Fig. 2.1
Historical comparison of wounding patterns by conflict for major military engagements of the USA from the Civil War (1861–1865) to the present. Data for combat-specific personnel are derived from the Iraq and Afghanistan conflicts as reported by Schoenfeld et al. [19]. WWI World War I, WWII World War II, OEF Operation Enduring Freedom, OIF Operation Iraqi Freedom, GSW gunshot wound
Explosive mechanisms of injury, including improvised explosive device (IED), explosively formed projectiles, rocket-propelled grenade, and landmine, have been found to account for 75–81 % of all musculoskeletal casualties incurred in Afghanistan or Iraq [8–10, 13–16, 18–21], although the rate may be 10–20 % lower among soldiers killed in action [9] and among those directly engaged in combat [19]. The destructive force of these explosive devices creates severely contaminated soft-tissue and osseous wounds, particularly involving the extremities, in dismounted personnel (Fig. 2.2) [2, 3, 23–26]. While armor-enhanced vehicles provide more protection for vital organs and extremities, the shock wave precipitated by the blast has been associated with injury to the axial skeleton [27, 28], creating characteristic wound patterns such as low lumbar burst fractures [29] and lumbopelvic dissociation [30]. An increased enemy reliance on explosive devices in Afghanistan and Iraq has also culminated in an elevation in major amputations as compared to other modern wars, with current figures for such injuries hearkening back to rates encountered during the Vietnam era [14, 15, 20]. Even in the event that these devastating wounds can be reconstructed, limbs salvaged, or those with amputations fitted with state-of-the-art prostheses, the extent of soft-tissue damage and wound contamination associated with the initial explosive event results in a high propensity for wound-related complications to develop in the long term, including heterotopic ossification [31], osteomyelitis [24, 32], and soft-tissue contractures.


Fig. 2.2
Left leg traumatic amputation that occurred as a result of improvised explosive device (IED) blast in a dismounted soldier. The soldier also sustained right lower extremity soft-tissue wounds, abdominal injuries, and lumbopelvic dissociation. He succumbed to his injuries during emergency surgery performed in theater
Combat-Related Injuries and Wounding Patterns
The aforementioned work of Belmont et al., conducted among soldiers from a single brigade combat team deployed to Iraq, identified soft-tissue or neurovascular injuries as the most frequent musculoskeletal wound, occurring in 33 of every 1000 soldiers deployed per year (Fig. 2.3) [14]. Closed fractures were identified in 6 per 1000, while open fractures were reported in 5 per 1000. A more refined analysis, conducted using data from the DoDTR, confirmed that nearly 50 % of all musculoskeletal wounds involved the soft tissues [8]. In this investigation, fractures represented 40 % of all injuries, with those involving the tibia/fibula (7 %) and foot (5 %) as the most frequent [8]. Among several others [4, 5, 9, 10, 15, 17, 19–21, 23], Belmont’s study also highlighted a comparatively elevated rate of major amputations, pelvic trauma, and injuries to the spine [8].


Fig. 2.3
Right upper extremity wound sustained during combat in Iraq. This injury was associated with a traumatic laceration involving the brachial artery
Combat-related amputations, which are nearly entirely attributable to explosive mechanisms of injury, have been found to represent anywhere from 4 to 11 % of all musculoskeletal wounds in the current conflicts [8, 14, 20, 23]. Stansbury et al. claimed that major limb amputations (those occurring proximal to the wrist or ankle joints) comprised 5 % of all serious war injuries and 7 % of major wounds involving the extremities [20]. These authors also contended that 18 % of all amputees had more than one extremity amputation and 2 % had amputations involving both the upper and lower extremities [20]. The Army Dismounted Complex Blast Injury Task Force reported that the amputation rate among Marine Corps personnel was 1 in 206, a metric markedly higher than that encountered for Army soldiers (1 in 641) [23].
Pelvic fractures have been identified in nearly 30 % of soldiers who were killed in action, with most wounds presenting as a result of IEDs [17]. Davis et al. maintained that combat-related pelvic trauma was associated with low survival (10 %), citing major hemorrhage or the combination of shock and associated head injuries as the leading cause of mortality [17]. Ramasamy and colleagues published similar results in their series of 29 consecutive patients treated for open blast-related injuries to the pelvis [26]. While the incidence of war wounds to the pelvis has not systematically been quantified, Belmont et al. reported that 2 % of all musculoskeletal injuries sustained in battle consisted of pelvic and acetabular fractures [8].
Spinal wounds occurring as a result of combat have repeatedly been found to be present at some of the highest rates in American military history during the wars in Afghanistan and Iraq [9, 15, 16, 21]. Schoenfeld et al., examining the incidence of combat-related spinal injury in a brigade combat team, documented a rate of 7 % [15] that approximates the near 6 % incidence reported by Blair and colleagues in their longitudinal investigation using the DoDTR [16]. In another work that considered spinal injury data encountered among soldiers killed in theater, Schoenfeld and colleagues published an astonishing 39 % prevalence [9] that, when combined with the data presented by Blair et al. [16] (which excluded service members killed in theater), yields an overall estimate of 12 % for spinal trauma during the current conflicts [9]. Most spinal injuries that transpire as a result of battle seem to be commensurate with civilian spine trauma, including transverse process fractures, compression injuries, and burst fractures [9, 15, 16, 21]. A higher rate of neurologic injury (Fig. 2.4) and penetrating wounds to the cervical region have been encountered, however, particularly when compared to studies confined to civilian populations [9, 16, 21, 33]. The rate of spinal cord injury among survivors appears to be in the range of 10–20 % [8, 15, 16], while this figure may be as high as 50 % in soldiers with spine trauma who succumb to their wounds [9]. The low survivability associated with penetrating cervical spine wounds in the setting of neurologic injury has led some authors to consider such personnel as expectant in the combat environment.
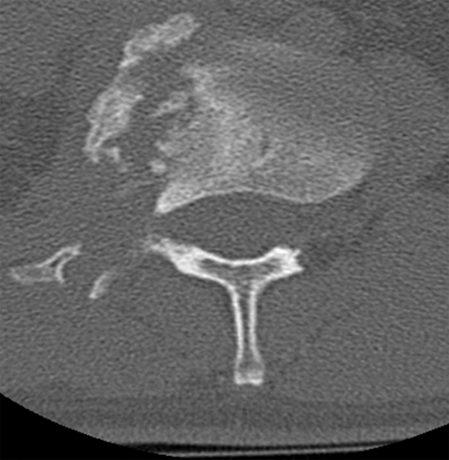
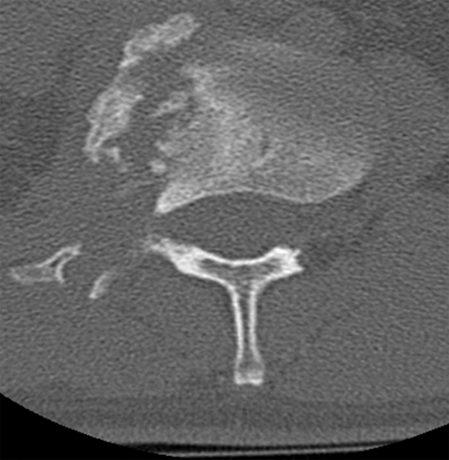
Fig. 2.4
Axial computed tomographic image of a soldier who sustained a gunshot wound to the L1 vertebrae. Besides an L1 vertebral body fracture, the bullet traversed the spinal canal precipitating a conus medullaris syndrome
Relatively rare spinal injuries, such as lumbopelvic dissociation and atlanto-occipital injury, are also seen with increased frequency among combat-injured soldiers [9]. Schoenfeld et al. reported that atlanto-occipital injury was present in 10 % of soldiers killed in theater, while low-lumbar vertebral fractures were identified in 26 % and lumbopelvic dissociation in 2 % [9]. In a retrospective review of 15 soldiers with lumbopelvic dissociation treated at Walter Reed Army Medical Center, Helgeson et al. reported that nearly all such injuries occurred as a result of explosive blast mechanisms and were significantly associated with severe wounds in other body regions [30]. Internal fixation was obviated in many instances due to the poor condition of overlying soft tissues, although when stabilization could be achieved, faster mobilization and earlier union were found to result [30]. Similar to other reports documenting outcomes following internal fixation for war trauma, these authors encountered a 13 % infection rate among those soldiers who were treated with spinal instrumentation [30].
Comparatively few works have focused on battle wounds to body regions outside of the axial skeleton, although some information regarding hand injuries is available. Fractures involving the hand comprised 5 % of all extremity injuries in the work of Owens et al. [18], and similar values were appreciated in the studies performed by Belmont and colleagues using unit-specific data [14] as well as the DoDTR [8]. A British military investigation, considering isolated deployment-related hand trauma from 2003 to 2009, reported that 73 % of 414 hand wounds required operative intervention (Fig. 2.5), with a plurality necessitating wound management, and 30 % some degree of internal fixation [31]. Nerve or tendon repairs were required in 23 % of cases.






Fig. 2.5
High-velocity gunshot wound to the hand sustained by a soldier in Iraq
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







