Tibial Plateau Fractures: Open Reduction Internal Fixation
J. Tracy Watson
Donald A. Wiss
Indications/Contraindications
Fractures of the tibial plateau involve a major weight-bearing joint and may alter knee kinematics. Fractures range from minimally displaced intra-articular injuries with minimal soft-tissue embarrassment to fractures with significant soft-tissue compromise, bicondylar and shaft involvement, and extensive articular disruption. In an effort to preserve normal knee function, the physician must strive to restore joint congruity, preserve the mechanical axis, ensure joint stability, and restore knee motion. These goals may be difficult to accomplish in the face of compromised soft tissues, variable bone quality, and multiple medical comorbidities.
When considering operative management of a tibial plateau fracture, the surgeon should individualize treatment with respect to a variety of factors, such as the patient’s age, preexisting levels of activity, medical conditions, and expectations. With regard to injuries, the surgeon should consider the extent of fracture comminution and joint impaction, associated injuries, and most important, the condition of the soft tissue.
The preferred treatment and specific methods of fixation of low-energy tibial-plateau fractures varies widely among surgeons. Numerous authors have reported satisfactory results using both nonoperative and surgical methods for treatment of low-energy tibial-plateau fractures in the elderly and others (1,2,3). Low-energy tibial-plateau fractures that do not result in joint instability, mal-alignment of the mechanical axis, or axial deformity are best treated nonoperatively.
Contemporary fixation techniques have been developed to improve outcomes in the treatment of high-energy fractures, particularly fractures that occur as a result of high-energy trauma with severe soft tissue compromise in a young patient population. For these complex fracture patterns, little controversy exists regarding the need for operative management. Absolute indications for surgery in these situations include open plateau fractures, fractures with an associated compartment syndrome, and fractures with a vascular injury. Relative indications for surgery include most displaced bicondylar
fractures, displaced medial condyle fractures, coronal-plane posterior condylar fracture-dislocations, and lateral plateau fractures that result in axial joint instability (4–8).
fractures, displaced medial condyle fractures, coronal-plane posterior condylar fracture-dislocations, and lateral plateau fractures that result in axial joint instability (4–8).
The most common contraindication to emergent open reduction internal fixation (ORIF) is a compromised soft-tissue envelope, which can occur in either open or closed fractures. For those fractures, a ligamentotaxis reduction with the application of a temporary external fixator is strongly recommended (7,8). Following the resolution of soft tissue swelling, definitive open techniques that decrease the risk of complications can be undertaken. The spectrum of injuries to the tibial plateau is so great that no single method of treatment has proven uniformly successful. However, by following the principles of sound operative management, a congruous and stable knee joint can be achieved.
Preoperative Planning
History and Physical Exam
A patient with a tibial plateau fracture invariably presents with a painful, swollen knee and is unable to bear full weight on the effected extremity. The magnitude of force delivered to the knee determines the severity of fracture comminution, the amount of articular impaction, and the degree of condylar and shaft displacement. Therefore, the surgeon should determine whether the injury occurred as the result of a high- or low-energy force.
On physical exam, the doctor should focus on the integrity of the soft-tissue envelope particularly following high-energy injuries. Superficial abrasions, deep contusions, hemorrhagic blisters, and massive swelling indicate a severe soft-tissue injury. The presence of some or all of these findings precludes early ORIF techniques. If open wounds are present, their relationship to the fracture site and the knee joint must be ascertained. These areas should be avoided if a surgical approach is to be undertaken (8).
Following high-energy injuries, the peripheral pulses and nerve function as well as the status of the compartments should be evaluated and documented. Compartment pressure monitoring should be done in many patients with high-energy fractures, especially displaced medial plateau, bicondylar, and plateau fractures with shaft dissociation.
