The Early Diagnosis and Treatment of Hypothyroidism
The Early Diagnosis and Treatment of Hypothyroidism
Hypothyroidism is a medical disorder that affects millions of people. It may be a functional disorder, the result of a weakened immune system, or produced iatrogenically by Western treatment such as a sequel to the treatment of hyperthyroidism. Factors that enter into weakening the immune system include nutritional deficiencies such as lack of iodine in the diet, deficiency of zinc, or deficiency of Vitamins E, A, C, B2, B6, selenium, or copper. Dietary excesses such as consumption of goitrogens (foods that block iodine utilization) such as excess peanuts, cabbage, soy, and mustard may be culprits, as well as lack of balanced, systemic exercise. While Western medicine has two differentiations of hypothyroidism—primary and secondary, the primary hypothyroidism is the most common.
Primary hypothyroidism is thought of as an autoimmune disease induced through chronic inflammation of the thyroid gland, also known as Hashimoto’s thyroiditis. This variety occurs most commonly in women. Secondary hypothyroidism is caused by failure of the hypothalamus to regulate the thyroid gland, or lack of secretion of thyroid-stimulating hormone (TSH) from the pituitary gland. Laboratory evaluation is needed to differentiate these two varieties. Low levels of TSH exist in secondary hypothyroidism, whereas very high levels of TSH characterize primary hypothyroidism due to the fact that there is no feedback inhibition of the pituitary gland.
Signs and symptoms of the early diagnosis of primary hypothyroidism may be non-detectable except through blood analysis. Overt symptoms include fatigue, weight gain, problems of memory and concentration, lowered metabolism, hyperlipidemia, edema, cardiovascular changes, menstrual changes and hypertension.
Standard Western treatment generally involves lifelong hormonal replacement therapy with synthetic hormones or animal protomorphogens. In Oriental medicine, hypothyroidism is classified as a vacuity syndrome of qi, yin or yang, usually of the kidney, and this must be differentiated. Treatment can include long-term acupuncture and herbal medicine, nutritional supplementation, exercise, and avoidance of chemical exposure. Because the illness and not the person is treated in Western medicine the rest of the body may be affected to the point of even inducing hyperthyroidism as the dosage of the medication is experimented with. Oriental medicine treats the whole person such that overall the person remains healthier. In Western medicine the treatment is for life; in Oriental medicine it is based upon the presentation of signs and symptoms.
In my clinical experience I have treated many patients with hypothyroidism but rarely as a major complaint. Such patients came for other health problems and accepted their diagnosis of hypothyroidism and medication as a reality. They did not want it treated directly nor did they have any interest in its possible remediation.
One of my first opportunities to treat hypothyroidism was with a patient with an early diagnosis of primary hypothyroidism within 3 weeks of detection. The reason for this propitious early treatment was related to the vigilance of the patient whom I had been treating for the last 8 years, initially for the effects of stress on her health, and later for health maintenance and other minor problems. She always sought Oriental medical treatment for the resolution of her health problems and this case was no exception.
Following her annual exam with her physician, she came to see me about her new diagnosis of hypothyroidism. At the time of her visit to the doctor she reported to him that she felt she had been suffering from “flu” for about 3 months. The “flu” was characterized by fatigue, sore throat, cough and congestion. Her doctor, on what he called a hunch, ordered blood work that revealed that her thyroid-stimulating hormone level was 9.02, an amount that is almost twice the normal range of 0.40 to 5.50. He diagnosed her condition as primary hypothyroidism and wrote a prescription for Levoxyl and made recommendations for future appointments and periodic testing. However, he was very cooperative and supportive of her medical choices and encouraged her to receive Oriental medical treatment since he knew it to be her preferred approach.
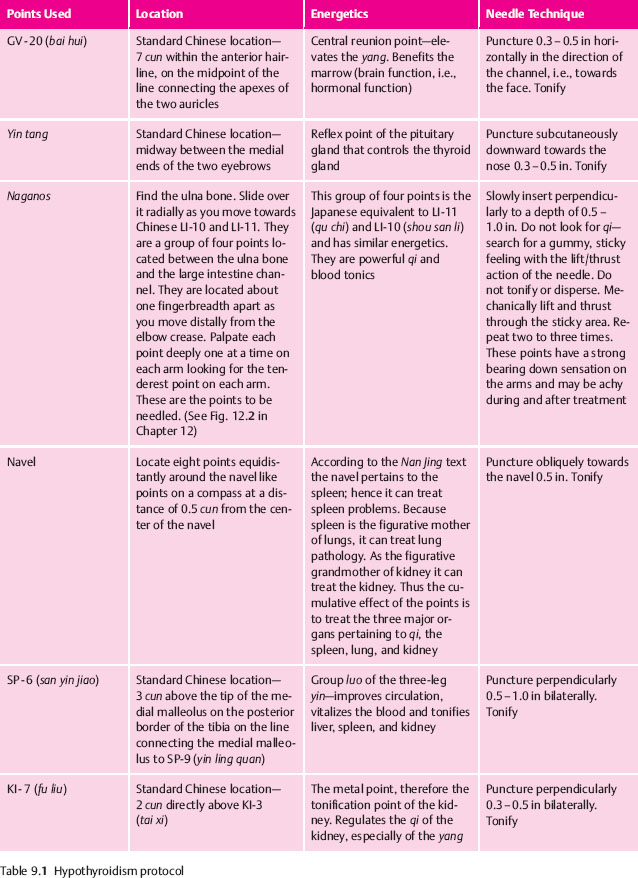
When she came to see me 3 weeks later she did not have any overt, classical signs or symptoms of hypothyroidism. Subjectively she was experiencing tenderness in her neck. I conducted what I call a thyroid evaluation by gently palpating the following points bilaterally for tenderness: local points in the proximity of the thyroid gland, ST-9 (ren ying) and LI-18 (neck fu tu), and KI-3 (tai xi), the source point of the kidney, indicating kidney vacuity. All points were tender. In my experience such tenderness suggests a sub-clinical or clinical hypothyroid condition. I administered a treatment, whose protocol is found in Table 9.1 Its effect is to regulate and tonify the qi and yang, vitalize the blood, and stimulate and strengthen the immune system.
About a week later she returned for a treatment and said that her neck “felt good” and the treatment was repeated. Two weeks later she returned for her third treatment. Overall she felt better and described the previous treatment as a “jump start,” an analogy I think accurately described the treatment plan and its desired effects.
One month after her initial acupuncture treatment her TSH levels were retested. They had almost halved from 9.02 to 4.98 and were now in the normal range of 0.40 to 5.50. Her doctor wrote on the lab results, “Great news?” For further reinforcement she received three acupuncture treatments over the next 3 months and then had a follow-up retest, which revealed that the TSH levels were now a little lower, 4.83. Her doctor pronounced the thyroid as normal and said “Great.” My recommendation was to have her see me three to four times a year for health maintenance and continued monitoring of the thyroid gland.
As of the patient’s 1-year evaluation, she has continued to maintain normal thyroid hormone levels and is in excellent health. I believe that the key to the successful resolution of this disorder is early detection, diagnosis, and treatment of the problem, augmented with high patient compliance, and of course the profound power of the medicine.
For clinician convenience, my treatment protocol follows in Table 9.1. It includes the points used, their locations and point energetics, as well as the specific needle technique employed. Insert needles in the order presented above. Retain the needles approximately 15 minutes. All needles are tonified after the de qi sensation is obtained. Use small amplitude of rotation as a tonification technique with #1 (36 g), 1 in (30 mm) Seirin needles. Remove needles in the same order as they were inserted.
Another patient then sought me out who had a similar diagnosis. She was a 61-year-old female who was diagnosed with hypothyroidism a month before consulting me. Her TSH level had recently risen from 4.5 to 6.37. Apart from high cholesterol, for which she was taking medication that worked, relatively speaking, she was very healthy. Her overall Oriental medical presentation pointed spleen and kidney qi and yang vacuity with concomitant liver qi stagnation due to blood vacuity as evidenced through long-standing cold hands and feet, sensitivity to external cold, gas, overthinking, minor seasonal allergies and a feeling of incompleteness with the bowel movement. Her tongue was slightly pale with paler sides and cracks. Her pulse was superficial, wiry, and weak in the lung and heart positions.
A physical examination by way of palpation revealed bilateral tenderness at ST-9 (ren ying), diagnostic of thyroid conditions, and Japanese “KI-3” (tai xi), referred to in Japanese acupuncture as the thyroid confirmation and treatment point. As the yuan source point KI-3 balances the kidney yin and yang, comprising the kidney qi, which was vacant. Her abdomen in the dan tian area was puffy and vacant indicating kidney yang vacuity. Palpation for a deep pulse at CV-6 (qi hai), where the qi of the two kidneys communicates with each other, was imperceptible, further supporting the vacuity of kidney yang. This could be construed, amongst other things in Western parlance, as hypothyroidism. (If interested in these concepts, see my book The Art of Palpatory Diagnosis1 for more information on abdominal diagnosis and Japanese point location, energetics, and treatment.)
The first treatment was administered consisting of needling yin tang, the pituitary gland reflex point, to adjust the secretion of thyroid-stimulating hormone, ST-25 (tian tu) bilaterally to balance the qi and the blood, and KI-3 (tai xi) to tonify the kidney qi. All insertions were performed with a #1 gauge, 1 in Seirin needle. Yin tang was inserted 0.5 cun transversely downward, tian tu perpendicularly 0.8 in, and Japanese “KI-3” (which is identical to Chinese KI-5) transversely and posteriorly toward the heel 0.3 in. With the exception of KI-3, which was simply tonified by inserting the needle towards the heel, in the direction of the channel, which is a tonification technique, the other points were tonified with a slight clockwise turn of the needle, and needles were retained for about 15 minutes.
After a month, the patient reported a feeling of well-being and decreased gas. Her blood work revealed a decrease in her TSH levels from 6.37 to 5.1, now within the normal range. Her doctor recommended a 6-month blood work follow up and I concurred. I likewise advised the patient to receive a minimum of one acupuncture treatment per month to maintain and/or further decrease the TSH level. During those times, further herbal evaluation and prescribing could be made based upon presenting signs and symptoms. Yearly Western thyroid evaluation was recommended to monitor TSH levels change in the blood so they can quickly be corrected.
Since then I have treated more hypothyroid patients similarly and with good result. For those I have treated with a longstanding diagnosis of hypothyroidism for 10 – 20 years, TSH levels have been reduced by about 67 % but at that point have been resistant to further lowering with Oriental medicine.
In summary, I am encouraged by the responsiveness of this disorder to Oriental medical intervention. As in the first case, I surmise that its efficacy s primarily related to early detection and appropriate differentiation and treatment and urge patients who receive such a diagnosis to seek qualified Oriental medical care and comply with practitioner recommendations to prevent a lifelong dependence on Synthroid or other thyroid medications and the possible devastating sequelae of hypothyroidism.
 Hyperthyroidism
Hyperthyroidism
In contrast to hypothyroidism, which is relatively easier to treat with Oriental medical modalities, hyperthyroidism is almost as equally difficult to address. The difference of course stems from their etiology and the corresponding difference in correcting those causative factors.
As we recall from our understanding of zang fu pathology outlined above, hypothyroidism is caused by spleen or kidney qi and/or yang vacuity, liver qi stagnation and blood vacuity with its corresponding symptoms of lethargy, intolerance to cold, modest weight gain, forgetfulness and coarse dry skin. As we have seen, many times its symptoms are sub-clinical. The appropriate treatment plan is to tonify the qi and yang of the kidney, move the liver qi stagnation and tonify the blood.
Hyperthyroidism, with its symptoms of nervousness, increased sweating, hypersensitivity to heat, palpitations, fatigue, tachycardia, fidgeting, weight loss, insomnia, increased appetite and various eye symptoms such as photophobia, irritation and dryness is caused by a vacuity of the yin of the kidney and the liver and hyperactivity of liver yang. There may be heart yin vacuity symptoms as well. Energetically, on a continuum of qi, blood, yin and yang, yin is the deepest structural level and qi the most superficial, and hence we can see the reasons why hypothyroidism is more responsive to treatment than hyperthyroidism
The doctors I studied with in China advocate the use of Western medications to treat hyperthyroidism although they do use some acupuncture as well. In my experience, because of the physical and psychological differences in both types of patients, i. e., the quiet and sedate hypothyroid patient versus agitated and restless hyperthyroid patient, the hyperthyroid patients are more resistant to therapy. In terms of acupuncture treatment, the hypothyroid patients who are vacuous in qi and yang can be well treated with needles and adjunct techniques such as moxibustion, the TDP lamp and herbs. Their symptoms of vacuity respond to energetic treatment better than symptoms of heat and fire, characteristic of hyperthyroidism.
For the hyperthyroid patient, reclining on the table in and of itself may be difficult because of the aforementioned symptoms. Because their deep-seated vacuity, their energy rises to the surface, so superficial needling should be avoided as well as long needle retention times. They are vacuous in a way more so than hypothyroid patients, because the yin is a deeper structural level. As such, hyperthyroidism takes longer to treat over time.
Below, two treatment plans are presented for the treatment of hyperthyroidism, which are similar in construction to each other, and can be used independently depending upon which modality you as a practitioner prefer or which therapy the patient would best tolerate.
Auricular Acupuncture
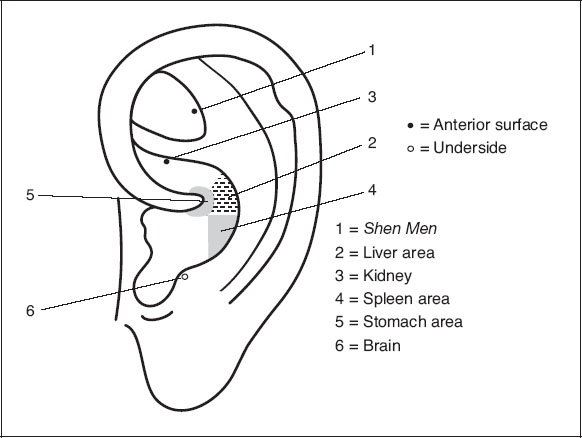
- Shen men. This point, analogous to HT-7 (shen men) in the body, quiets the heart, grounds the patient, makes the heart serene, and puts the patient into a state of receptivity for treatment. It is useful for the heart yin vacuity symptoms of insomnia, restlessness, and agitation, tachycardia and palpitations. To accomplish this aim, treat this point first.
- Kidney. Use to tonify kidney yin and liver yin because the kidney is the mother of liver. It will reduce fatigue and decrease fire by strengthening yin.
- Liver. Use to directly nourish the liver yin, and to reduce the liver yang and fire, and move liver qi stagnation. The liver point treats eye symptoms, decreases nervousness, fidgeting and heat hypersensitivity.
- Brain. Use to influence all neurological functions, to regulate the mind, and improve eye problems.
- –6. Spleen and stomach. Choose these points to tonify the qi, which produces the yin and the blood. The kidney yin will thereby be nourished through the five-element control cycle. Because these points relate to the earth element, they also ground and anchor the energy and this assists in treating insomnia, mental symptoms and appetite
Method
After cleaning the ear with an alcohol swab, allow the ear to dry naturally. Then insert a 0.5 in #28 gauge needle perpendicularly into each point with the exception of the brain point, which is needled obliquely and anteriorly due to its location on the posterior border of the antitragus. Obtain qi, ideally in the form of heat, and tonify with a slight clockwise turn. Retain the needles 10 to 15 minutes. After removal of the needles, to reinforce the treatment, affix gold Magrain pellets to the same points but in the opposite ear, which has also been cleaned. Instruct the patient to press gently on the pellets three to five seconds, three to five times a day, for three to five days. Show the patient how to remove the pellets within the allotted timeframe or earlier if the ear becomes irritated, or to return to the office for you to remove them. See Figure. 9.1 for the location of these points
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree