Chapter 8 Tibial Osteotomy
Why osteotomy?
In 1994, the Centers for Disease Control and Prevention1 reported that by the year 2020, osteoarthritis will have the largest increase in numbers of new patients of any disease in the United States. Approximately 60 million persons aged 45 to 64 years (referred to as baby boomers) constituting 20% of the U.S. population are at risk. Total knee arthroplasty has become one of the most commonly performed procedures with reproducibly good results in the United States. This is largely due to generically designed anatomic implants with universal knee instrumentation. Prior to the development of total knee replacement, high tibial osteotomy was commonly performed. However, in 2008, 220,000 total knee replacements were performed in patients younger than 55 years, and a total of 450,000 total knee replacements were performed overall. As good as total knee replacement is, patient satisfaction remains only approximately 80%. With the inherent problems of prosthetic arthroplasty failure due to polyethylene osteolysis, mechanical loosening, joint infection, and problematic revision surgery secondary to ligamentous laxity or bone deficiency, reevaluation of joint preservation techniques led to the resurgence of osteotomy and cartilage repair surgeries as well as more bone-sparing partial prosthetic arthroplasties.
Tibial osteotomy had been a procedure routinely performed in patients older than 50 years with tibial varus malalignment and medial unicompartmental disease. In the series by Coventry et al,2 the average age of patients undergoing tibial osteotomy was 63 years. However, today it would be difficult for surgeons to perform tibial osteotomy in patients of a similar age given the reproducible long-term results with total knee arthroplasty in that age category.
However, unicompartmental arthrosis is becoming prevalent among patients in their 20s, 30s, and 40s. As baby boomers age and activity levels remain high because of their interest in sports, injuries to the anterior cruciate ligament (ACL), meniscus, and articular cartilage predispose to unicompartmental disease in patients much younger than those treated in the past. The average age of patients undergoing high tibial osteotomy for bone-on-bone medial compartment disease in my practice was 44 years.3 Unicompartmental and total knee arthroplasty cannot offer these patients long-term, high-level functional activity.
Sharma et al4 demonstrated that the risk of progression of unicompartmental osteoarthritis with malalignment is four times more common in a varus than a neutrally aligned knee and five times more common in a valgus than a neutrally aligned knee over a 18-month time course, with evidence of progression on standing radiographs. Osteoarthritis in the malaligned limb with unicompartmental disease remains a problem in the young athlete and adult. Tibial osteotomy remains the procedure of choice in the limb with unicompartmental osteoarthritis with malalignment.
A long-term Swedish study evaluating the natural course of arthrosis of the knee over 20 years noted that 61% of patients with Ahlback stage 1 osteoarthrosis (50% joint space narrowing) would have progression of disease; the remaining 39% would remain stable without further reduction in joint space.5 Fifty-seven percent of patients with Ahlback stage 0 arthrosis, defined as osteophytes or subchondral bone sclerosis with normal joint space, would not progress over time. Patients with more advanced cases, Ahlback stages 2, 3, 4, and 5, would progress over time.
Technique-related issues against high tibial osteotomy
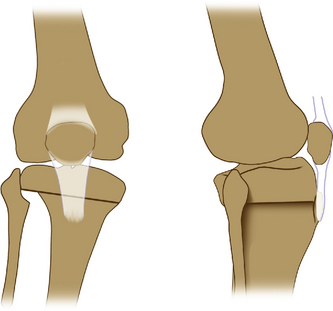
Arthroplasty surgeons have conceptual difficulty with osteotomies because of the potential for making the arthroplasty more challenging and for compromising the results of primary arthroplasty. Issues that have led to problems include placement of skin incisions, patella baja (infera)–infrapatellar tendon contracture, contracture of the lateral ligament and posterolateral corner with release of the proximal tibial fibular joint, obliquity of the joint line, and distortion of the upper anatomy of the tibia (Figure 8–1). Excessive valgus correction also has resulted in difficulty with arthroplasty balancing of the flexion–extension gap and obtaining adequate alignment and increases the risk of perineal nerve palsy. The total joint literature is abundant with reports of inferior outcomes following tibial osteotomy to primary total joint replacement. However, other investigators have reported that results are equivalent but that experienced surgeons using modified surgical techniques are needed in order to obtain results equal to those of total knee replacement as a primary procedure. If osteotomy surgery is to be pursued for cartilage repair or for treatment of instability or unicompartmental arthritis in young patients, then the eventuality of total knee replacement must not be compromised or made more difficult.
