Tibial Plateau Fractures: Open Reduction Internal Fixation
Tracy J. Watson
INTRODUCTION
Fractures of the tibial plateau involve a major weight-bearing joint covering a wide spectrum of injury, from minimally displaced intra-articular fractures to complex fractures that present with severe articular impaction, shaft extension, and soft-tissue compromise. In an effort to preserve normal knee function, the goals of treatment are to restore joint congruity, preserve the normal mechanical axis, create a stable joint, and restore knee motion. This may be a formidable task particularly in high-energy comminuted fractures with massive limb swelling and variable bone quality.
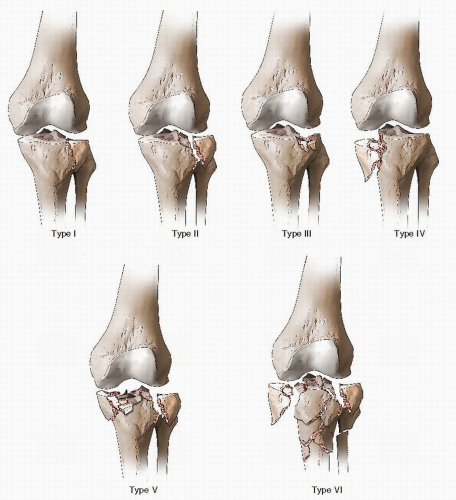
In North America, the most widely used classification schemes for plateau fractures are the AO/OTA and Schatzker classifications (1). These classifications are based on grouping fracture morphology such as condylar splits, articular depression, comminution, and metadiaphyseal extension. Schatzker’s classification divided these injuries into six distinct subtypes each with its own method of treatment (2). Additionally, dividing these into low-energy versus high-energy fractures allows one to predict the initial degree of soft-tissue compromise (3) (Fig. 27.1). This is important when planning the timing of surgery.
INDICATIONS AND CONTRAINDICATIONS
Treatment decisions should include patient factors such as age, levels of activity, preexisting medical conditions, and patient expectations as well as fracture factors such as the extent of articular involvement, fracture comminution, associated injuries, and, most importantly, the condition of the soft tissues.
The method of treatment for lower-energy tibial plateau fractures varies widely among surgeons, and numerous studies have reported satisfactory results using both nonoperative and surgical modalities particularly in the elderly (4, 5 and 6). Low-energy tibial plateau fractures that do not result in joint instability or significant malalignment of the mechanical axis can usually be treated nonoperatively. Minimally displaced fractures (<2 mm) in a patient with a stable knee joint and minimal angular deformity are usually managed without surgery
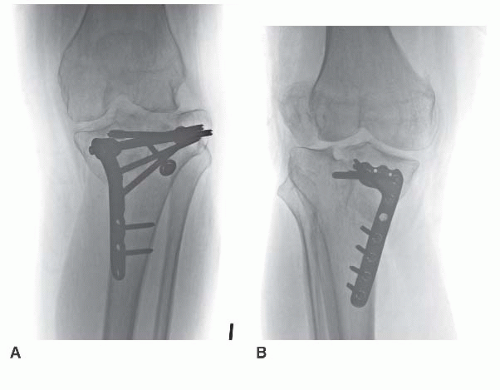
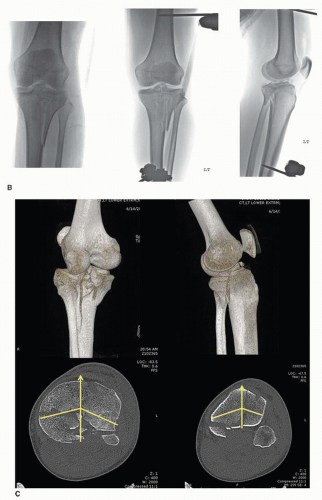
In the past 20 years, newer treatment algorithms have been developed to treat complex tibial plateau fractures that occur in patients following high-energy trauma with soft-tissue compromise. Multiple studies have shown that the ability to maintain the dynamic mechanical axis as well as an anatomic reduction correlates closely with clinical outcomes (3,5,6). In these complex fracture patterns, there is little controversy regarding the need for surgical treatment. Malunions following nonoperative treatment of displaced tibial plateau fractures are difficult to treat, and often require complex corrective osteotomies or joint arthroplasty (7). Clinical outcomes following intra-articular or extra-articular osteotomies are further compromised when posttraumatic arthritic changes have developed (Fig. 27.2). On the other hand, outcomes following properly
done initial surgery are superior to late reconstructive procedures adding increased importance to the index procedure (7).
done initial surgery are superior to late reconstructive procedures adding increased importance to the index procedure (7).
There is wide consensus that surgery is indicated for a tibial plateau fracture when there is
1. Varus or valgus instability of the knee >5 to 10 degrees with the knee examined in full extension (compared to the uninvolved knee). This indicates significant axial instability caused by articular impaction or condylar displacement (2,5,6).
2. A static or dynamic deviation of the mechanical axis, from longitudinal or axial displacement of a tibial condyle, leading to excessive varus or valgus with weight bearing.
Absolute indications for emergent surgery in tibial plateau fractures include open plateau fractures, fractures with an associated compartment syndrome, and displaced fractures in the presence of a vascular injury. Relative indications for surgery include lateral plateau fractures that result in axial joint instability, most displaced bicondylar fractures, displaced medial condyle fractures, and coronal plane posterior condylar fracture dislocations (2,3,8).
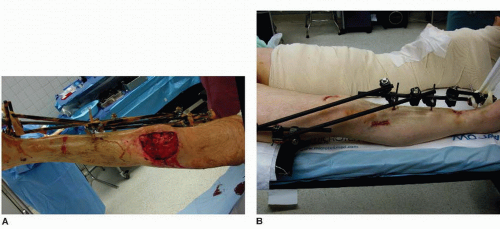
The most common contraindication to emergent internal fixation of a tibial plateau fracture is a compromised soft-tissue envelope, which can occur in either open or closed fractures. Following resolution of the soft-tissue injury, definitive fracture surgery can be undertaken with the expectation of fewer complications (Fig. 27.3). The spectrum of injuries to the tibial plateau is so great that no single method of treatment has proven uniformly successful. However, by following sound surgical principles, a congruous knee joint that is functionally stable can usually be achieved.
PREOPERATIVE PLANNING
History and Physical Exam
A patient with a tibial plateau fracture invariably presents with a painful, swollen knee and is unable to bear weight on the affected extremity. The magnitude of force delivered to the knee determines not only the degree of comminution of the fracture fragments and amount of articular impaction but also the degree of condylar and shaft displacement. Therefore, it is important to determine whether the injury occurred as the result of a high- or low-energy force.
Most low-energy fractures have a common history of a ground-level slip and fall or occur following a twisting moment resulting in a varus or valgus force to the knee and often occur in elderly patients. These are usually isolated injuries, and the patient may not seek immediate medical attention. As the degree of articular impaction increases, patients are unable to bear weight secondary to pain and instability.
High-energy fractures are the end result of a combined axial load with a rotational or angular force imparted onto the knee that is stationary. Falls from a height, head on motor vehicle accidents, pedestrian versus vehicle, and other direct impact loading mechanisms produce high-energy fracture patterns with associated soft-tissue injuries. Not uncommonly, ipsilateral injuries to the hip or lower leg occur, and many patients present with multiple system injuries.
The physical exam for all plateau fracture patterns, but especially for the high-energy plateau fractures, should document the integrity of the peripheral pulses and nerve function. Close attention to the superficial peroneal nerve is important as the inability to actively dorsiflex the foot with subjective paresthesias may be the first clinical signs of a compartment syndrome. Gentle stress testing of the knee to assess any varus or valgus instability is important, especially with lower-energy fracture patterns where instability of more than 5 degrees in full extension compared to the uninjured knee is the major consideration for proceeding to surgical management. Severe fracture patterns may occur in association with a fracture dislocation of the knee, and assessment of the cruciate ligaments often influences treatment.
The evaluation of the surrounding soft-tissue envelope should be based on objective criteria. Superficial abrasions, deep contusions, hemorrhagic blisters, and the lack of skin wrinkles all indicate a high-energy injury with some component of internal degloving. The presence of some or all of these findings usually precludes early internal fixation because surgical incisions through compromised soft tissues is associated with a significantly increased risk of wound complications and infection. If open wounds are present, their relationship to the fracture site and the knee joint must be determined (3,8, 9 and 10). Compartment pressure monitoring should be performed in selected patients particularly those with significant soft-tissue swelling, painful paresthesias, displaced medial plateau, bicondylar, and plateau fractures with shaft extension. In patients with head trauma, altered mental status, or where the physical exam is equivocal, we strongly recommend measuring compartment pressures.
In patients with absent or diminished pulses, longitudinal traction with gross realignment of the limb often restores blood flow. If a pulse deficit remains, then an ankle/brachial indices (ABI) should be obtained. ABIs consist of a systolic blood pressure obtained at the ankle over the posterior tibial artery and a systolic pressure obtained at the elbow over the brachial artery. The ratio of ankle systolic pressure divided by brachial pressure should normally be >0.9. Values <0.9 are predictive of arterial injury, and angiography with vascular surgery consultation should be obtained.
Imaging Studies and Fracture Classification
Except for very subtle plateau fractures, anteroposterior and lateral radiographs of the knee usually demonstrate the fracture. Routine radiographs should also include internal and external oblique views as well as a full-length radiograph of the entire tibia and fibula. The oblique views often detect subtle degrees of joint impaction or fracture lines not visible on the AP or lateral views.
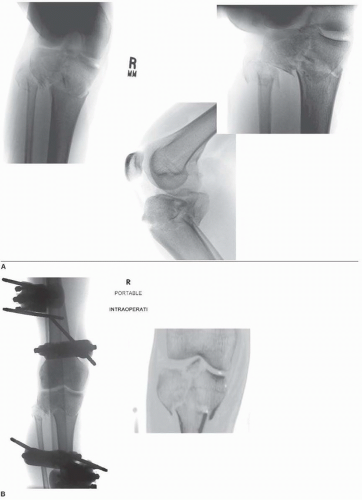
In higher-energy displaced fractures, traction radiographs are useful in improving the understanding of the fracture geometry and morphology when length is restored. Traction films may be painful to the patient and usually require analgesics to obtain in the acute setting. Distraction radiographs are best obtained after application of a bridging external fixator. Traction films aid in the preoperative planning for the location of surgical incisions based on the orientation and size of the metaphyseal fragments and depth of articular impaction.
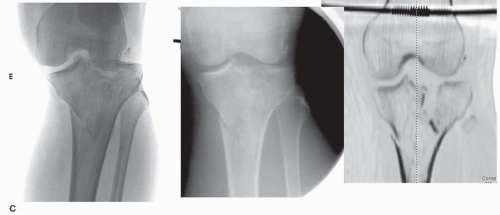
CT scans are obtained in virtually all patients with higher-energy fracture patterns (Schatzker VI, V, and VI) where plain x-rays are often difficult to interpret because of displacement, impaction, and comminution. When the plateau fracture results in axial shortening and displacement, CT scans should be performed after traction or bridging external fixation has been applied. Properly interpreted, CT scans guide the choice of surgical approach or the possibility of using percutaneous plates or screws (3,12) (Fig. 27.4).
Because of the high incidence of associated soft-tissue injuries that can occur in displaced fractures, MRI is an important tool to evaluate soft-tissue pathology (11,12). In addition to delineating the fracture and possible meniscal pathology, it can detect tears of the collateral or cruciate ligaments often seen with plateau fractures (11,12) (Fig. 27.5). Obtaining an MRI acutely may be problematic in some institutions, especially in the multiply injured patient and those with spanning external fixators. Although most contemporary external fixator components are classified as “MR compatible,” the concerns of fixation pin image distortion and heat generation may negate their use for the more complex fracture patterns, especially when spanning frames are used. Many radiology departments still consider MRI to be contraindicated in patients with external fixators. This is especially true for critically ill ICU patients.
MRI is most useful for low-energy fractures with equivocal knee stability and lesser degrees of articular involvement. The decision to operate is based on the integrity of the meniscal and ligamentous structures, which are easily defined by MRI. The MRI will also detail the extent of bony involvement much like a CT scan. We preferentially obtain MRI scans for low-energy Schatzker I, II, and III fracture patterns in ambulatory
patients when indicated. CT scans are preferred for higher-energy Schatzker IV, V, and VI injuries and in patients with spanning fixators. Very rarely will both a CT scan and MRI be obtained.
patients when indicated. CT scans are preferred for higher-energy Schatzker IV, V, and VI injuries and in patients with spanning fixators. Very rarely will both a CT scan and MRI be obtained.
CT angiography is now used to evaluate the integrity of the vascular system in patients where the ABIs are equivocal or pulses are absent. These studies are less invasive than standard angiography and can be performed quickly with less contrast. However, CT angiogram produces images that are slightly less detailed than classic angiography, but it is accurate enough to diagnose arterial compromise in most patients (12). In addition, threedimensional CT images have added another dimension in diagnostic accuracy and allows some visualization of the surrounding soft tissues (12).
Alternatively, magnetic resonance angiography does not involve radiation and uses a dye that is less likely to cause an allergic reaction or kidney damage. It is less useful in the trauma patient, particularly once a spanning external fixator has been applied.
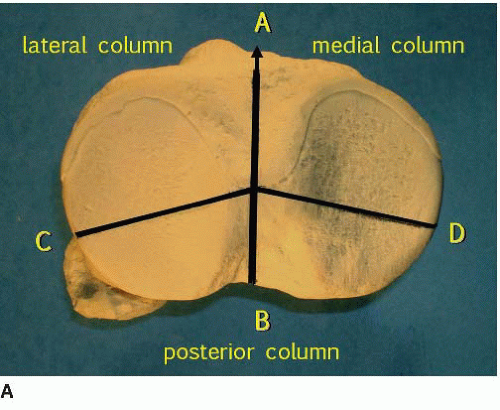
Preoperative planning is improved when the fracture can be categorized using a widely accepted classification system. The Schatzker classification appears to be useful in categorizing lower-energy fractures (types I, II, and III). However, for high-energy fracture patterns, this classification scheme has significant limitations. The Schatzker classification was developed based on plain radiographs before CT scanning was available (Fig. 27.1). However, CT scans with axial, coronal, and sagittal reconstructions provide far greater understanding of the anatomy as well as the extent and orientation of condylar fracture lines, the location, and depth of articular impaction and comminution. Both 2D and 3D CT scans have demonstrated that many fracture patterns cannot be classified or are erroneously classified by the AO/OTA or Schatzker classifications. These injuries include posterior coronal plane fractures, articular rim fractures with joint impaction, or various combinations of these injuries.
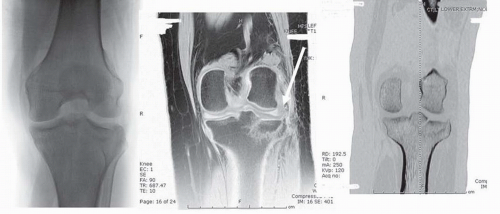
Luo et al. (13) proposed the Three Column Classification for tibial plateau fractures. This classification scheme clarifies the diagnosis and pre-op planning as well as improving the choice for the surgical approach. According to Luo classification, the transverse CT scan at the level of the plateau fracture is subdivided into three anatomic areas: the lateral column, the medial column, and the posterior column (Fig. 27.6A).
Luo proposed that one independent articular depression with a break of the column wall (condylar fracture line) is defined as a fracture of the relevant column. A pure lateral articular depression fracture is a Schatzker III injury. Luo also defined this as a “zero-column fracture.” It has only articular impaction and does NOT have a break in the lateral condylar region “column” (Fig. 27.5). Simple splits and split depression injuries such as Schatzker type I and II fractures are considered a “one column (lateral column) fracture.” When there is a split depression of the lateral condyle with an associated displaced coronal plane posteromedial condylar fracture traditionally classified as a bicondylar or Schatzker V injury, this is defined as a “two-column (lateral and posterior column) fracture.” The “three-column fracture” is defined as at least one independent articular fracture fragment in each column. The most common three-column fracture is a traditional “bicondylar fracture” (Schatzker V or VI) with a separate posterolateral articular fragment (Fig. 27.6B,C) (13).
Timing of Surgery
The timing of surgery for closed injuries is dependent upon many factors. These include the stability of the injured knee joint, the condition of the soft tissues, availability of hospital resources, and a skilled OR team familiar with the implants and instruments required for surgery. For most low-energy fractures, emergent surgery is not indicated. Appropriate imaging studies should be obtained and a preoperative plan developed. The soft tissues are not usually compromised in these fracture patterns, and aspiration of a tense hemarthrosis improves patient comfort. Schatzker I, II, and III injuries are axially stable and do not shorten significantly when placed in a well-padded compressive dressing and knee immobilizer. If the patient is comfortable and the neurovascular status is intact, they can be discharged from the emergency room with clinic follow-up. If surgery is indicated, it can be scheduled electively as soon as skin wrinkles appear, usually within 5 to 7 days. On the other hand, if the patient has significant pain, is unable to ambulate with crutches or a walker, or has other injuries, admission to the hospital is warranted.
High-energy fractures (Schatzker IV, V, VI) are not axially stable and shorten or displace when placed into a splint or a knee immobilizer. Furthermore, these injuries frequently present with compromised soft tissues,
abrasions, or skin blisters or have other associated injuries. Emergent open reduction and internal fixation is contraindicated; however, restoration of length is crucial, and a closed reduction and application of a spanning external fixator should be applied within 24 hours. The longer this procedure is delayed the less effective reduction via ligamentotaxis becomes and makes subsequent surgery more difficult. These patients require hospital admission following fixator application to monitor the neurovascular status and observe for any signs of compartment syndrome. If definitive surgery will be delayed more than 5 days, postreduction CT scans have been completed, and the patient is stable, they can be discharged if their social situation allows. Staged surgery is performed once soft-tissue recovery occurs.
abrasions, or skin blisters or have other associated injuries. Emergent open reduction and internal fixation is contraindicated; however, restoration of length is crucial, and a closed reduction and application of a spanning external fixator should be applied within 24 hours. The longer this procedure is delayed the less effective reduction via ligamentotaxis becomes and makes subsequent surgery more difficult. These patients require hospital admission following fixator application to monitor the neurovascular status and observe for any signs of compartment syndrome. If definitive surgery will be delayed more than 5 days, postreduction CT scans have been completed, and the patient is stable, they can be discharged if their social situation allows. Staged surgery is performed once soft-tissue recovery occurs.
Open plateau fractures invariably require emergent irrigation and débridement in the operating room with application of a spanning fixator especially for high-energy injuries. Repeat débridements, negative pressure dressings, or plastic surgical reconstruction may be required. Small open wounds can often be treated with sterile dressings and appropriate prophylactic antibiotics until an operating room becomes available. If the open wound communicates with the knee joint, then emergent irrigation and débridement is indicated to avoid late joint sepsis.
Surgical Tactic
There is no universal agreement on the amount of articular depression or plateau step off that dictates nonoperative or surgical treatment. Long-term studies with >20-year follow-up have indicated an inconsistent relationship between residual osseous depression of the joint surface and the development of osteoarthrosis. However, if joint deformity or depression produces knee instability, the likelihood of a poor outcome significantly increases (2,5,6). The goals of surgery and thus the surgical tactic should address the four primary areas specific to the fracture that ultimately determines prognosis. These include
A. The amount of articular depression
B. The extent of condylar displacement
C. The degree of metadiaphyseal comminution
D. Associated soft-tissue injuries MCL, ACL, etc.
A preoperative plan should address these factors and helps ensure that proper implants, reduction tools, bone graft or bone graft substitutes, and fluoroscopic equipment are available for the surgical procedure.
The surgical tactic begins by analyzing the location of the major metaphyseal fracture fragments as well as location of articular impaction. Specifically, the condylar fracture area identifies the “apex” exit point as the primary determining factor where fixation hardware should be placed. Buttress and antiglide plates must be centered over these apices’ to maintain the reduction and avoid late condylar displacement. This assessment determines the placement and location of the surgical incisions. This may require posteromedial, direct posterior, or posterolateral surgical approaches, in addition to the more common anterolateral and medial approaches. This gives the surgeon 360-degree access to the entire proximal tibia.
The majority of plateau fractures involve the lateral condylar surface (lateral column), and an anterolateral parapatellar incision is used. The length of incision depends on the specific fracture pattern and varies from patient to patient.
With medial condyle and combined column fracture patterns, the preoperative CT scan determines the need and location of a second incision (Schatzker IV, V, VI). Occasionally with a posterior column injury (“fracturedislocation of the medial condyle”) (4), the apex of the fracture line is oriented directly posteriorly, which requires a direct posterior approach for exposure and fixation (14,15).
Equipment requirements for most patients should include small fragment plates and screws (3.5/2.7 mm) as well as proximal tibial precontoured plates. These are useful because they have a low profile and anatomically match the proximal tibial. However, in very large or obese patients and those with substantial comminution, 4.5/5.0-mm implants should be available (16).
In depressed fractures that require articular reduction but have minimal condylar displacement, an anatomic precontoured nonlocking buttress plate is indicated, assuming that the bone quality is adequate. Bone on bone apposition of the condyle provides an inherent buttress and resists axial displacement. A locking plate is not required in length-stable fracture patterns.
Precontoured locking plates offer potential advantages in certain fracture patterns including increased holding power in osteopenic bone, the ability to successfully bridge severely comminuted metadiaphyseal areas, and most importantly prevent unwanted cantilever loading. Most preshaped plating systems allow for the use of both locking and nonlocking screws.
A step-by-step written problem list with a simple drawing outlining the reduction and fixation tactic is very helpful for residents and less experienced surgeons. This simple exercise summarizes the exposure, hardware requirements, and fixation strategy PRIOR to the actual event, and facilitates the case by doing the surgery on paper first.
A full complement of fracture-specific reduction clamps is necessary as these are designed specifically to apply linear compression to both condyles. A femoral distractor and/or external fixator components should be available to provide consistent ligamentotaxis throughout the case.
SURGERY
Positioning
Unless there is a medical contraindication to general anesthesia, this is our anesthetic technique of choice. General anesthesia provides more consistent muscle relaxation and facilitates better patient control when the patient is positioned in a prone position. Additionally, it avoids masking an evolving compartment syndrome that has been reported when long-acting regional anesthesia is used. Following the induction of anesthesia, the patient is positioned either supine or prone, depending on the location of the fracture. I prefer a radiolucent operating table with the involved leg elevated on a bean bag positioner (Fig. 27.7A). Once the patient is draped, multiple sterile bolsters can be used to further flex the knee if necessary. Some surgeons prefer a table that can “break” so that the knee can be flexed (Fig. 27.7B).
For some fractures, the patient is positioned in a “floating position,” with the patient primarily in a modified medial or lateral decubitus position to allow for an initial anterolateral or posteromedial approach. By rotating the leg, a second posterolateral or modified posterior incision can be accomplished (13) (Fig. 27.7C). The advantage of the bean bag for use with the “floating position” is that once the initial procedure has been completed, the bean bag can be deflated, and the leg rotated to accommodate a secondary approach.
Skin Prep and Drape
A tourniquet is placed on the upper thigh with a steridrape at the tourniquet margin (Fig. 27.7C). The limb is prepped from toes to tourniquet. For more extensive approaches, the limb is prepped from toes to umbilicus, and a sterile tourniquet is placed on the upper thigh.
The tourniquet is inflated for the primary exposure. Once completed, the tourniquet is deflated and hemostasis achieved. The majority of the fixation and the bulk of the case is then performed without tourniquet control.
Imaging
The C-arm image intensifier should be brought in from the contralateral side. Preliminary images should be obtained prior to prepping and draping to ensure that high-quality AP, lateral, and oblique fluoroscopic images
are easy to obtain without interference from the table. The entire extremity is then prepped and draped as noted above (Fig. 27.7A).
are easy to obtain without interference from the table. The entire extremity is then prepped and draped as noted above (Fig. 27.7A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree