is avulsed together with the tendon [29, 38, 50]. This is more commonly observed in skeletally immature patients in whom the ossification center of the olecranon is not fused; by contrast, proximal olecranon fracture is the most frequently associated lesion in adults. We believe that these types of injury should be classified, respectively, as detachment of the ossification center and olecranon fracture, rather than as triceps ruptures. We thus excluded these types of lesions from this chapter. Indeed, tendon degeneration, which is the main predisposing factor to these injuries, is highly unlikely in skeletally immature patients. We believe that only triceps lesions characterized by small bony avulsion fragments of the olecranon footprint (i.e., the flake sign) should be considered true triceps tendon tears in adults, because the majority of ruptures in such cases occur at the degenerated tendon insertion.
15.8 Treatment
No guidelines on the treatment of triceps tendon injuries are available, even for athletes. This is due to several factors, which include the rarity of this type of injury and the lack of a widely accepted classification. This has resulted in few studies, most of which are retrospective and with low level of evidence, and in the lack of RCTs on this topic.
Triceps tears are generally managed according to tear location and extension. Some authors have reported that the nonsurgical treatment of an acute tear affecting less than 50 % of the triceps tendon [5], along with the belly muscle, triceps aponeurosis, and lateral expansion lesions, yields satisfactory results in non-professional sports players, in the majority of cases. Other authors believe that this type of lesion warrants surgery to ensure rapid recovery of elbow function, particularly in athletes [2, 51]. A greater agreement is shown in the literature regarding the need for surgical treatment in case of complete or near-complete tears, both in low- and high-demand patients [16, 36, 52].
15.9 Conservative Treatment
Although partial triceps tendon ruptures have historically been treated nonoperatively, this is not a consensus opinion. Some authors believe that partial tears at the muscle belly and musculotendinous junction and within the tendon can be managed nonsurgically, particularly in low-demand patients [5, 19]. Bos et al. described a patient with a partial injury treated with posterior splinting of the elbow in 30° flexion for 6 weeks, followed by active motion [53]. Full ROM and normal strength were achieved, respectively, at 3 and 6 months, with the MRI at 3 months showing fibrous tissue continuity. Farrar and Lippert also reported a successful outcome in a patient whose elbow was splinted at 30° flexion for 3 weeks; full ROM and strength were achieved at 9 months [22]. Harris et al. described a patient with a 70 % right- sided rupture and a 50 % left-sided rupture, as seen at the MRI [19]. As this patient refused immobilization, arm slings were prescribed. The patient began weightlifting 4 weeks following injury and regained normal function by 41 weeks.
Other authors believe that it is not always possible to predict the healing of partial tears at the tendon insertion [54]. Although they may show healing signs initially, with reduced pain and improved function, the patient will often become symptomatic as activity levels increase; it is thus advisable to observe recovery progression over a 6- to 12-week period before deciding if delayed surgery is needed [54]. Lempainen et al. reported failed conservative treatment of a partial musculotendinous junction tear in six athletes who subsequently underwent delayed surgical treatment [55]. Delayed surgical treatment in conservatively treated partial tears has also been reported in the general population by other authors [16, 20, 29, 34, 56, 57].
Mair et al. reported that six out of ten professional football players with partial tears who were treated nonsurgically did not experience any residual pain or weakness [2]. Three players were treated by means of bracing for the remainder of the season, followed by surgery to correct residual pain and weakness, whereas one player sustained a complete rupture upon returning to play despite the bracing. Authors concluded that surgery was required in 40 % of the patients treated conservatively. This suggests that, although treatment should be individually tailored, surgery should be preferred in professional sports players, even in partial tears. Mair et al. thus recommended nonoperative management in professional sports players only in cases of tendon “strain,” in which a gradual recovery can be achieved by means of physical activity alone.
To sum up, conservative treatment may be performed in partial tears of the triceps tendon; patients may return to play after about 4–6 months, when symptoms have resolved and strength has returned to nearly normal. However, close observation of the patient is mandatory during this period to rule out any worsening of the lesion; the persistence of pain and weakness are the most negative prognostic factors.
15.10 Surgical Treatment
Primary repair is recommended in patients with acute and chronic complete or near- complete triceps tendon tears associated with a significant loss of triceps strength, as well as in complete muscle belly or musculotendinous junction with a significant gap. As above mentioned, surgical treatment may also be beneficial for acute partial tears in high-demand patients or in cases of failed nonsurgical treatment. Surgical treatment is contraindicated in patients that have serious comorbidities or are medically unstable, as well as in noncompliant patients. Although primary repair should be performed as soon as possible, it has been adopted as late as 8 months after injury [5, 16, 56]. Van Riet et al. noted good results in all eight patients who presented and underwent primary repair within 3 weeks after injury, but in less than half of the patients (6/15) who presented after 25 days [16]. These seem to suggest that an early intervention offers the best chances to perform primary repair, thereby avoiding challenging reconstruction procedures.
Several procedures have been described for primary repair, including reinsertion of triceps tendon with the trans-osseous technique and suture anchors [7, 10, 16, 18, 22, 52]. By contrast, relatively little is known about belly muscle or musculotendinous junction repair, because such lesions are extremely rare [30]. With regard to tendon insertion tears, the most investigated technique is a direct attachment with #2 or #5 nonabsorbable cross-suture (Bunnell or Krackow whipstitch technique) through cruciate drill holes through the olecranon [7, 10, 16, 18, 22, 33]. Another less common surgical procedure for primary repair is the suture anchor technique [52]. It provides the positioning of the anchors in the middle of the tendon footprint and the tying of locking stitches applied to either side of the tendon. Yeh et al. recently described the “anatomic triceps tendon footprint repair” in a biomechanical study; the authors used suture anchors to create a suture bridge (double-row) in order to restore the pre-injury anatomy and create a wider area of tendon-bone contact [10]. They concluded that this technique not only restores the pre-injury anatomy more effectively but also reduces repair-site motion compared to other types of repair.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








