Total Shoulder Arthroplasty for Osteoarthritis
Patient Selection
Successful outcome depends on proper patient selection, preoperative planning, surgical technique, and postoperative rehabilitation
Most common etiologies are primary and secondary arthritis
Pathology includes osteophytes, joint space narrowing with subchondral sclerosis, and cyst formation
Rheumatoid and inflammatory arthritis and osteonecrosis are also indications
Contraindications include cuff tear arthropathy, active infection, brachial plexopathy, excessive glenoid bone loss, and Charcot arthropathy
Preoperative Imaging
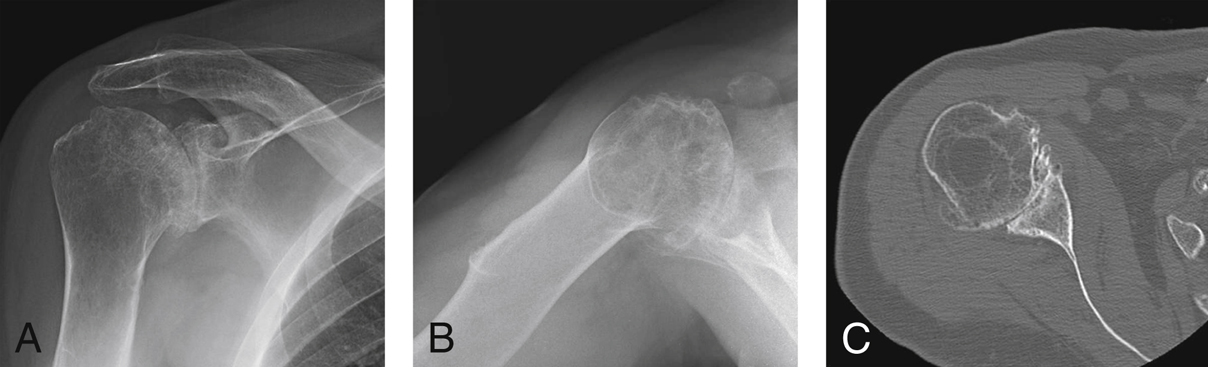
Figure 1Images obtained before total shoulder arthroplasty for osteoarthritis. A, AP radiograph of a right shoulder demonstrates loss of glenohumeral joint space, marginal osteophyte formation, sclerosis, subchondral cysts, and maintenance of acromiohumeral distance, suggesting an intact rotator cuff. B, Axillary lateral radiograph demonstrates marginal osteophytes and posterior glenoid wear. C, Axial CT cut illustrates posterior wear of the glenoid, with good glenoid vault bone stock and glenoid version.
Plain radiographs, including Grashey AP in neutral/external/internal rotation, axillary, and scapular Y views (Figure 1)
CT scans help determine glenoid version, depth of glenoid vault, and wear pattern
MRI is useful if there is concern regarding rotator cuff integrity
| Video 31.1 Total Shoulder Arthroplasty. Louis U. Bigliani, MD; Stephanie H. Hsu, MD; Howard Y. Park, BA (6 min) |
Procedure
Room Setup/Patient Positioning
Authors use indwelling regional interscalene catheter block
Give antibiotics within 1 hour of incision
Beach-chair position with head of the bed raised 30° to 40°
Position patient toward edge of table for full range of motion (ROM)
Check ROM under anesthesia.
Identify and mark relevant anatomy
Special Instruments/Equipment/Implants
TABLE 1
Instruments Used in Total Shoulder Arthroplasty
| Baby Richardson retractor |
| Darrach retractors (wide, special sharp tip) |
| Army-Navy retractors |
| High-speed drill |
| Drain/Hemovac |
| No. 1 and No. 2 nonabsorbable nylon sutures |
| Absorbable monofilament |
| Needle-tip Bovie |
| Fukuda posterior glenoid retractor/malleable retractors |
| Metal finger/elevator |
| Straight Adson |
| Flat-blade oscillating saw |
| Mallet |
| Gelpi retractors |
Total shoulder arthroplasty system of the surgeon’s choice
Additional instruments listed in Table 1
Surgical Technique
Approach
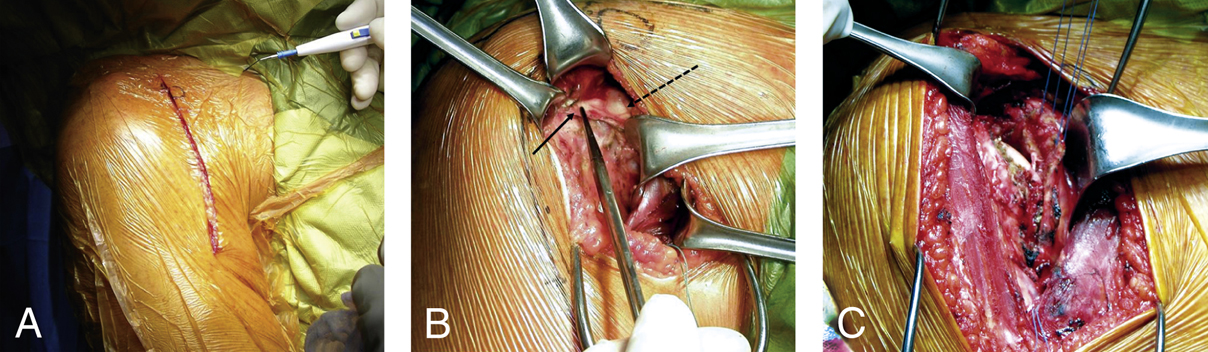
Figure 2Intraoperative photographs show the deltopectoral approach for total shoulder arthroplasty. A, The incision. B, The coracoacromial ligament is resected anteriorly for superior exposure. The solid arrow indicates the coracoacromial ligament, and the dashed arrow indicates the coracoid. C, The subscapularis tendon is carefully taken down with a needle-tip Bovie, just medial to the bicipital groove, and marked with nonabsorbable heavy suture.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