Patient-related issues
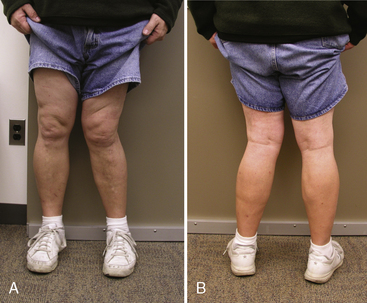
Closing wedge osteotomy with staple fixation and postoperative casting in full extension often leads to patient dissatisfaction that arises predominantly from overcorrection in valgus with cosmetic disfigurement (Figure 8–2). Release of the proximal tibiofibular joint leads to lateral laxity, which results in the sensation of a sloppy knee secondary to posterolateral ligament instability. Cast immobilization leads to difficult ambulation and return to work as well as the technique-related problems previously discussed: patella baja (infera) and lateral contracture with decreased motion. These problems can be avoided or eliminated by appropriate procedural osteotomy technique selection, patient selection, and careful preoperative and postoperative planning and care. Renewed interest in joint preservation and cartilage repair have led to innovative new osteotomy techniques that are more precise, have improved technical ease, and provide reproducible results.
Procedural planning
In a multivariate analysis of predictors of good outcome, Coventry et al2 found that long-term outcome was determined by mechanical correction to 8 degrees or more of tibiofemoral valgus and patient weight less than 1.32 of ideal body weight.2 Rinonapoli et al6 noted that longevity was proportional to the stage of disease at the time of osteotomy. Updated reports with experimental cadaveric loading have demonstrated similar findings.7 The authors found that when tibiofemoral alignment was shifted from varus to valgus alignment, decreases in medial contact pressure and medial contact area occurred. For defect chondral sizes 10 to 20 mm, all contact pressures within the medial compartment were shifted to the lateral compartment at between 6 and 10 degrees of tibiofemoral valgus. Contact pressures were found to concentrate around the defect rims for all defect sizes. From 6 to 10 degrees of tibiofemoral valgus was recommended as the optimal axial alignment favoring cartilage repair.
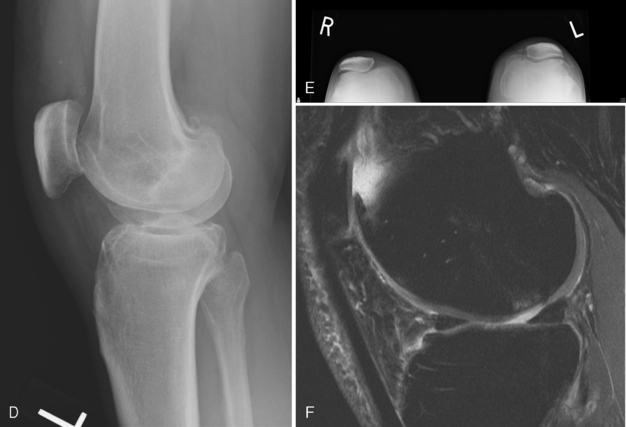
Preoperative x-rays films (Figure 8–3) include long axial alignment x-ray films on 54-inch cassettes to include the hip, knee, and talus as a standing film in extension. Rosenberg 45-degree bent posteroanterior, standing AP, lateral, and skyline films and radiograph measurements of leg length are important.
Preoperative Planning for Angular Correction of Tibial Osteotomy
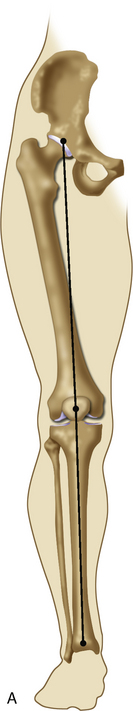
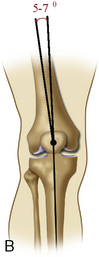
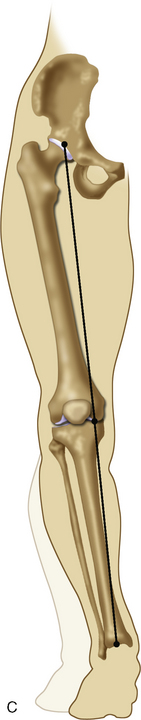
Consider the normal tibiofemoral alignment of the knee. A neutral mechanical access requires that a line pass from the center of the femoral head through the center of the knee into the center of the ankle (Figure 8–4). This assumes that the neck shaft angle at the hip joint is within normal limits, 130 to 135 degrees, and that the tibiofemoral axis at the knee is 5 to 7 degrees of valgus.
My desired angular correction for medial osteoarthritis (Figure 8–5) is to place the mechanical axis through the center of the lateral intercondylar spine or just to the downslope of this area. This is 2 degrees overcorrected from a neutral mechanical axis. It is different than the classic teaching, which recommends that the mechanical axis pass through the Kurosaka point at 62% across the width of the tibia. I believe this is overcorrected to a level that is cosmetically unacceptable to patients and alters the kinematics of the patient’s athletic endeavors so that they are difficult to perform. If the osteotomy is performed for a cartilage repair procedure with an intact joint space, the mechanical axis should pass through the center of the knee joint and should not overcorrected. In addition to the mechanical axis, consider the tibiofemoral axis. From previous basic science research, a 6- to 10-degree tibiofemoral valgus angle is sufficient to unload a medial compartment.7 If there is varus in the proximal femur, the knee alignment can be markedly overcorrected by looking only at the mechanical varus of the overall leg alignment.
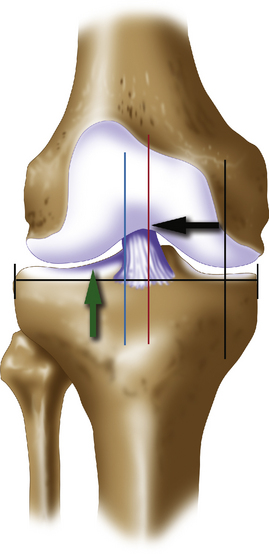
Figure 8–5 Mechanical axis correction. Classic mechanical axis correction for tibial valgus-producing osteotomy is recommended by several authors to pass through the Kurosaka point at 62% across the width of the tibia (broad green arrow).12 This results in a tibiofemoral valgus angle of approximately 10 to 12 degrees. My preference is to correct the mechanical access to the midline (red line) when correcting the varus with cartilage repair for a focal medial defect and to only overcorrect by 2 degrees to the lateral tibial spine if the patient has a very large medial femoral condyle chondral defect, “kissing” medial chondral defect, or established osteoarthritis with greater than 50% loss of the joint space on weight-bearing-x-ray films.
Assuming that the proximal femur has a normal neck shaft angle, my preferred technique for calculating the angular correction is as follows (Figure 8–6). A simple angular correction as measured on the long axial standing films is performed by passing a line from the center of the femoral head to the desired axis at the knee joint (e.g., lateral intercondylar spine). A second line from the center of the talus then intersects this same point. The acute angle between the two is the angular correction desired. Ligamentous instability of the medial complex and ACL should be assessed so that laxity, if present, can be accounted for at the time of osteotomy to ensure that marked overcorrection does not ensue.
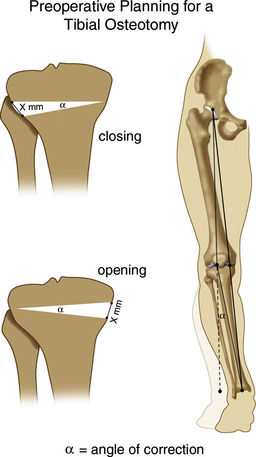
Figure 8–6 Osteotomy is a straightforward procedure when the varus is in the proximal tibial metaphysis, which is the most common situation. A line is drawn from the center of the femoral head to the desired point of correction (see Figure 8–5), in this case, the lateral tibial spine, to the proposed position of the foot, at the center of the ankle. The angle between the center of the talus and the proposed position is the angle of correction, α. Using calibrated digital x-ray films and commercially available web-based software (Centricity, General Electric, Waukesha, WI), the actual opening in the millimeters, x, can be calculated for a opening wedge osteotomy. Similarly, the exact number of millimeters for angle α for a closing wedge osteotomy can be calculated or the angle taken directly off the osteotomy closing wedge calibrated angular system, which is typical. Intraoperative check with clinical appearance of the limb after osteotomy as well as intraoperative checks with long alignment wires or rods under fluoroscopic control confirm accurate angular corrections.
Cartilage Repair, Osteoarthritis, Instability
Interest in the use of tibial osteotomy has been renewed. Patients are maintaining higher levels of fitness and aerobic activity as they age and generally wish to preserve their joints as long as possible. Newer techniques of both opening and closing wedge tibial osteotomy give predictable angular corrections with reliability. This increased technical accuracy lessens the risk of complications, make the pursuit of joint preservation more appealing for both surgeon and patient. Three broad categories of indications for osteotomy surgery presently exist. It is generally agreed that cartilage repair in the presence of malalignment usually results in failure because the source of cartilage breakdown in the first place is generally malalignment in addition to other traumatic factors such as meniscal deficiency, ACL injury, or articular cartilage injury. Therefore, osteotomy has become an adjuvant procedure that has been deemed necessary when the articular cartilage injury undergoing repair is greater than 2 degrees of malalignment if the lesion is greater than 2 cm2 with a cell-based treatment such as microfracture or autologous chondrocyte implantation. The goal of realignment osteotomy with cartilage repair without evidence of joint space narrowing is restoration of normal mechanical alignment and mechanics to the knee joint prior to bringing the mechanical axis to the midline or restoring at least 6 degrees of tibiofemoral valgus.7 When bone-on-bone changes are present on x-ray film and joint preservation with cartilage repair is not indicated, osteotomy remains effective as a pain-relieving procedure that still allows improved levels of activity. However, overcorrection is recommended in this situation, with 2 degrees of overcorrection to the lateral tibial spine being my preferred amount. Anteroposterior instability may be improved upon by altering the tibial slope when performing osteotomy surgery for recurvatum or hyperextension deformity secondary to neuromuscular disorder or anatomic joint line deformity by performing flexion osteotomies. ACL-deficient knees or knees with fixed flexion deformities may be improved upon by extension osteotomies either in isolation or in combination with tibial valgus osteotomies.
Technique selection for high tibial osteotomy
Factors to consider when performing proximal tibial valgus osteotomy include leg length discrepancy, medial joint laxity, ACL laxity, presence or absence of an osteochondral defect on the medial femoral condyle, joint line obliquity, a patient who is a prior smoker or presently is smoking, opiate requirements at baseline, and a cooperative and compliant patient. Recent basic science work evaluating the effect of open versus closing wedge osteotomy on changes in load distribution across the knee have demonstrated that with less than 5-degree osteotomy correction, the closing wedge provided superior results in load transfer from medial to lateral compartments than that seen with an opening osteotomy. However, at 10-degree osteotomy correction, no significant difference in load transfer in the knee compartments was seen between opening versus closing wedge osteotomy.8
Closing wedge osteotomies are presently performed for corrections less than 10 degrees, specifically for conditions of osteochondritis dissecans, large osseous bone cysts, or avascular necrosis of the medial femoral condyle. The autologous bone graft that is harvested with the osteotomy is used as the restorative bone graft for the osteochondral defect on the medial femoral condyle. In this way, malalignment is corrected and the osseous defect is repaired in a single setting (see Chapter 6). Other indications for a closing wedge osteotomy include patients who previously were smokers and laborers who require a quick return to work (i.e., cancellous bone to cancellous bone healing usually occurs within 6–8 weeks).
A reverse dome osteotomy, as popularized by Paley,9 is very powerful for large corrections of 15 to 30 degrees. It has the advantage of maintaining the anatomy of the upper tibia and correcting large deformities. It is technically demanding and requires a freehand technique with a concomitant fibular osteotomy and a fixed-angle device for fixation or an external fixator. It usually is longer to heal (3–4 months).