In patients with absent or diminished pulses, ankle/brachial indices (ABI) should be obtained. ABIs consist of a systolic blood pressure obtained at the palpated ankle over the palpated posterior tibial artery and a systolic pressure obtained at the elbow over the brachial artery. Under normal circumstances, the ratio of ankle systolic pressure divided by brachial pressure should be greater than 0.9. Values less than 0.9 are indicative of arterial injury, and formal angiography is indicated to determine the level of arterial disruption.
Imaging Studies
Except for very subtle joint injuries, anteroposterior (AP) and lateral radiographs of the knee usually indicate a plateau fracture. Routine radiographs should also include internal and external oblique views. The oblique views often allow physicians to detect subtle degrees of joint impaction or fracture lines not visible on the AP or lateral views.
Traction films are useful in highly comminuted and displaced fractures. Contemporary techniques require the surgeon’s precise knowledge of the three dimensional anatomy of the fracture and ligamentotaxis effect; therefore, use of distraction or traction films is helpful in preoperative planning. Computed tomography (CT) scanning with axial, coronal, and sagittal reconstructions is still the image study of choice to delineate the extent and orientation of condylar fracture lines as well as to determine the location and depth of articular comminution and impaction. With low-energy fractures in stable patients, the CT scan can be obtained in a routine preoperative setting. However, for high-energy fractures that require early, spanning, external fixation, the CT scan should be obtained following the distraction treatment. Properly interpreted, CT scans can often influence the choice of surgical approach, including the location of surgical incisions and the insertion points of percutaneous plates and/or screws (8) (Fig. 26.1).
Because of the high incidence of associated soft-tissue injuries that can occur with tibial plateau fractures, magnetic resonance imaging (MRI) scans can be very helpful. MRI has been shown to be superior to CT scans in assessing soft-tissue injuries. In addition to delineating the fracture and possible meniscal pathology, MRI can detect associated soft-tissue lesions such as tears of the medial collateral ligament or anterior cruciate ligament, which are often seen with lateral plateau fractures. Likewise, tears of the lateral collateral or cruciate ligaments associated with fractures of the medial plateau can be detected through this imaging modality (Fig. 26.2) (9,10).
A preoperative plan and surgical tactic help ensure that the proper implants, reduction tools, bone graft (or bone graft substitutes), and fluoroscopic equipment are available for the surgical procedure.
We stratify tibial plateau fractures according to the Schatzker classification in which these injuries are divided into six distinct subtypes and associated treatment principles (6). In addition, dividing these fractures into low-energy versus high-energy injuries may help in determining the initial degree of soft-tissue compromise (8). Depressed articular fragments will not reduce by manipulation, traction, or ligamentotaxis techniques alone. If articular impaction and subsequent defects are sufficient to produce axial joint instability or mechanical axis deviation with weight bearing, the joint surface should be surgically elevated and supported with graft material and fixation hardware (6). Therefore, the surgical tactic and location of incisions must optimize exposure and reduction techniques.
Surgery
There is no universal agreement on the amount of articular depression or step off that dictates nonoperative or surgical treatment. Long-term studies with greater than 20-year follow-up have shown an inconsistent relationship between residual osseous depression of the joint surface and the development of osteoarthrosis. However, if joint deformity or depression produces knee instability, the likelihood of a poor outcome is significantly increased (2,3). When forming the goals of surgery, the physician must address the factors that are thought to determine outcomes:
integrity of the soft tissue envelope,
the degree of articular depression,
the extent of condylar separation or widening, and
the degree of diametaphyseal comminution and shaft dissociation association.
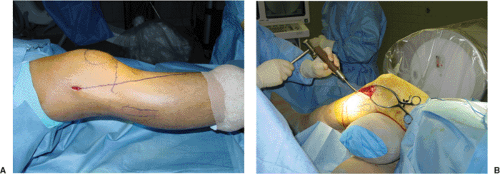
Surgery is performed with the patient under general or spinal anesthesia positioned supine on a radiolucent operating table. Some surgeons prefer a table that has the ability to break so that the knee can be flexed to approximately 90 degrees. We prefer a large bolster or a bean bag patient positioner to elevate the operative extremity when placed under the ipsilateral hip; it allows the knee to be flexed to 90 degrees intraoperatively. A C-arm image intensifier is positioned on the contralateral side. Trial images should be obtained prior to prepping and draping to ensure that accurate AP, lateral, and oblique fluoroscopic images are easily attainable without interference. The entire extremity is then prepped and draped from toes to groin. If an iliac crest bone graft is planned, then the ipsilateral crest is also included in the initial prep and a sterile tourniquet is utilized (Fig. 26.3).
Contemporary implants include 2.7-mm and 3.5-mm low profile sizes, which are precontoured to match the proximal tibial condylar anatomy. The large 4.5-mm and 6.5-mm implants are used less frequently today. Peri-articular plates require less exposure than do their predecessors. Because the majority of plateau fractures involve the lateral condylar surface, a variant of a lateral parapatellar incision is most commonly used for most lateral plateau fractures. This incision can be utilized at its proximal extent to expose only the lateral condyle, but it can also be easily extended proximally and distally when more exposure is needed, such as in an Schatzker V or VI injury.
With medial condylar fractures, the orientation and apex of the medial fracture line determines the location of a possible medial incision. Thus a medial or posteromedial incision may be necessary when treating specific, isolated, medial condylar (Schatzker IV) or bicondylar fracture patterns. With fracture dislocations of the medial condyle in the coronal plane (1), the apex of the fracture line is sometimes oriented directly posterior. In these cases, a direct posterior exposure may be required for fracture stabilization (11).
Treatment of Specific Fracture Types
Schatzker Type I
A split or wedge fracture of the lateral tibial plateau is often amenable to a percutaneous fixation (Fig. 26.4). A preoperative MRI should be obtained to assess the integrity of the lateral meniscus. If the meniscus is intact, a closed reduction and percutaneous fixation with cannulated screws or noncannulated cortical screws may be performed (9). Applying longitudinal traction with a varus force may improve the reduction. As an alternative, a laterally based femoral distractor can be used to restore length and alignment through ligamentotaxis. When an acceptable reduction is obtained, the fracture is held with a large pointed forceps placed percutaneously on the medial and lateral condyles to compress the fracture line. Fixation is usually accomplished with two or three 6.5- or 7.0-mm screws placed through small stab incisions, or occasionally through use of multiple 3.5-mm cortical screws (12). The orientation of these screws should be determined preoperatively and based either on the MRI or CT scan (Fig. 26.5).
If the preoperative MRI demonstrates a peripheral meniscal tear or incarceration of the meniscus within the vertical fracture line, or if a closed reduction fails to reduce the fracture adequately, ORIF with meniscal repair or excision is indicated.
In comminuted fracture patterns, when direct cortical apposition (i.e., bone on bone stability following reduction) is not found, a laterally directed buttress or antiglide plate should be used instead of solitary, multiple, lag screws.
Schatzker Type II
Schatzker type II injuries involve a lateral condyle fracture combined with varying degrees of articular surface depression (Fig. 26.6). Preoperative imaging studies are important to determine the degree and location of articular impaction as well as the orientation of the apex of the condylar fracture line. In most cases, the depression is anterior or central and is best approached through an anterolateral incision. The joint surface is visualized through a submeniscal arthrotomy. The lateral menisco-tibial ligament is incised transversely, allowing elevation of the meniscus through the use of several small traction sutures or small angled retractors (Fig. 26.7). A varus stress is applied to open the joint line for visualization of the articular surface of the lateral plateau.
Following joint exposure, the knee is flexed to 90 degrees, which allows additional visualization of the joint surface because the joint is distracted via the weight of the leg. Alternatively a femoral distractor can be used to enhance joint visualization through sustained distraction.
Impacted articular fragments can be reduced by two different techniques. In one method, the condylar fracture line is wedged open like a book. The articular depression is directly visualized and an impactor is inserted from below to disimpact and elevate the




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree