Tibial Tubercle Transfer
John P. Fulkerson
DEFINITION
Tibial tubercle transfer is a versatile surgical alternative in the treatment of difficult and resistant patellofemoral disorders ranging from patellofemoral instability to patellofemoral arthritis.
Patients with combined instability and arthritis often benefit from tibial tubercle transfer.
Tibial tubercle transfer may be best regarded as “compensatory.” In other words, if a multiplicity of structure and alignment factors leads to patellar instability or arthritis, carefully planned repositioning of the tibial tubercle can compensate for other deficiencies, providing permanent relief of pain and instability.
ANATOMY
The patella articulates within the femoral trochlea in such a way that the distal aspect of the patella enters the trochlea from a slightly lateralized position upon initiation of knee flexion. Normally, the patella enters the trochlea promptly within the first 10 degrees of flexion, first making contact with the distal aspect of the patella.
As the knee flexes further, load is transferred more proximally on the patella such that in full flexion, contact is on the proximal aspect of the patella. The intervening flexion transfers load more gradually along the patella, moving proximally with each degree of flexion load.11
As the patella enters the trochlea with further knee flexion, the trochlea becomes deeper, so that containment of the patella is improved. Therefore, in most people, the point of greatest instability is early flexion of the knee, when the trochlea is at its shallowest and containment of the patella is most limited.
The position of the tibial tuberosity relative to the femoral trochlea further complicates the process of patella entry into the trochlea.4
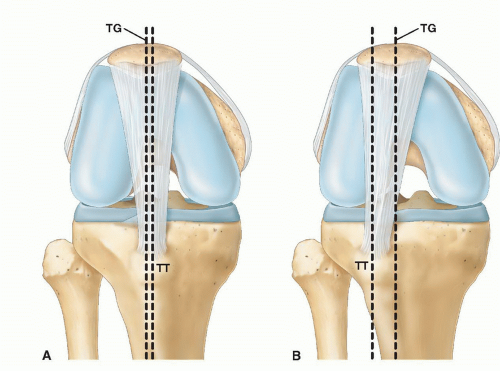
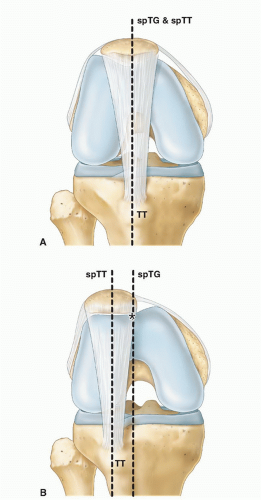
This relationship has been referred to as the tibial tuberosity to trochlear groove (TT-TG) index, measured in millimeters using superimposed tomographic images of the position of the central trochlea and the tibial tubercle (FIG 1).
The patella is contained within a soft tissue investing layer of tendon and retinacular structure.
The lateral retinaculum extends to the iliotibial band but also proximally to the lateral femur and to the tibia (the patellofemoral and patellotibial components, respectively, of the lateral retinaculum).
On the medial side is the medial retinaculum including the medial patellofemoral ligament (MPFL) and the medial quadriceps tendon-femoral ligament (MQTFL), which extends from the proximal half of the peripatellar extensor mechanism to the adductor tubercle region.1 This medial retinaculum is complex and is predominantly a blend of restraint fibers from the adductor tubercle region into the extensor expansion, not so much into the patella itself.
The patellar tendon is located distally, with the quadriceps tendon proximally connecting the patella to the quadriceps muscle. The quadriceps tendon is a massive tendon,
including a major vastus lateralis tendon component on the proximal lateral aspect of the patella.
The superolateral corner of the patella is supported dynamically by the vastus lateralis obliquus, which interdigitates with the lateral intermuscular septum.14
PATHOGENESIS
The pathogenesis of problems around the patellofemoral joint relates to dysplasia of anterior knee anatomy, malalignment, and trauma.
Most patients with significant dysplasia have a congenital underlying imbalance of the extensor mechanism and/or lower extremity, which leads to improper morphologic development.
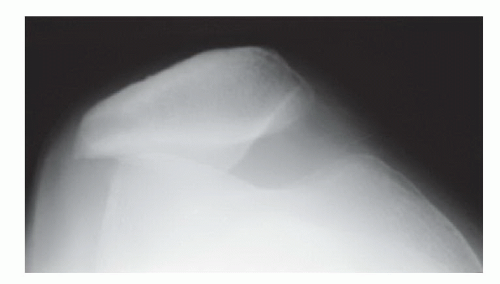
A chronically lateralized extensor mechanism is likely to cause abnormally high lateral pressure on the femoral trochlea, thereby leading to developmental flattening of the lateral trochlea and also flattening of the lateral patella (FIG 2). Although it is not always the case, this pattern of development most likely explains the poor development of the lateral trochlea, trochlea dysplasia, and persistent instability in patients with abnormal extensor mechanism alignment. Such patients stretch the medial patella support structure over time, leading to subluxation and tilt of the patella in many cases.
This stretching can lead to chronic instability, chronic overload of the lateral patellofemoral joint, dislocation (which often causes medial patella articular damage as the dislocated patella reenters the lateral trochlea forcefully after a dislocation), breakdown of the lateral patellofemoral joint, and pain related to overload of the joint and peripatellar retinacula.13
Some patients have anterior knee pain as the result of blunt trauma causing subchondral bone or retinacular injury, usually with the knee flexed.
An impact to the flexed knee and resulting trauma to the patellofemoral joint usually leads to proximal patella injury. This is important because anteriorization of the tibial tubercle shifts contact on the patella proximally and can, therefore, exacerbate a lesion on the proximal patella related to blunt injury.
Because lateral tracking of the patella is not a factor in the injury of most patients who have had blunt trauma, the problem usually is not one of abnormal extensor mechanism alignment requiring correction.
NATURAL HISTORY
The natural history of patellofemoral pain, instability, or arthrosis often relates to the imbalance noted earlier. With chronic lateral tracking of the patella in the trochlea, overload occurs with increased point loading on the patella and trochlea, particularly the patella.
Eventually, this can lead to breakdown of articular cartilage and what Ficat7 has called excessive lateral pressure syndrome (FIG 3).
Schutzer et al21 demonstrated a high incidence of patellofemoral tilt and subluxation in patients with patellofemoral pain, compared with controls.
With dislocation of the patella, the MPFL is torn and, even after healing, elongated. This further exacerbates any tendency toward lateral displacement of the patella out of the trochlea.
With blunt trauma, pain is related to impact and subchondral bone injury, generally on the proximal patella. This pain, then, originates from injured subchondral bone because there are no nerves in cartilage.
PATIENT HISTORY AND PHYSICAL FINDINGS
In the patient who may be a candidate for tibial tubercle transfer, it is important to establish that this definitive surgery truly is indicated because of a structural alignment imbalance or articular overload condition leading to instability or pain.
The physical examination should emphasize a very critical look at patella tracking within the femoral trochlea, the condition of the medial retinacular structure, evidence of focal articular breakdown of the patellofemoral joint, evidence of retinacular or soft tissue pain, and a search for other possible causes of pain such as medial or lateral compartment disease or referred pain from the hip or back.
Careful palpation of the retinacular structure around the patella will indicate whether there is soft tissue or retinacular overload contributing to pain.18
In some cases, simple release of the painful retinacular structure may be all that is needed.
When examining the medial retinaculum including MPFL and MQTFL, holding the patella laterally in extension is recommended, then slowly flexing the knee to see whether the medial supports deliver the patella into the central trochlea by 20 to 30 degrees of knee flexion. A distinct pressure, pushing the examining finger back as the patella enters the trochlea, should be encountered using this technique.
If the patella remains lateralized with the examining finger holding it lateral as the knee is flexed to 20 to 30 degrees of flexion, the medial retinacular supports are incompetent.10
Similarly, in a patient who has had previous extensor mechanism surgery, the examiner should hold the patella medially in extension and flex the knee abruptly to 30 to 40 degrees of flexion (FIG 4).
If the patella enters the trochlea very suddenly and reproduces the patient’s symptom, he or she actually may have a medial instability problem (ie, medial subluxation) that requires repair or reconstruction of the lateral support structure or even lateralization of the tibial tubercle if it previously was overmedialized.
The patella is held in the central trochlea, and the knee is flexed with compression of the patella to see if this elicits crepitus or pain. The degree of flexion at which this crepitus or pain occurs is important in localizing the location of the lesion, bearing in mind that the articulation surface of the patella moves proximally as the knee is flexed. This compression of the patella in the trochlea should be repeated as the patient extends the knee actively against resistance of the other examining hand from full flexion up to full extension, taking note of where pain or crepitus occurs with active extension against resistance.
Every patient should be examined prone so that the hip can be rotated internally and externally to see if there is a source of pain within the hip. With the patient prone, the pelvis is flat, and, therefore, flexion of the knee may be completed to compare with the contralateral side to establish whether the quadriceps and extensor mechanism are overly tight. The patient should be taught at this time how to stretch the extensor mechanism.
Nonoperative treatment should be exhausted before considering surgical intervention.
IMAGING AND OTHER DIAGNOSTIC STUDIES
In diagnosis of the anterior knee, a standardized office posteroanterior radiograph with the knee flexed 45 degrees and standardized axial radiograph of the patellofemoral joint with the knee flexed exactly to 30 or 45 degrees is very important.15
By 45 degrees of knee flexion, the patella normally is centralized in the femoral trochlea. This is a good screening test in the office to determine whether there is significant imbalance of the extensor mechanism.
Radiographs taken in more than 45 degrees knee flexion are not particularly useful in most patients.
Our practice has not found 30-60-90-degree radiographs useful.
Many patients present for evaluation with axial radiographs taken only at 90 degrees of flexion. This probably is easier for radiology technicians because they can simply hang the patient’s legs over the side of an examining table and take the axial radiograph in this fashion. It is very important to standardize flexion to 30 or 45 degrees, using a support frame as needed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree