Talus Fractures: Open Reduction Internal Fixation
Paul T. Fortin
Patrick J. Wiater
Indications/Contraindications
Displaced talus fractures are uncommon but devastating injuries. Because they are seen infrequently, most surgeons have limited experience managing these fractures and their sequelae. Two thirds of the talus is covered in articular cartilage, and all fractures are articular injuries affecting one or more of the adjacent joints. Operative treatment is usually necessary to restore hind foot anatomy and mechanics, as well as joint congruity in the majority of these fractures. Disruption of articular congruity and/or loss of talar length, alignment, and rotation are general indications for operative treatment. Even small residual-fracture displacement can result in a significant compromise of subtalar, ankle, or talonavicular joint function.
In general, talar neck and body fractures should be treated operatively if the fracture is displaced more than 1 to 2 mm. Talar neck fractures are classified into one of four types (Fig. 34.1). Hawkins described types I, II, and III and Canale and Kelly described type IV injuries that involve the talonavicular joint. Type I talar neck fractures are nondisplaced injuries and can be managed nonoperatively in cooperative patients who agree to frequent follow-up x-rays. Any displacement should be considered significant and usually warrants surgical intervention. Nondisplaced talar neck fractures that are not visible on plain x-rays but diagnosed with other imaging modalities, such as magnetic resonance imaging (MRI), computed tomography (CT), or bone scans, may be treated nonoperatively. Types II, III, and IV talar neck fractures are, by definition, displaced and require reduction and fixation.
Talar body fractures often involve articular disruption of both the tibiotalar and subtalar joints, and surgical restoration of articular congruity, talar height, and ligamentous stability of the ankle is usually the best option. Talar body fractures can be classified into cleavage, crush, and tubercle or process fractures (Fig. 34.2). Because of the impaction mechanism of many of these injuries, anatomic reduction of the joint surface is not always possible, but restoration of height and stability of the hind foot is indicated to help diminish long-term complications.
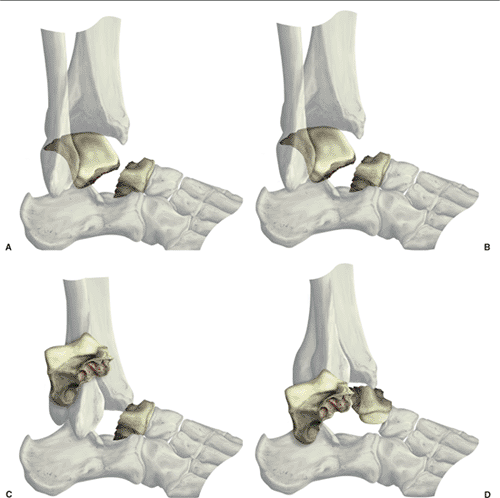 Figure 34.1. Hawkins classification of talar neck fractures. A. Type I. B. Type II. C. Type III. D. Type IV. |
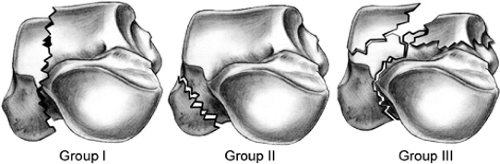 Figure 34.2. Talar body fractures. A. Group I cleavage fractures (horizontal, sagittal, coronal). B. Group II process or tubercle fractures. C. Group III crush with compression/impaction. |
Talar neck and body fractures are usually the result of high-energy injuries. However, talar injuries are commonly overlooked and may go unrecognized. This is particularly true in multiply injured patients, and late treatment of the talar injury often results in suboptimal outcomes. Occult foot or ankle injuries should be suspected when foot and ankle swelling or ecchymosis is presented even when obvious radiographic abnormalities are not found.
Significant neuropathy, peripheral vascular disease, soft-tissue compromise, and limited ambulatory capacity are relative contraindications to surgical management. Peripheral neuropathy is highly variable in severity, and many elderly patients have some degree of peripheral neuropathy that should not necessarily preclude operative treatment. Loss of protective sensation, however, as judged by the ability to differentiate a 5.07 monofilament, is a sensitive indicator of significant neuropathy; therefore, failure to differentiate the monofilament should be considered a relative contraindication to surgery. The decision to operate also depends upon the fracture pattern, ankle stability, and presence of dislocation or significant joint subluxation and should be made on a case by case basis. A minimally displaced talar body fracture in a patient with significant neuropathy may be best treated nonoperatively, whereas a Hawkins III talar neck fracture with posteromedial extrusion of the talar body should be treated operatively, even in patients with significant neuropathy, to relieve soft-tissue and/or neurovascular compromise. Elderly patients with limited ambulatory capacity, similarly, may be best treated nonoperatively if the joint is not significantly displaced or dislocated.
On occasion, poor soft-tissue conditions complicate the operative treatment of these fractures. For example, a dual incision approach to a talar neck fracture may be contraindicated in situations where the anterolateral skin is compromised (Fig. 34.3). Extensile exposures may also be contraindicated in patients with marginal perfusion of the extremity.
Preoperative Planning
The urgency of reduction and timing of surgical intervention for talar injuries remains controversial. Initial fracture displacement, rather than the timing of reduction, is thought to be a major factor controlling the development of osteonecrosis following talar neck fractures. Fractures associated with joint subluxation or dislocation, as well as those with soft-tissue compromise due to fracture displacement, necessitate emergent reduction to avoid neurovascular compromise and/or skin necrosis (see Fig. 34.3). Because of the urgency of expedient reduction in these circumstances, preoperative planning is invariably limited. If the peritalar joints are reduced and fracture displacement is not significant, operative fixation can be performed when soft-tissue swelling and bruising are resolving and proper imaging studies have been obtained. In most patients, a well-padded plaster or fiberglass splint provides adequate temporary support and pain relief. Provisional, spanning, external fixation to restore length and stability may occasionally be necessary when the soft-tissue status precludes early open reduction.
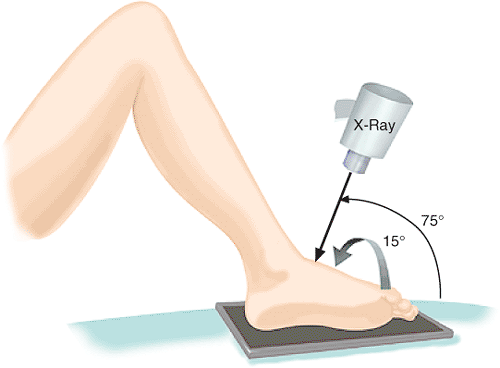
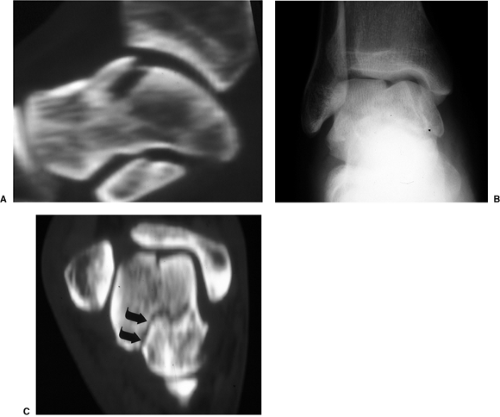
The standard radiographic evaluation for talar injuries includes anteroposterior (AP), lateral, and oblique views of the foot and ankle. The Canale oblique view (Fig. 34.4) may be helpful to assess length and alignment of the talar neck. Shortening of the medial column of the talus secondary to impaction is common in talar neck fractures and is well seen on the Canale view. CT scans are also useful in defining the fracture pattern and detecting occult fractures in the ankle and foot (Fig. 34.5). Concomitant osteochondral fractures are common with talar neck fractures and are not well visualized on plain x-rays.
Knowledge of the fracture pattern and classification is very helpful when planning the surgical approach, methods of reduction, and fixation techniques. For example, talar body fractures and type III talar neck fractures with posteromedial extrusion of the talar body often require transmalleolar exposure either through a concomitant medial-malleolar fracture or osteotomy of the medial malleolus. Reduction aids such as a femoral distractor may be necessary to reduce an extruded talar body. Chondral and osteochondral fractures often necessitate small-diameter subarticular screws or bioabsorbable implants. By definition, talus fractures are articular injuries, and having an assortment of small-diameter plates and screws will facilitate anatomic restoration of the joint surface and rigid fracture fixation to allow early motion.
Surgical Technique
Access to the talus for fracture surgery is limited, and extensile approaches are not recommended. Fracture pattern and associated soft-tissue disruptions suggest potential avascular zones. The goal of fracture surgery is to gain access to the bone for reduction and fixation without further compromise of the remaining blood supply. Unnecessary dissection should be avoided and ligamentous attachments should be protected.
X-rays are carefully assessed to determine fracture pattern, areas of comminution, medial neck shortening, and associated osteochondral fractures (Fig. 34.6). The patient is positioned supine on a radiolucent operating table with a bolster placed under the affected extremity. A well-padded pneumatic tourniquet is placed on the proximal thigh. General anesthesia with muscle paralysis is preferred to counteract potential muscular-deforming forces in the hind foot. Intraoperative c-arm fluoroscopy is utilized (Fig. 34.7).
For most displaced talar neck fractures, we prefer a dual incision technique in which anteromedial and anterolateral incisions are utilized. Visualization of both the medial and lateral talar neck regions allows for more accurate fracture reduction (Figs. 34.8 and 34.9). Oftentimes the dorsal and medial talar neck is comminuted and the lateral and plantar portion are not or visa versa.
The anteromedial incision extends from the anterior aspect of the medial malleolus to the medial cuneiform and is centered midway between the tibialis anterior and tibialis posterior
tendons (Fig. 34.10). This approach exposes the dorsomedial talar head and neck as well as the anteromedial body. Proximally, the greater saphenous vein and nerve are identified and protected. The tibiotalar and talonavicular joints are exposed.
tendons (Fig. 34.10). This approach exposes the dorsomedial talar head and neck as well as the anteromedial body. Proximally, the greater saphenous vein and nerve are identified and protected. The tibiotalar and talonavicular joints are exposed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree