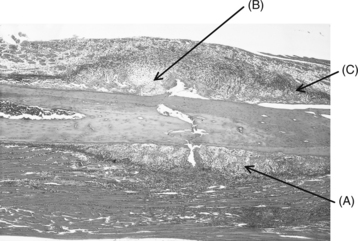
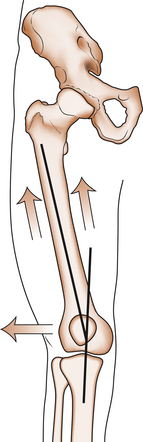
10 Andrew Ellis and Thomas Taylor • Fracture: a structural break in the continuity of bone. • Open fracture: where the overlying skin is breached, allowing communication between the fracture and the outside. Open fractures are often referred to as compound fractures but the former is the preferred and more correct term. • Closed fracture: the overlying skin is intact. • Pathological fracture: a fracture caused by normal force in abnormal bone. • Stress fracture: a fracture caused by repetitive ‘normal’ forces. • Insufficiency fracture: a type of pathological fracture occurring in osteoporotic bone, e.g. a compression fracture of the thoracic vertebra occurring in a postmenopausal woman (see Ch. 5). • Greenstick fracture: a type of incomplete fracture that occurs in children. Because of the relatively high moisture content and strength of collagen in children, bones tend to bend or fracture incompletely. The fracture looks as the name implies. • Growth plate or physis: consists of cartilage until skeletal maturity. • Diaphysis: shaft of a long bone. Consists of cortical or lamellar bone. Loads well in compression but does not tolerate torque (twisting) force well. • Metaphysis: the flare of a long bone towards the joint. Consists of cancellous or trabecular bone. • Epiphysis: the part beyond the growth plate leading up to the joint surface. Blends with the growth plate scar to form the metaphysis beyond skeletal maturity. • Dislocation: disruption of a joint such that the normally opposing joint surfaces have no contact with each other. • Subluxation: disruption of a joint such that the normally opposing joint surfaces have some contact with each other but are not congruous. Bone has a remarkable capacity to heal, far exceeding that of all other connective tissues. Unfortunately, hyaline articular cartilage has none (see Ch. 6). The inherent determination of fractures to repair is viewed as a highly efficient, primitive response to injury. Moreover, many residual deformities from fractures can remodel with time and leave no trace of the original injury. The repair process is different in cortical and cancellous bone and this is not at all surprising when one considers the functions and biology of the two tissues (summarized in Table 10.1; return to Ch. 5 to review this in more detail). Table 10.1 Features of cortical and cancellous bone In general terms, cancellous or trabecular bone is strong in compression and weak in tension. Most often its honeycomb, sponge-like structure fails in compression, for example a crush fracture of a vertebral body with excessive axial loading as sustained in a fall from a height. The tissue is compacted as the trabecular bone fails. Healing is directly between endosteal surfaces with no significant periosteal (indirect) contribution. The process is favoured by immobility (fixation) and the close apposition of the fracture surfaces. Hence, the very mechanism of injury produces circumstances conducive to healing. The rich blood supply is central to the reparative process. Non-union of a vertebral crush fracture is unknown. According to the mechanism of certain cancellous bone fractures, there may be a gap at the fracture site. A displaced metaphyseal fracture is an example of this. Endosteal bone does not proliferate to fill the defect and delayed or non-union occurs. This is the rationale of open reduction and rigid internal fixation of widely displaced metaphyseal fractures in adults. Fracture fragments are reduced and rigidly internally fixed. The reparative tissue has two components—one from the periosteum and the other produced by osteoinduction of primitive local mesenchymal stem cells. It is a highly efficient healing mechanism (Fig. 10.3). The key anatomical structures of the knee relevant to osteoarthritis were reviewed in Chapter 6. Here, we will review the anatomy of the knee joint with an emphasis on its functional anatomy relevant to musculoskeletal injury. Because of the widened human pelvis, the femur makes a coronal plane angle of 6–10° with the tibia in the fully extended position. This is relatively larger in the female because of the wider pelvis. This configuration results in a tendency for the patella to move laterally when the quadriceps muscle contracts (Fig. 10.4). This is resisted by the elevated lateral femoral condyle, which is well seen in profile. The upper surfaces of the tibial plateaus are increased in an anteroposterior direction to accommodate the flattened femoral condyles (those of the chimpanzee are much rounder). Lastly, the ACL, which becomes taut in extension, helps guide the femur medially on the tibia in the last 15° of extension—the screw-home movement. This crucial mechanism results in grooving of the anterolateral surface of the intercondylar notch and the smooth depression can be easily seen and felt in well-preserved bones.
TRAUMA AND THE MUSCULOSKELETAL SYSTEM
Introduction
Terminology
Pathophysiology
Cortical
Cancellous
Location
Diaphyseal (shaft) bone
Metaphyseal (marrow) bone(carpal, tarsal, vertebral and flat bones)
Function
Mechanical
Primarily metabolic
Cortex
Thick
Thin
Periosteum
Thick
Thin
Turnover
Slow
Rapid
Blood supply
Slow
Rich
Functional anatomy of the knee joint
General joint morphology
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


TRAUMA AND THE MUSCULOSKELETAL SYSTEM
Only gold members can continue reading. Log In or Register to continue