Throwing Shoulder
Brian C. Werner
Stephen F. Brockmeier
DEFINITION
The repetitive acceleration and deceleration of the arm during the throwing motion places the thrower’s shoulder in extreme positions and under significant stresses, which can lead to chronic overuse-type injuries as well as acute injuries to the throwing shoulder.
The overhead athlete develops well-described adaptations in response to the stresses of throwing, including range-of-motion changes (glenohumeral internal rotation deficit [GIRD]), soft tissue changes, and bony adaptations.
Soft tissue adaptations that occur in overhead athletes result from the large rotational and distractive forces the glenohumeral joint experiences during throwing; over time, this leads to anterior capsular laxity and maladaptive contracture of the posteroinferior glenohumeral joint capsule.6
Posteroinferior capsular contracture alters the biomechanics of the glenohumeral joint during the throwing motion and produces a predictable constellation of injuries in disabled throwers, termed internal impingement, including superior labral and biceps anchor pathology, undersurface partial-thickness rotator cuff tears that can progress to full-thickness rotator cuff tears, and disruption of the anteroinferior capsule or labrum.2
Symptoms resulting from these injuries can lead to “dead arm syndrome,” where the throwing athlete cannot compete at a premorbid level due to shoulder discomfort with throwing and resultant loss of pitch velocity and control.5
Muscle strength imbalances and scapular dyskinesia can contribute to the development of shoulder pain in the throwing athlete and should not be ignored as a potential etiology for symptoms.
ANATOMY
It is important to consider both native shoulder anatomy as well as adaptive bony and soft tissue anatomic changes in the thrower’s shoulder.
The scapula plays a critical role in energy transfer from the trunk to the humerus. Eighteen muscles attach to the scapula and control its position on the chest wall.
Changes in scapular position can lead to external impingement due to anterior tilt, internal impingement, decreased rotator cuff strength, and anterior capsular strain. Altered static and dynamic scapular mechanics arise from overuse and weakness of scapular stabilizers and posterior rotator cuff muscles.
A pitcher’s shoulder experiences forces equal to nearly half their body weight during the late cocking phase and distraction forces of nearly the entire body weight during the deceleration phase. Professional pitchers can generate up to 92 Nm of humeral rotation torque, which is above the torsional failure limit found in cadavers. The scapular stabilizers and posterior rotator cuff muscles contract violently at ball release and protect the glenohumeral joint from the deceleration force of the arm.
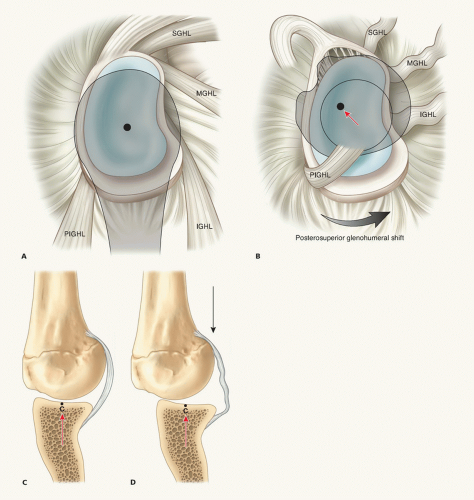
The relative position of the glenohumeral ligaments changes with different arm positions. As the arm is brought into full abduction and external rotation (late cocking phase), the posterior band of the inferior glenohumeral ligament (PIGHL) complex moves from a posteroinferior position to a position directly inferior (6 o’clock) in relation to the glenoid.4
As many as five anatomic structures are at risk in the pathologic thrower’s shoulder: the posterior superior labrum, the rotator cuff tendon (specifically the articular side of the posterior supraspinatus and anterior infraspinatus), the greater tuberosity, the inferior glenohumeral ligament (IGHL) complex, and the posterior superior glenoid.
PATHOGENESIS
Internal Impingement
Internal impingement of the shoulder is characterized by excessive or repetitive contact of the greater tuberosity of the humeral head with the posterosuperior aspect of the glenoid when the arm is abducted and externally rotated; this leads to impingement of the rotator cuff and labrum.
Controversy exists regarding whether internal impingement is a normal or pathologic condition; however, it has most often been described as a chronic, pathologic condition that is associated with throwing and other repetitive, overhead athletic activities.
The inciting lesion causing disability in throwers is posterior shoulder muscle weakness due to chronic, repetitive loading.
Posterior muscle weakness leads to shoulder dysfunction as a result of both scapular dyskinesis (described in the following texts) and posterior capsular (PIGHL) contracture. One of these pathologic entities may predominate in the disabled thrower, but they are generally intimately related.6
PIGHL contracture develops primarily due to failure of the weakened posterior shoulder muscles to counteract the distraction force of the arm after ball release. This exposes the posterior capsule to abnormal stress due to the forward-flexed and adducted position of the arm at follow-through. Fibroblastic thickening and contracture of the PIGHL occurs as a maladaptive response to these substantial stresses.
PIGHL contracture can be identified clinically as a scapular-stabilized GIRD in the throwing shoulder.4
The thickened PIGHL alters the normal biomechanics of the glenohumeral joint, particularly as the arm is brought into abduction and external rotation (late cocking phase). The center of glenohumeral rotation is shifted posterosuperiorly due to the contracted PIGHL occupying a position directly inferior to the humeral head in this arm position (FIG 1A,B).7
Alteration of the glenohumeral contact point leads to a predictable pathologic cascade with continued throwing.4
Posterosuperior shift allows greater clearance of the tuberosity over the posterosuperior glenoid rim, enabling pathologic hyperexternal rotation of the arm in the late cocking phase, which leads to the following:
An abnormal posteriorly directed shear stress and torsion on both the rotator cuff and biceps insertion point of the labrum. The biceps anchor ultimately fails and “peels back” medially along the posterosuperior glenoid neck (superior labral anterior posterior [SLAP] tear). SLAP tears are typically anterior and posterior or posterior subtypes of type II tears (the “thrower’s SLAP”).10
Rotator cuff tears occur because of repeated abrasion and torsion of tendon fibers. Torsion failure is most pronounced on the articular side of the tendons, resulting in the partial undersurface tears most commonly seen in throwers, which may progress to full thickness with continued throwing.
Posterosuperior shift of the glenohumeral contact point causes relative relaxation and “pseudolaxity” in the anterior capsule (FIG 1C,D). This is termed microinstability or the acquired anterior capsular laxity that allows increased humeral head translation with arm motion. Although some capsular laxity and increased translation represent functional adaptations, beyond a certain threshold, the increased laxity becomes pathologic.
With continued hyperexternal rotation, tension may ultimately cause anteroinferior capsular fiber attenuation, leading to tertiary anterior glenohumeral instability. Discrete “Bankart-type” lesions of the labrum can occasionally occur in this group. Anterior instability is a later event in the pathologic cascade, not the primary lesion as previously described.8
Muscle Imbalances
Both symptomatic and asymptomatic throwers have been shown to have imbalances in shoulder muscle strength. The throwing athlete requires a balanced ratio of concentric agonist and eccentric antagonist muscle strength for stability and function.
In throwers with internal impingement, imbalances in rotator cuff musculature, including relative weakness of the internal rotators, result in abnormal internal/external rotational strength ratios.
These imbalances alter the anterior/posterior force couples that stabilize the glenohumeral joint and increase compressive forces in the joint.
This also decreases the ability of the shoulder to decelerate during the later phases of throwing.
Scapular Dyskinesis
In scapular dyskinesis, the position of the scapula on the chest wall is altered owing to loss of scapular elevation and retraction control. The scapula drops (infera), moves lateral from the midline (protraction), and abducts from the midline. The inferior scapular angle may also lift off the chest wall and pitch toward the front of the body (antetilt).
These changes in scapular position lead to external impingement due to anterior tilt, internal impingement, decreased rotator cuff strength, and anterior capsular strain.9
Altered scapular position causes abnormal tension on the insertion of scapular stabilizer muscles and over time leads to inflammation and pain.6
The abnormally positioned thrower’s scapula has been labeled SICK for Scapular malposition, Inferior medial border prominence, Coracoid pain, and dysKinesis of scapular movement by Burkhart.6
NATURAL HISTORY
Throwing athletes manifesting clinical findings of posterior muscle weakness and scapular asymmetry, including decreased pitch velocity, heaviness, or fatigue, without signs of labral or rotator cuff pathology may attempt to correct their shoulder dysfunction with a progressive scapular strengthening program and return to normal function through a pitching program when the asymmetry resolves.
Throwers who have vague shoulder discomfort and demonstrate an internal rotation deficit (GIRD) are started on focused internal rotation stretches (“sleeper” stretches) to alleviate PIGHL contracture and restore normal glenohumeral biomechanics and range of motion. GIRD reduction to less than 20 degrees removes the athlete from being at risk for shoulder injury and generally allows return to premorbid function.
Pain with throwing is indicative of an injury to glenohumeral structures.
Once actual injury to glenohumeral structures, particularly the labrum, has occurred, mechanical symptoms ensue and the thrower will more frequently not be able to return to prior function without surgical intervention.
PATIENT HISTORY AND PHYSICAL FINDINGS
Presenting symptoms typically include subjective feelings of heaviness and sluggishness, stiffness, fatigue, and weakness.
Objective indications of dysfunction include decreased throwing velocity, lack of movement on pitches, and decreased accuracy and control.
Acute injuries do occur in overhead throwing athletes; however, it is much more common for injuries to be secondary to overuse and fatigue.
The timing of onset of symptoms, previous and current treatments, and history of previous shoulder injuries should be determined.
In addition to standard history questions, the throwing athlete should be asked questions specifically related to their pitching including changes in mechanics, addition of new pitches, increased pitch count, changes in training, and if injury to other areas of the body (ie, hip, core, lumbar spine) has occurred, which could lead to compensatory alterations in throwing mechanics.
Physical examination should not just focus on the shoulder or upper extremity but also on the rest of the kinetic chain including the lower extremities and trunk.
Pain is most prominent during the late cocking phase of throwing when the peel-back phenomenon of the superior labrum occurs caused by the posterosuperior glenohumeral shift.5
Pain is localized to the antero- or posterosuperior shoulder and is described as “deep.”
Mechanical symptoms, such as painful popping, clicking, or snapping, may occur after injury to the superior labrum, particularly during late cocking and early acceleration.
The surgeon should check for tenderness in the coracoid, the acromioclavicular joint, and the superomedial scapular angle.
Both shoulder girdles must be completely exposed or subtle asymmetry will be overlooked.
Inspection is done with the patient standing in front of fixed vertical and horizontal references (such as window blinds or door frames) so that affected and unaffected shoulders can be compared for scapular height and malposition (FIG 2).
Superior and inferior angles as well as the medial scapular border are marked as a visual reference. Spinous processes are marked for a midline reference.
Asymmetry from the unaffected side when in protraction or infera indicates scapular stabilizer muscle weakness.
When in abduction or antetilt, increasing magnitude compared to opposite side signifies scapular muscle weakness.
Both active range of motion (AROM) and passive range of motion (PROM) should be assessed with special attention paid to glenohumeral and scapulothoracic motion. The patient should be examined in both the standing and supine positions.
Glenohumeral PROM is assessed for external rotation (ER) and internal rotation (IR) at 90 degrees of abduction and for ER at 45 degrees of abduction in the scapular plane.
Increased external rotation with the arm at the side with patient supine can be indicative of rotator interval laxity.
Increased external rotation in abduction and external rotation reflects anteroinferior capsular laxity or humeral retroversion.
A careful assessment for GIRD must be made. The posteroinferior capsule is evaluated by stabilizing the scapula and passively rotating the arm when it is abducted at 90 degrees. Internal rotational deficits of 15 to 20 degrees can be seen in the throwing arm due to both bony and soft tissue adaptations of the throwing shoulder; however, the overall arc of motion should be similar between the throwing (ts) and nonthrowing shoulders (nts).
ER + IR = total mobility arc (TMA)
IRnts − IRts = GIRD
TMAts = TMAnts in healthy throwers
GIRDts greater than 20 degrees seen in “shoulders at risk” for injury; generally GIRDts loss of TMAts versus TMAnts
Muscle strength should be evaluated after range of motion is determined. The rotator cuff musculature, including subscapularis, should be isolated and assessed.
Subacromial impingement is assessed using the Hawkins-Kennedy and Neer tests.
Several tests are available to examine the labrum of the throwing athlete. The examiner should use the tests they are comfortable using and develop a consistent pattern of examination. The following tests for type II SLAP lesions in throwers are commonly used:10
The modified Jobe relocation test is specific for a posterior subtype. In throwers with SLAP tears, their usual pain is reproduced and they will localize to the posterosuperior joint line (“deep”). Pain in the abduction and external rotation (ABER) position is due to an unstable labrum; anterior pressure reduces the labrum and relieves pain.2
The O’Brien active compression test is specific for an anterior subtype. A positive result is defined as pain with resisted forward flexion and pronation; pain is diminished or relieved with supination.
The Speed test is specific for an anterior subtype. A positive result is defined as pain with resisted forward flexion.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs: anteroposterior (AP), scapular lateral (Y), and axillary views to detect bone or joint space abnormalities
Possible radiographic findings in association with internal impingement include exostosis of the posteroinferior glenoid rim, sclerotic changes of the greater tuberosity, posterior humeral head osteochondral lesions, or rounding of the posterior glenoid rim.
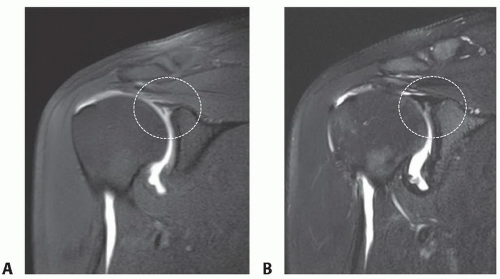
Magnetic resonance imaging (MRI): MRI remains the gold standard imaging modality for young patients with shoulder pain, particularly overhead athletes. The decision whether to include intra-articular contrast is widely debated and depends greatly on the preferences of the radiologists reading the studies. We routinely order intra-articular contrast material because it improves the ability to detect labral and capsular abnormalities as well as partial-thickness rotator cuff tears (FIG 3A,B).
Typical MRI findings of internal impingement include articular-sided partial-thickness rotator cuff tears and posterior or superior labral lesions.
Specialized MRI imaging sequences taken with the affected arm positioned in ABER view can be helpful in this patient population to demonstrate subtle superior labral pathology and partial-thickness rotator cuff tears with delamination.
DIFFERENTIAL DIAGNOSIS
Subacromial bursitis secondary to rotator cuff weakness and dysfunction
Various forms of anterior shoulder pain, acromioclavicular joint dysfunction, and posterior periscapular pain secondary to scapular dyskinesis and the SICK scapula syndrome.6
Pain with throwing may occur with rare conditions such as bone tumors, stress fractures, and growth plate abnormalities in adolescent athletes.
NONOPERATIVE MANAGEMENT
With a few notable exceptions, conservative options should be exhausted in throwing athletes prior to consideration for surgical intervention.
Rest, cryotherapy, oral anti-inflammatory medications, and a supervised phased physical therapy program are the cornerstones of nonoperative treatment.
Symptomatic athletes are begun on a scapular reconditioning program combined with internal rotation posteroinferior capsular sleeper stretches.
Scapular reconditioning focuses on regaining scapular elevation and retraction control; progress is assessed by repeat examination for normalization of scapular symmetry.
Initially, bilateral shoulder shrugs and rolls are combined with retraction “no money” exercises.
The patient progresses to closed-chain “table top” movements and wall-washing motions.
Finally, prone “Blackburn”-type exercises are instituted.
Strengthening of the periscapular musculature and rotator cuff can minimize hyperextension and external rotation of the glenohumeral joint.
Sleeper stretches focus on the posteroinferior capsular contracture that initiates the internal derangement in the glenohumeral joint (FIG 4). Response to a course of internal rotation stretching will determine the extent of the PIGHL contracture.
90% of athletes will decrease their GIRD to an acceptable magnitude with 10 to 14 days of focused stretching (<20 degrees) with near-normalization of TMAts and TMAnts.
The remaining 10% have recalcitrant PIGHL contracture and will show little or no decrease in GIRD after a period of stretching; they are termed stretch nonresponders. These are generally veteran athletes with long-standing GIRD and may require posteroinferior capsulotomy to regain internal rotation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree