Tibiotalar Arthrodesis
Patient Selection
Indications
Mainstay of treatment for end-stage ankle arthritis
Posttraumatic arthritis after ankle and tibial plafond (pilon) fractures
Rheumatoid arthritis and osteoarthritis
Failed total ankle arthroplasty
Chronic ankle instability
Relative indication—severe ankle deformity (varus, valgus, or equinus)
Contraindications
Acute or chronic infection
Osteonecrosis of talar body
Osteoporosis hinders optimal fixation
Peripheral neuropathy raises risk of nonunion and infection
Preoperative Imaging
Weight-bearing AP, mortise, and lateral views of ankle
Evaluate for incongruities, joint malalignment, and signs of arthritis of subtalar joint complex
CT, MRI as needed to evaluate for bone loss, osteonecrosis, adjacent degeneration
Nuclear imaging as needed to evaluate for infection
Principles of Fusion
Rigid fixation, adequate compression, favorable biology are crucial for osseous healing and successful fusion construct
Special situations
External fixator preferred for previous infection, severe osteoporosis
Use arthroscopic or mini-open arthrodesis only for minimal deformity
Open arthrodesis appropriate for significant deformity
Nonunions, osteonecrosis of talus, and Charcot arthropathy need bone grafting, extensive débridement, possible plating
Position of ankle key to successful outcomes
Neutral flexion
5° to 10° of external rotation
5° of valgus
Optimize patient potential for healing by addressing medical comorbidities and supplementing with orthobiologics as necessary
Procedure
Patient Positioning
Supine position at edge of table
Bump under ipsilateral hip
Tourniquet on upper third of thigh
Special Instruments/Equipment
Microsagittal saw
Curets, osteotomes
7.3-mm cannulated screws
4.0- or 4.5-mm cannulated screws
Have plating system available
Surgical Technique
| Video 88.1 Tibiotalar Arthrodesis. Siddhant K. Mehta, MD; Nicholas A. Abidi, MD; Sheldon S. Lin, MD (6 min) |
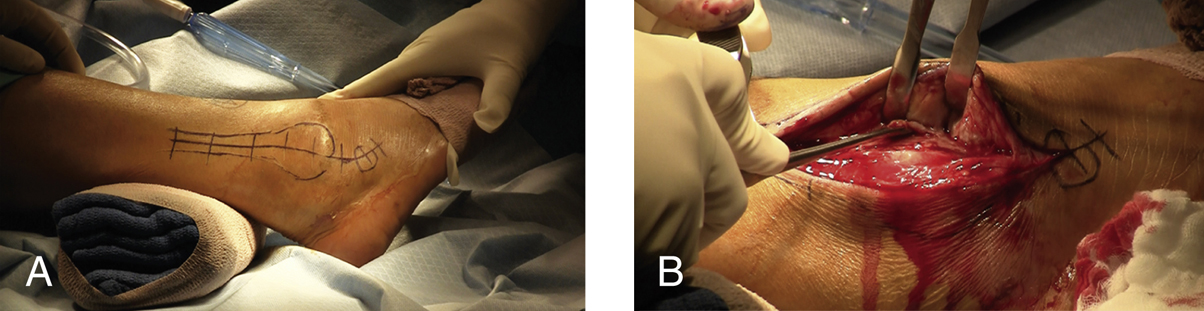
Figure 1Intraoperative photographs show ankle arthrodesis. A, The lateral landmarks and planned incision are drawn on the skin. B, The periosteum is stripped from the anterior aspect and, minimally, from the posterior aspect to fully expose the distal fibula.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


