Triangular Fibrocartilage Tears
24.1 Introduction
The triangular fibrocartilage complex (TFCC) is the three-dimensional link that stretches between the radius and ulna and the carpus, serving key functions of load transmission and stabilization of the ulnar side of the radiocarpal joint (RCJ) and of the distal radioulnar joint (DRUJ). The term triangular fibrocartilage (TFC) refers to the proximal component of the TFCC that represents the critical ligamentous assembly of the TFCC. The TFC combines the articular disk and the radioulnar ligament (RUL).1 The articular disk is the triangularly shaped fibrocartilage originating from the distal margin of the sigmoid notch. The RUL serves as the principal stabilizer of the DRUJ. It originates at both margins of the sigmoid notch of the radius with two bundles of densely organized connective tissue: palmar and dorsal RUL. These two bundles converge at the apex of the articular disk, then they blend together to insert onto the fovea ulnaris and the base of the ulnar styloid. The ligamentous fibers of the RUL inserting onto the fovea, particularly those of its palmar bundle, merge with the ulnocarpal ligamentous complex (UCLC). The UCLC comprises the ulnolunate, ulnocapitate, and ulnotriquetral ligaments. Its main role is to stabilize the ulnar carpus relative to the ulna and to prevent abnormal supination of the carpus. It also contributes to stabilizing the DRUJ in wrist extension and supination, providing increased tension to the palmar RUL. Taken as a whole, the compound ligamentous structure in the ulnar periphery of the TFC originates from the fovea and extends in two perpendicular planes: in the transverse plane toward the radius and in the coronal plane toward the carpus.2 Integrity of the TFC is of paramount importance for normal wrist kinematics, both in flexion-extension and pronosupination. In contrast to the TFC, the distal component of the peripheral TFCC plays a negligible role in the stability of the ulnar side of the wrist. It consists of loose ligamentous tissues, including the meniscus homologue, overlying the periphery of the TFC and the ulnar styloid.
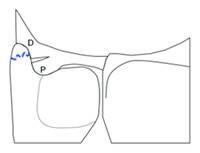
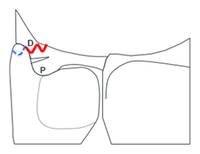
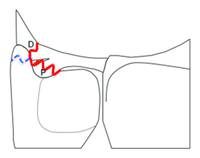
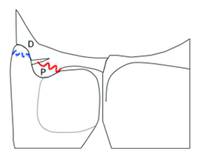
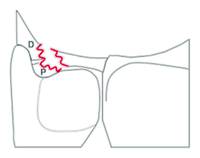
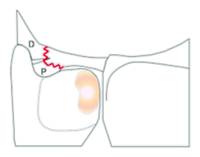
During the two last decades surgeons’ perspective on the TFCC has changed dramatically due to the increased knowledge of functional anatomy and pathomechanics and the definitive role of diagnostic arthroscopy. The earlier concept of the TFCC as the “hammock” structure of the ulnar carpus has been reconsidered and updated to the novel “iceberg” concept.3 In analogy with the iceberg (▶ Fig. 24.1), RCJ arthroscopy shows the distal peripheral TFCC as the iceberg’s “emerging” tip. On the other hand, the “submerged” part of the iceberg cannot be seen by RCJ arthroscopy, but only through DRUJ arthroscopy. The “submerged” part of the iceberg corresponds to the TFC and, particularly, to the foveal insertions of the TFCC. The larger size of the submerged part parallels the greater functional importance of the TFC as the stabilizer of the DRUJ and of the ulnar carpus, compared to the emerging part of the iceberg, that is, the distal peripheral TFCC, acting as the “shock absorbing” part of the complex. The “iceberg concept” underlines the importance of clinical assessment of DRUJ instability and intraoperative (arthroscopic) evaluation of the integrity of the foveal insertions of the TFC to improve accuracy and efficacy of either arthroscopic or open surgical repair. According to recent clinical studies on TFC repair,4,5 DRUJ instability is frequently misdiagnosed or mistreated, representing the commonest cause of poor clinical outcome. The TFC may rupture in a variable manner, as a consequence of different traumatic mechanisms, such as traction and twisting of the wrist or, more commonly, a fall on the outstretched hand (which may also cause a fracture of the ulnar styloid). Therefore, the so-called Palmer type 1-B TFCC tears should be reconsidered as a spectrum of traumatic lesions. According to clinical, radiological, and arthroscopic parameters, TFC tears may be classified as stable or unstable, repairable or nonrepairable. Following this new classification method, a new algorithm of treatment was developed to provide indications for surgical treatment and to improve comparison of outcome of the different surgical techniques.6
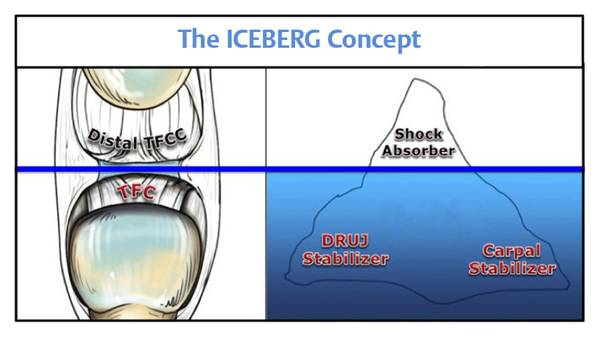
Fig. 24.1 Visual representation of the “iceberg concept” represents the functional importance of the TFC compared to the distal TFCC as well as the difficulty of assessment from standard radiocarpal (arthroscopic) exploration. DRUJ arthroscopy is required to visualize the “submerged part of the iceberg” (i.e., the foveal insertions of the TFC). The larger size of the submerged part parallels the greater functional importance of the TFC, as the stabilizer of the DRUJ and of the ulnar carpus. DRUJ, distal radioulnar joint ; TFC, triangular fibrocartilage; TFCC, triangular fibrocartilage complex.
24.2 A Comprehensive Classification of TFC Tears
A comprehensive classification that considers the different types of TFC tears, including the fracture of the ulnar styloid, should be based on clinical, radiographic, and arthroscopic findings. Six classes (0—5) are defined and provided with indications for specific treatment modalities: suture repair, foveal refixation, ulnar styloid fixation, reconstruction with tendon graft, or salvage procedures (arthroplasty or joint replacement) (▶ Table 24.1).
CLASS 0 | CLASS 1 | CLASS 2 | CLASS 3 Isolated TFC Tear | CLASS 4 NON-repairable TFC Tear | CLASS 5 DRUJ Arthritis | ||||
Clinical Findings | DRUJ Ballottement Test | Negative | Slight Laxity (Hard end-point) | Mild to Severe Laxity | Variable | ||||
Radiographic Findings | Intact Ulnar Styloid or Tip Fracture |
|
|
|
|
|
|
| |