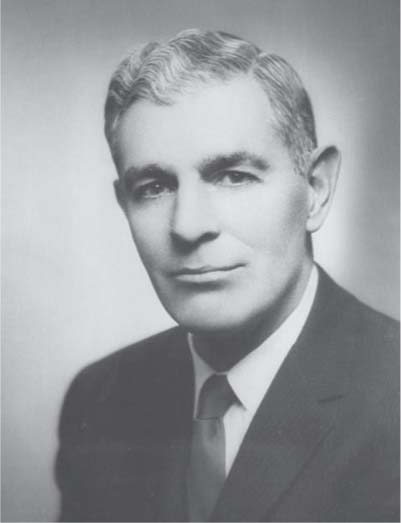
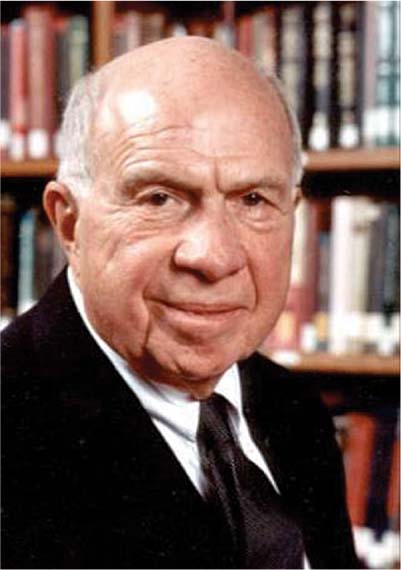
12 Treating the Rotator Cuff–Deficient Shoulder: The Columbia University Experience The New York Orthopaedic Hospital, located within New York Presbyterian Hospital, Columbia Campus, in upper Manhattan, has supported the work of great leaders in shoulder surgery throughout the 20th century, a privilege that continues today. The pedigree of the Shoulder Service is extensive; it has its roots within the renowned Fracture Service, established by Dr. William Darrach. Harrison Lloyd McLaughlin, M.D., F.A.C.S. (Fig. 12–1) began his medical career on the Fracture Service in 1935 under Darrach and established himself as a pioneer in the study of the rotator cuff (RC) and its pathology.1 With seminal studies on lesions of the RC and their surgical repair published in the 1940s and 1950s, McLaughlin staked his position as an innovative thinker in the pathology and treatment of RC disease.2–5 Although best known for his contributions to the field of shoulder instability, and, in particular, posterior dislocation, with an operative procedure bearing his name, his theories on RC pathology have served as the foundation for successive leaders of the Columbia Shoulder Service.2 In his report on 100 consecutive patients and their long-term follow-up, McLaughlin wrote, “Operative experiences soon demonstrated that no two tendon ruptures were similar or amenable to identical repair techniques, that each required a plastic tenorrhaphy suited to its own original characteristics…” He realized that the three prerequisites to a successful repair included “1) The snug apposition of healthy to healthy tissue without tension at the site of repair. 2) The restoration of continuity between the short rotator muscle bellies and the humerus. 3) The restoration of a smooth surface for articulation with the acromion…” He also suggested the impingement phenomenon in which the RC and bursa are compressed between the humeral head and acromion, which has been expanded upon by following leaders of the Columbia Shoulder Service, Drs. Charles S. Neer and Louis U. Bigliani.2 Charles S. Neer, M.D. (Fig. 12–2) is considered by many to be the father of modern shoulder surgery. Dr. Neer developed the first widely used prosthetic shoulder replacement, established the most commonly used classification of proximal humerus fractures, and advanced the management of shoulder instability.3–8 Neer created the first shoulder fellowship in the world and initiated the great legacy of the Columbia Shoulder Service. Many leaders in shoulder surgery around the world have either trained under Neer and with those whom he trained. With respect to the RC-deficient shoulder, Neer first described the radiographic and clinical features of arthritis associated with massive RC tear in 1977 and, in 1983, Neer coined the term cuff tear arthropathy in his classic paper on the subject.4,5 Neer reported on 26 patients with cuff tear arthropathy (CTA) who underwent surgical reconstruction with total shoulder replacement at Columbia between 1975 and 1983.4 He described their symptoms as “remarkably similar,” consisting of “long-standing and progressively increasing pain that was worse at night, was exacerbated by use and activity, and was made more intense by movement of the humerus against the scapula… and the patients complained of inability to elevate or externally rotate the shoulder.” Physical examination revealed swelling of the shoulder resulting from synovial fluid communicating between the glenohumeral joint and the subacromial space (the “fluid sign”), atrophy of the supraspinatus and infraspinatus muscles with corresponding weakness of external rotation (ER) and abduction, decreased active elevation (only 2 patients of 26 could actively elevate above 90 degrees), and crepitus at the glenohumeral joint line. Radiographic findings were described as “characteristic,” consisting of collapse of the proximal humerus, instability of the glenohumeral joint, loss of the acromiohumeral distance, and erosion of the superior glenoid, inferior acromion, coracoid, distal clavicle, and greater tuberosity (Fig. 12–3). Figure 12–1 Harrison Lloyd McLaughlin, M.D., F.A.C.S. Figure 12–2 Charles S. Neer, M.D. Figure 12–3 Anteroposterior radiograph of one of Dr. Neer’s cuff tear arthropathy patients. Note superior head migration and corresponding loss of the acromiohumeral interval, superior glenoid erosion creating a biconcave glenoid, erosion of the acromion, and rounding off of the greater tuberosity. At the time of surgery, Neer found a large, complete RC tear in all patients, involving the supraspinatus in all, the infraspinatus in all but one, and often involving the subscapularis and teres minor muscles as well. Instability was also common, with 14 shoulders exhibiting passive dislocation and 12 shoulders demonstrating fixed dislocation. Dramatic cartilage loss was noted, and radiographic findings of coracoacromial arch erosions were confirmed at surgery. Neer also performed histologic studies, and found that the humeral head became covered with a disordered fibrous membrane, with the underlying bone osteoporotic and hypervascular. He also found areas at points of fixed contact with the scapula that resembled changes seen in osteoarthritis with complete loss of articular cartilage and subchondral sclerosis. Finally, he found fragments of articular cartilage in subsynovial layers which resembled those found in neuropathic joints and hypothesized that these were the products of instability and subsequent abnormal trauma to the articular surfaces. Neer’s theory regarding the etiology of CTA was also put forth in this seminal paper.4 He proposed the hypothesis that the reason this condition only affects the glenohumeral joint and not other joints is because of the shoulder’s unique dependence on the soft tissue for stability and relative lack of bony constraint. He hypothesized that both nutritional and mechanical factors are important in the development of CTA: Nutritional factors imposed by the massive tear include loss of a closed joint space and impaired movement of the glenohumeral joint. The loss of a closed joint space with leaking synovial fluid under reduced pressure would be expected to deter the perfusion of nutrients into the articular cartilage. Joint inactivity has been shown to lead to structural alterations in articular cartilage as well as to biochemical changes in the water and glycosaminoglycan content of the cartilage and capsule. Both then, loss of a closed joint space and inactivity, are thought to contribute to the atrophy of the articular cartilage of the humeral head. Inactivity is also thought to cause disuse osteoporosis of the subchondral bone, in accordance with Wolff’s law, which may eventually lead to collapse of the subchondral bone… The mechanical factors include gross instability of the humeral head on the glenoid as well as upward migration of the head against the acromion and acromioclavicular joint. Loss of the stabilizing functions of the long head of the biceps following rupture or displacement of its tendon as well as of the RC contribute to at least two types of instability. Anterior and posterior subluxations and dislocations produce abnormal trauma and injury to the articular surfaces of the humeral head and glenoid. Eventually the incongruous head may erode through the glenoid into the coracoid process. The upward instability and upward migration of the head escalate the previously described process of subacromial impingement.6 Impingement wear erodes the anterior part of the acromion, the acromioclavicular joint, and the outer part of the clavicle. Instability of the head seems to be essential for the development of its collapse.4 Neer treated his 26 patients with total shoulder arthroplasty (Fig. 12–4), which is now considered to be less preferable than hemiarthroplasty due to early glenoid loosening from eccentric loading and increased lateral offset.7–14 He remarked, “surgical reconstruction of these shoulders is especially difficult.” Nevertheless, he found that only one of the 26 patients did not consider the procedure helpful. His paper first describing the entity of CTA laid the groundwork for many subsequent investigations and treatments for this previously unrecognized condition. One such subsequent investigation performed at Columbia is that of Pollock et al.7 In this study, 30 shoulders with glenohumeral arthritis and RC deficiency, which had undergone prosthetic replacement, were retrospectively reviewed at an average of 41 months follow-up. Of these, 19 had undergone hemiarthroplasty and 11 had undergone total shoulder arthroplasty. All had an attempt at RC repair. Both total shoulder arthroplasty and hemiarthroplasty had similar levels of pain relief and patient satisfaction. The most interesting finding was that, despite similar levels of pain relief, the group undergoing hemiarthroplasty displayed a significant improvement in active forward elevation (+52 versus +2 degrees) postoperatively compared with those undergoing total shoulder arthroplasty. The surgeons felt that hemiarthroplasty afforded greater ease of RC repair because the lateral offset of the humerus was decreased relative to that of total shoulder arthroplasty, and that this technical factor might be responsible for improved postoperative active elevation. Because of these findings, hemiarthroplasty has been the procedure of choice at Columbia for CTA over the past decade.
History
The Legacy of Harrison L. McLaughlin
The Legacy of Charles S. Neer, II
Treatment of Cuff Tear Arthropathy
Overview
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree