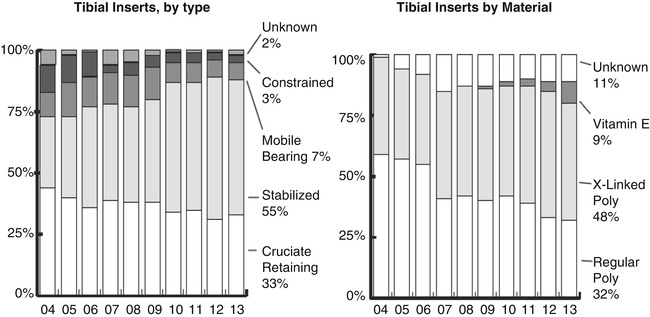
Fig. 8.1
Age distribution of all knee procedures (N = 27,158) in the United States in 2013. The mean age (66.7 years) reflects the decreasing age at which knee procedures are being performed (2013 1st Annual Report of the American Joint Replacement Registry)
The 2014 Australian Joint Registry Annual Report also supports this trend, with there being an increase in the number of total knee replacements in patients aged 55–64 years, while there is a relative status quo versus decrease in prevalence among all other age groups (Fig. 8.2).
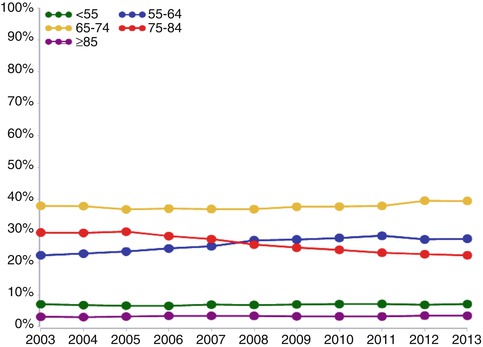
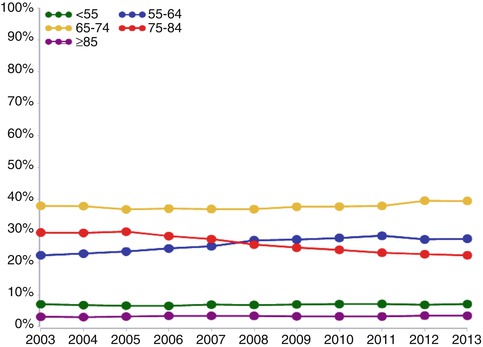
Fig. 8.2
Primary total knee replacement by age (Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA, 2014)
8.3 Survivorship
With the decreasing mean age of patients receiving total knee arthroplasties, a discussion about the durability of the components and the likelihood of the need for revision becomes paramount. In the 2014 Australian Joint Registry Annual Report [1], the cumulative incidence of revision after primary total knee arthroplasty was in the order of 2 % for aseptic loosening and 1 % for infection. When analyzing the rates of revision by age, patients less than 55 made up the highest cumulative percent revision for primary total knee arthroplasty in every year after the primary procedure when compared to groups aged 55–64, 65–74, and greater than 75 years (Fig. 8.3).
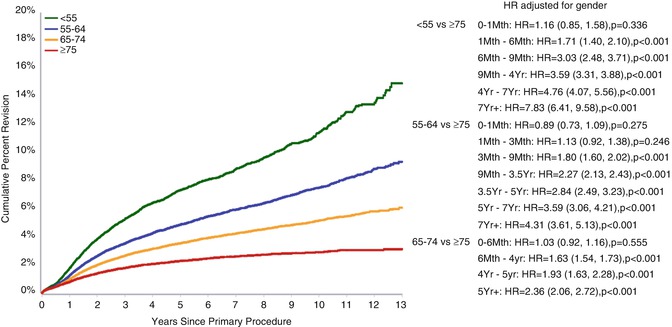
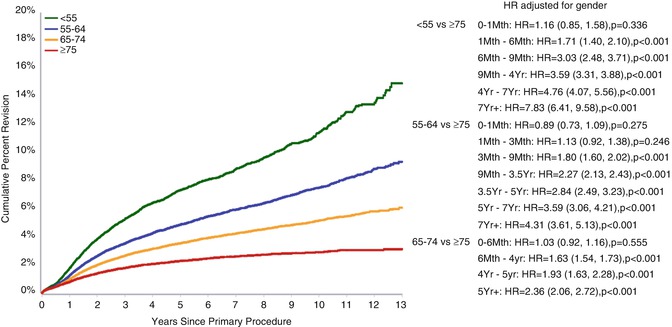
Fig. 8.3
Cumulative percent revision of primary total knee replacement for osteoarthritis by age (Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA, 2014)
When controlling for gender, the hazard ratio was greatest (7.83) when comparing cumulative percent revision for those less than 55 years to those greater than 75 years at 7+ years post primary total knee arthroplasty.
In the United States, the reasons for revision knee arthroplasty have changed over the last couple of decades. In the early 2000s, Sharkey et al. showed that the leading reasons for revision were polyethylene wear (25 %), loosening (24 %), instability (21 %), infection (18 %), arthrofibrosis (15 %), and malalignment (12 %) [2]. When looking at the time to revision, the majority (56 %) of these were early failures (less than 2 years after primary total knee arthroplasty), and among these early failures, infection was the leading cause for revision. Whereas in the late failure (greater than 2 years postprimary TKA), the leading causes for revision were polyethylene wear, loosening, and instability.
In 2010, a nationwide inpatient sample of over 60,000 patients from 2005 to 2006 revealed that infection was the leading reason for revision at 25 %, followed by mechanical loosening (16 %), implant failure (10 %), wear and lysis (8 %), dislocation (7 %), and fracture (1.5 %) [3]. In 2014, Sharkey et al. published a follow-up study comparing reasons for revision knee arthroplasty in 2012 to those in 2002, which also demonstrated that while the overall most common reason for revision was loosening (40 %), infection (28 %) was by far the most common reason for early revisions [4]. A multicenter study by Schroer et al. in 2013 found instability to be the most common reason (25.2 %) for early (<2 years since primary TKA) revision TKA, followed by infection (22.8 %) [5]. A single-center study by Le et al. in 2014 also found a similar trend with instability (26 %) and infection (24 %) as the leading reasons for early revision TKA [6].
The reasons for infection and loosening resulting in higher rates of early failure of TKA are not entirely understood and remain an ongoing area of research. Bozic et al. recently reviewed a sample of >117,000 Medicare patients from 1998 to 2010 who had revision TKA within 12 months of their index operations and found that there were a number of associated medical comorbidities and modifiable risk factors: chronic obstructive pulmonary disease, depression, alcohol and drug abuse, renal disease, and obesity [7]. Although this study was done in an older cohort, it is reasonable to infer that these same risk factors should be identified and addressed in counseling younger patients considering TKA about potential postoperative complications.
8.4 Fixation
Since the durability and survivability of components are paramount in the young, active patient who undergoes TKA, many studies have attempted to analyze whether there is an optimal fixation modality, bearing mobility, bearing material, and level of constraint for such a patient population.
Although the original cementless TKA designs had limited survivorship due to metal-backed patellae, patch porous coating, and screw holes, newer designs have comparable survivorship and functional outcomes as cemented designs. A long-term (20–30-year) follow-up study of young, active patients who underwent TKA at a mean age of 51 years revealed 70.1 % survivorship without revision. Those who had cementless cruciate-retaining components had two designs, one with 95 % survivability at 12 years and the other with 99 % survivability at 18 years [8]. A Cochrane Review of five randomized, controlled trials with 297 patients revealed that at 2 years postoperatively, cemented TKA fixation demonstrated less displacement than cementless fixation; however, the cemented components went on to have two times the risk of future aseptic loosening compared to cementless fixation [9].
The 2014 Annual Report of the National Joint Registry of England and Wales [10] has also supported that cementless or hybrid fixation with unconstrained fixed and mobile-bearing designs has a similar probability of revision as cemented designs (Fig. 8.4a, b).
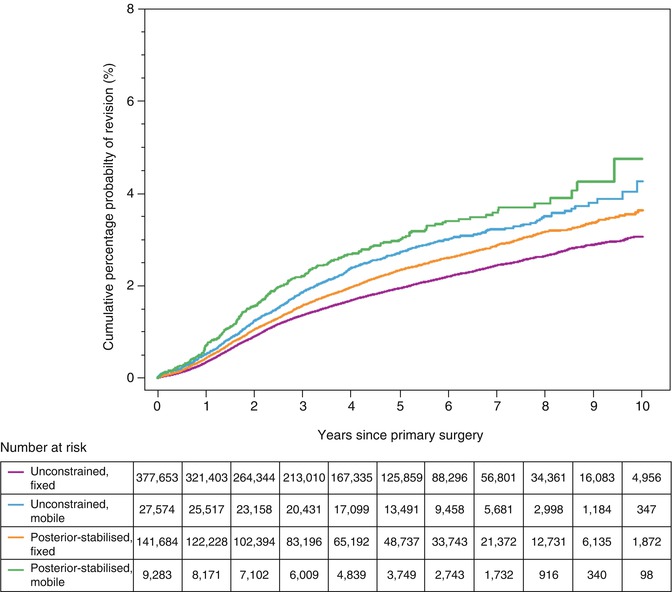
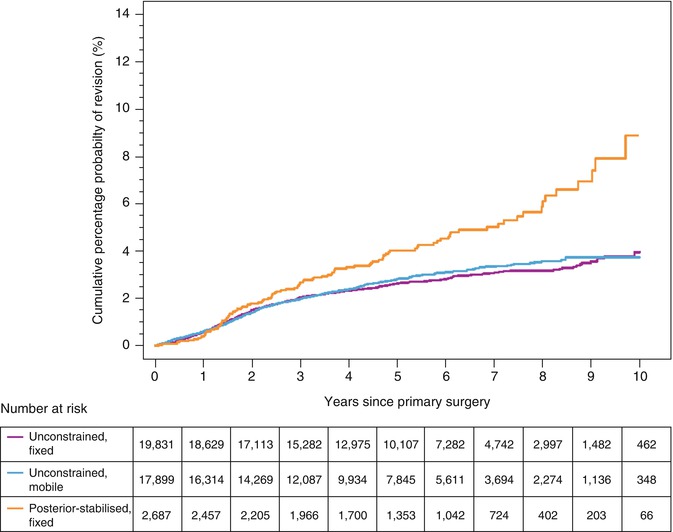
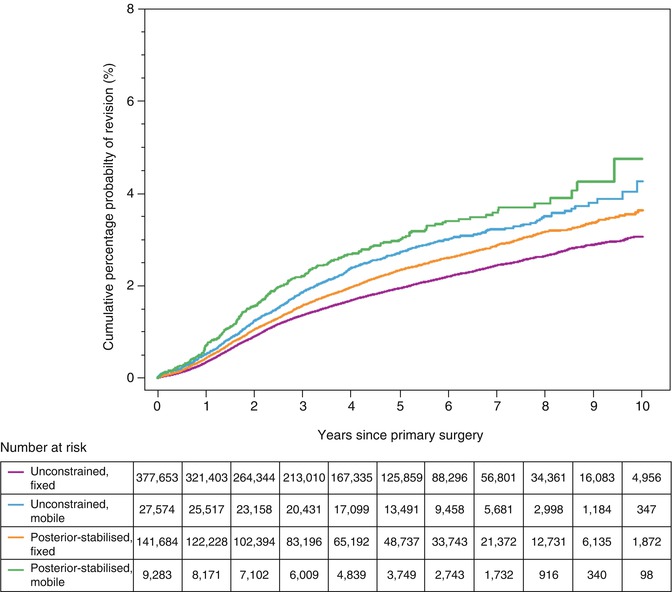
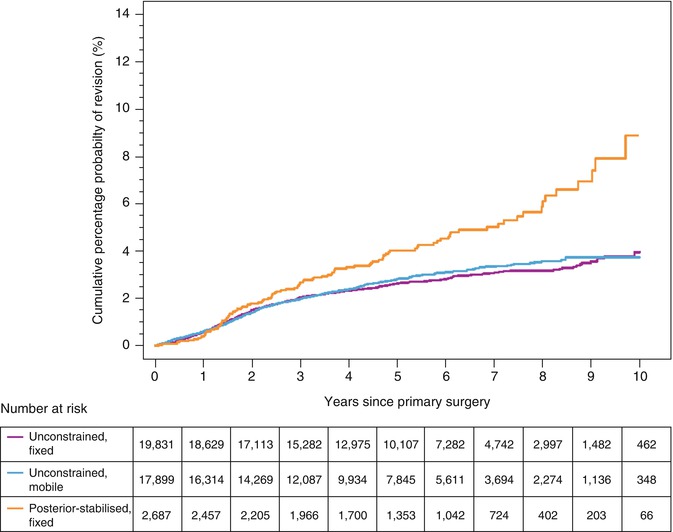
Fig. 8.4
(a) Comparison of the Kaplan–Meier cumulative percentage probability estimates of a knee prosthesis first revision for different bearing types at increasing years after the primary surgery with cemented-only fixation (2014 Annual Report of the National Joint Registry of England and Wales). (b) Comparison of the Kaplan–Meier cumulative percentage probability estimates of a knee prosthesis first revision for different bearing types at increasing years after the primary surgery with uncemented or hybrid fixation (2014 Annual Report of the National Joint Registry of England and Wales)
The 2014 Annual Report of the Australian Joint Registry reported the same finding with approximately the same cumulative percent revision of 4 % at 10 years. Thus, current data supports the use of cementless fixation, and it may be an advantageous choice in the young, active patient because of the possibility for improved long-term survivorship compared to cemented fixation.
8.5 Bearing Mobility (Fixed versus Mobile)
The primary rationale for using a mobile-bearing TKA design is to reduce wear while affording greater conformity. This sounds like an attractive option for young, active patients; however, the literature has not supported that mobile-bearing knees provide any greater function or better durability than fixed designs. Long et al. found the survivability of five fixed-bearing designs in young, active patients to range from 84 to 100 % at 9–16 years [8]. In 2014, Kim et al. published their 12-year follow-up data on 444 patients who underwent simultaneous bilateral TKA with a single manufacturer’s fixed design as well as its mobile-bearing one. They found no significant difference between designs with respect to several activity scores, range of motion, prevalence of aseptic loosening, or survival rate, which was over 97 % for both groups [11]. The 2014 Annual Report of the Australian Registry actually reported a lower cumulative percent revision for fixed-bearing designs throughout their 13 years of reported follow-up. At 10 years, fixed-bearing knees had a 5 % cumulative percent revision compared to 6–7 % among various mobile-bearing designs (Fig. 8.5).
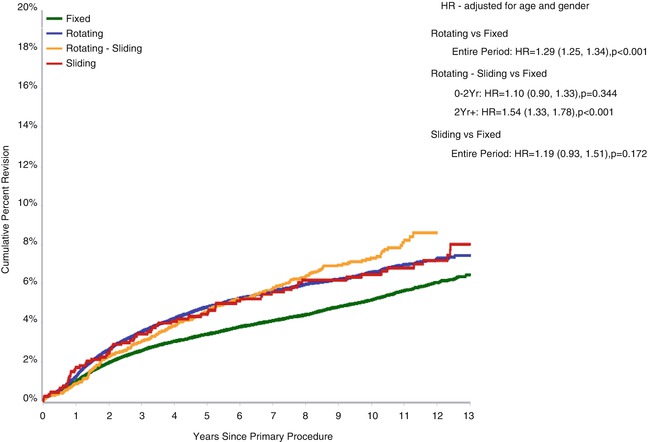
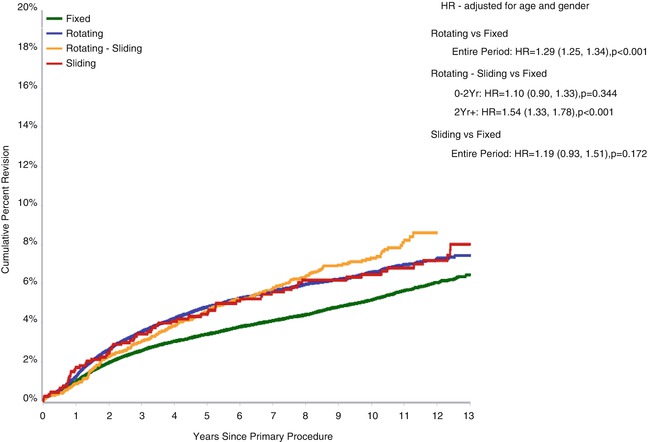
Fig. 8.5
Cumulative percent revision of primary total knee replacement by bearing mobility for patients with primary diagnosis of osteoarthritis (Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA, 2014)
Thus, the current evidence remains convincing that fixed- and mobile-bearing designs afford the same functional outcomes and survivorship.
8.6 Level of Constraint (Cruciate Retaining versus Posterior Stabilized)
The level of constraint in a primary TKA, whether it is cruciate retaining or posterior stabilized (also described as cruciate sacrificing), is another frequent concern of young patients who usually favor preserving as much of their anatomy as possible and may fear mechanically imposed limitations to their motion. A meta-analysis of 130 studies with nearly 10,000 patients with a mean 4-year follow-up of patients who had both types of constraint measured outcomes with a global rating scale [12]. This instrument measured patient outcomes in the domains of pain, function, and range of motion and combined them into a summary scale. Although patients with cruciate-retaining designs had the highest postoperative global scores and greatest global score increase from preoperatively to postoperatively, patients with posterior-stabilized designs had the highest percentage of reported good or excellent outcome (91.7 %), and there was no significant difference in outcomes between the two designs (Fig. 8.6).
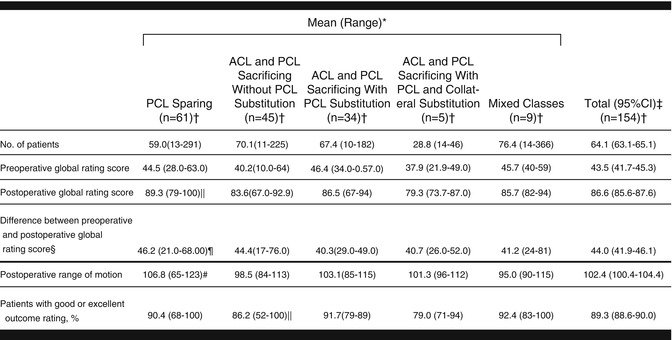
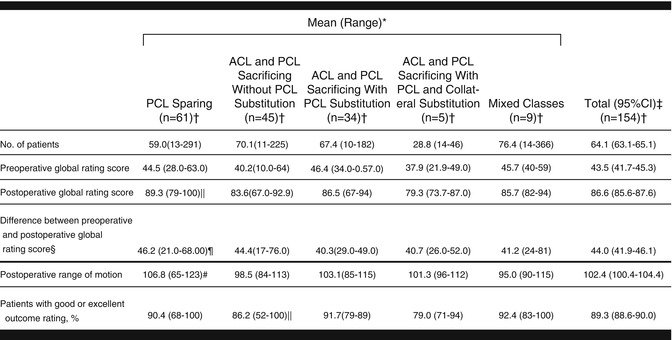
Fig. 8.6
Patient outcomes by anatomic classification of prostheses. ACL anterior cruciate ligament. PCL posterior cruciate ligament (Table 3. JAMA, 1994;271(17):1349–57)
The 2013 Annual Report of the American Joint Replacement Registry reported that the majority (59 %) of TKAs done in the United States are posterior stabilized, and there has yet to be proof of inferiority of this design warranting a practice change. In contrast, the 2014 Annual Report of the Australian Registry described a slightly higher rate of cumulative percent revision in their posterior-stabilized TKAs from 1 to 13 years postoperatively (HR 1.21, p <0.001 at 2+ years postoperatively). Nonetheless, there remains insufficient evidence to strongly recommend one level of constraint for young, active patients undergoing TKA.
8.7 Bearing Material
Over the last decade, there has been a trend in knee arthroplasty—largely inspired by the experience with osteolysis in total hip arthroplasty (THA)—that has resulted in decreased utilization of conventional polyethylene inserts in the United States (Fig. 8.7).
Currently, nearly half of tibial inserts are highly cross-linked polyethylene (XLPE), approximately one-third are conventional polyethylene, 10 % are vitamin E infused, and 11 % are unknown. Although the improved wear characteristics of XLPE were proven clearly in THA, it remains a source of debate whether this improved wear profile translates to show favorable benefit in the very different biomechanical environment of TKA. However, the 2014 Annual Report of the Australian Joint Registry Report shows evidence that XLPE in TKA demonstrates improved performance compared to conventional polyethylene. Cumulative percent revision and osteolysis as a reason for revision are lower in the TKAs with XLPE (Fig. 8.8a, b).
Fig. 8.8
(a) Cumulative percent revision of primary total knee replacement by polyethylene bearing surface (Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA, 2014). (b) Cumulative incidence revision diagnosis of primary total knee replacement by polyethylene bearing surface (Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA, 2014)
Given these data, it is reasonable to consider XLPE for use in TKA for young, active patients.
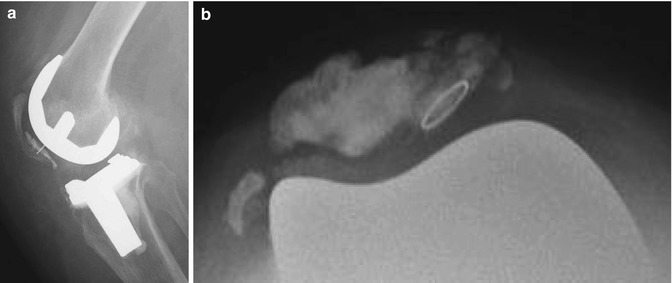
8.8 Patellar Resurfacing
Whether to resurface the patella has been a longstanding debate in TKA with wide variability in practice patterns across the world. He et al. performed a meta-analysis of 16 randomized controlled trials from 1966 to 2009 and found that there was no difference in anterior knee pain rate, knee pain score, American Knee Society score, or function score [13]. The only significant finding was that the reoperation rate was lower in the resurfacing group (p = 0.03). The arguments against resurfacing are the number of potential negative sequelae: loosening, fragmentation, avascular necrosis, lateral facet pain, stress fracture, acute fracture, late fracture, maltracking, and restricted motion (Fig. 8.9).