Throwing Injuries
Walter A. Thomas MD
Heinz R. Hoenecke MD
Jan FronekD MD
Specific questions of an overhead athlete should include the type of throwing, level of competition, and any history of previous trauma, such as shoulder dislocation.
Juvenile throwers are more likely to present with a physeal injury and symptoms related to laxity and associated labral tears, while older throwers tend to injure the rotator cuff.
Sports-specific questions are helpful; for example, where in the pitching cycle symptoms are experienced; changes in throwing accuracy, velocity, or stamina; as well as changes in training regimens.
Physical examination should include focus on general posture, position of the head and neck, and trunk, as well as on the affected arm.
Various provocative tests are useful to help identify the source of pain in a throwing athlete. Overlap exists with the tests designed to identify biceps pathology because these may be positive in an athlete with labral pathology.
Radiographs should include a throwers’ series—an anteroposterior (AP) view in internal and external rotation, a scapular outlet view for assessment of acromion morphology, and an axillary lateral to identify bony Bankart lesions.
Electrodiagnostic imaging may be warranted in cases where weakness is believed to be neurologic in nature. The electromyogram (EMG) can help differentiate mononeuropathies for more diffuse, widespread processes such as radiculopathy or brachial plexopathy. The most common mononeuropathies in the throwing athlete are suprascapular and long thoracic neuopathies.
Partial-thickness articular-sided tears of the supraspinatus and infraspinatus are well recognized in the throwing athlete. The etiology of these tears is multifactorial, but a significant component is believed to be tensile force overload during the deceleration phase in addition to the mechanical abrasion of internal impingement.
How and when the injury occurred and what took place right before the injury is important in establishing a diagnosis when dealing with the elbow. Changes in throwing accuracy, velocity, stamina, and strength are important, as well as changes in training regimens.
Ulnar nerve compressions may occur at various sites. Throwing athletes experience ulnar nerve irritation from traction injuries, compression from adjacent structures, or friction due to subluxation of the ulnar nerve. Complaints are typically paresthesia of the small and ring finger during or after the throwing motion.
The throwing athlete places far greater stress on his or her shoulder and elbow than the average population and consequently injuries commonly occur. The pathoanatomy and biomechanics of the throwing motion is complex and our understanding of injury mechanism and etiology continues to evolve. Specific injuries can occur in isolation and also as part of a spectrum of interrelated pathology, making a comprehensive understanding of pathoanatomy critical for rapid diagnosis and effective treatment.
The throwing motion has been divided into six phases (Fig 21-1):
Phase I: The wind up
Phase II: Early cocking
Phase III: Late cocking
Phase IV: Acceleration
Phase V: Deceleration
Phase VI: Follow through
Phase I is the initial wind up. This represents the coiling phase in which potential energy is developed. During this phase, the center of gravity is raised and no appreciable stress is placed on the shoulder and elbow.
Phase II is early cocking. During this phase, the arm is positioned in preparation for maximal external rotation which occurs with stride initiation as the arm is positioned in 90 degrees of abduction. Early deltoid and late rotator cuff activity is show by electromyogram (EMG).
Phase III is late cocking. This phase initiates with the foot plant. It is also the point of maximal external rotation of the shoulder, approaching 170 degrees. The shoulder is positioned in abduction and external rotation, and the humeral head translates posteriorly on the glenoid. High rotator cuff activity is seen in supraspinatus, infraspinatus, and teres minor during the middle of this phase, while the subscapularis fires later coinciding with the opening of the torso. Maximal stress to the anterior restraints of the shoulder occurs and the shear forces approach 400 N, with the compensatory rotator cuff forces reaching 650 N.
Phase IV is the acceleration phase. The shoulder delivers the ball to the release point during this phase. Peak rotational velocity can approach 7,000 per second. The shoulder rapidly internally rotates and returns the humeral head to a neutral position; this occurs with minimal load to the glenohumeral joint during energy transfer.
Phase V is the deceleration phase. This is the most forceful phase of the throwing cycle. Deceleration occurs from the point of ball release. It occurs with substantial eccentric contraction of the rotator cuff to slow the arm. Posterior capsule stress is at a maximum. Joint loads are as follows: posterior shear 400 N, inferior shear 300 N, and compressive force approaching 1,000 N.
 Fig 21-1. Phases of the throwing motion: I. Wind up; II. Early Cocking; III. Late Cocking; IV. Acceleration; V. Deceleration; VI. Follow through. |
Phase VI is the follow through. This phase is a time of muscle rebalancing with stress still present in the posterior capsule. The entire throwing cycle spans approximately 2 seconds.
History
An evaluation of the overhead athlete begins with a thorough history. The specific questions should address the patient’s history regarding handedness, type of throwing, level of competition, and any history of previous trauma (such as previous shoulder dislocation). The age of the athlete is particularly important, because the juvenile athletes may present with a physeal injury; the younger throwers are more likely to have symptoms related to laxity and associated labral tears while the older throwers tend to injure their rotator cuff.
The history should include questions concerning the mechanism of onset, the duration of symptoms, aggravating and alleviating factors, and any previous treatments and their effectiveness. Is pain the major concern? Does the patient experience weakness or fatigue? Does the patient have a feeling of generalized looseness or tightness in his or her shoulder? Are there any episodes of catching or popping that may be indicative of labral pathology or instability? Understanding the patient’s specific concern is important, as is understanding his or her short- and long-term goals. Are these goals realistic, given the patient’s age, previous level of performance, severity of injury, and other medical factors?
Sport-specific questions will often be helpful. Where in the pitching cycle do they experience symptoms? Pain occurring during the cocking phase may be related to internal impingement, labral pathology, or instability (usually anterior or antero-inferior). Pain occurring during deceleration may be suggestive of cuff pathology, or posterior subluxation. Do the symptoms occur early in the game or during the later innings? What is the specific location of the symptoms? Does the patient experience a dead arm, can he or she continue throwing, and is there associated paresthesia? Does the thrower experience signs or symptoms of fatigue?
Physical Examination
The physical examination begins with inspection; focus should be not only on the affected arm, but also on the athlete’s general posture and the position of the head, neck, and trunk. Muscle contour and balance should be observed with attention given to subtle signs of asymmetry or atrophy, which may help focus the examination. When viewing the back of the patient, the examiner can appreciate a scapular asymmetric depression, protraction, or winging of the scapula, which may be present as an isolated finding or in combination with an intra-articular problem.
Range of motion should be observed, both glenohumeral and scapulothoracic contributions. Scapulothoracic motion should be smooth and pain free; comparison with the contralateral shoulder should be noted for symmetry of position and motion; crepitus may be suggestive of inflammatory bursitis. Total rotation of the throwing shoulder should be recorded and compared with the nonthrowing shoulder. It is common for throwing athletes to have increased external rotation in abduction and decreased internal rotation in abduction in their throwing shoulder; however, the arc of total motion should be similar.
Palpation for pain is helpful to identify specific areas of injury and can distinguish between various types of pathology that can often present with similar symptoms. Specific focus should be on the muscles of the rotator cuff, long head of the biceps, conjoined tendon, anterior and posterior capsule, acromioclavicular (AC) joint, and suprascapular notch.
Strength testing of the rotator cuff muscles and the periscapular stabilizing muscles should be performed. The supraspinatus is tested with resisted forward elevation with the arms in 30 degrees of abduction with the thumbs pointed to the floor. The infraspinatus and teres minor are tested with resisted external rotation with the arms adducted at the side. The subscapularis is tested with the lift-off test or the belly press test. When weakness or muscle pain is present, the testing should be repeated with the scapula actively retracted and depressed. If strength improves or pain decreases, this represents a positive scapular retraction test consistent with scapular dyskenesis.
Laxity and translation of the glenohumeral joint should be assessed in the anterior, posterior, and inferior directions. This should be performed with the arm in both internal and external rotation and with the athlete sitting and also lying supine. Increased laxity is an expected finding in the dominant arm and is not necessarily pathologic, but laxity associated with discomfort or with reproducing the thrower’s symptoms is likely to be pathologic instability.
Various provocative tests are useful to help identify the source of pain in a throwing athlete. Hawkins and Neers tests may be useful for identifying impingement. The apprehension and relocation test may be useful when they elicit discomfort or apprehension, but are less helpful when they are associated with pain. Various tests have been described for assessing labral pathology; recent reports reveal limited sensitivity and specificity with the active compression test, the anterior slide test, and the compression rotation test (1,2,3). Overlap exists with tests designed to identify biceps pathology because these may be positive in an athlete with labral pathology.
Ancillary Tests
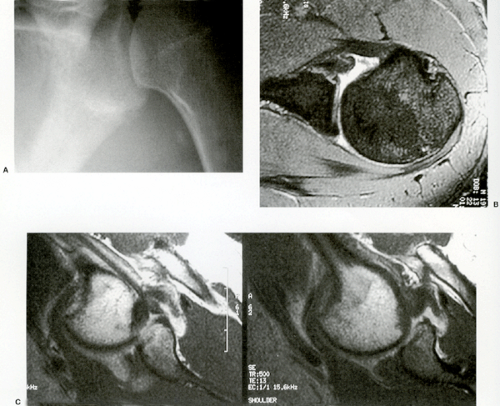
Radiographs are useful in evaluating bony anatomy and include a throwers’ series, an anteroposterior (AP) view in internal and external rotation (internal rotation view is helpful to assess Hill-Sachs lesions), a scapular outlet view for assessment of acromion morphology, and an axillary lateral to identify bony Bankart lesions (Fig 21-2A). Additional views and MRIs may be ordered when physical examination indicates that they would be useful (Figs 21-2B and C, and Figs 21-3,21-4,21-5).
Computed tomography (CT) scanning has limited applications, but may be useful in evaluation of glenoid bone loss. Ultrasound can be helpful for rotator cuff tendinopathy, but is of limited application because it is very operator dependent and few institutions have the experience necessary for consistent interpretation.
Magnetic resonance imaging (MRI) may be helpful in certain situations for establishing a specific diagnosis. Magnetic resonance arthrography (MRA) can also be a useful adjuvant diagnostic tool; dilute gadolinium is injected into the shoulder and gives more anatomic detail in athletes with suspected labral lesions or potentially other instability-related pathology [humeral avulsion of the glenohumeral ligament (HAGL lesion), anterior labor-ligamentous periosteal sleeve avulsion (ALPSA lesion), and glenoid labral articular disruption (GLAD lesion)].
Electrodiagnostic testing may be warranted in cases when weakness is believed to be neurologic in nature. The EMG can help differentiate mononeuropathies for more diffuse, widespread processes such as radiculopathy or brachial plexopathy. The most common mononeuropathies seen in the throwing athlete are suprascapular and long thoracic neuropathies.
The Shoulder
The Thrower’s “Dead Arm”
In the overhead athletes, the “dead arm” syndrome has long been recognized as a potentially career-ending condition. Historically, the specific pathology has been poorly understood; only recently has greater insight been achieved into etiology; however, treatment remains controversial.
Athletes often complain of pain during the late cocking and acceleration phase, as the arm moves forward. The arm then “goes dead” and the athlete has loss of velocity and control; this, along with pain, prevents continued throwing and results in compromised performance. Various conditions have been observed, and debate concerning which model of pathology is most accurate is further complicated by the fact that
these conditions may be present in asymptomatic throwing athletes, thus suggesting a spectrum of variation, often with no clear distinction from the adaptive to the pathologic changes.
these conditions may be present in asymptomatic throwing athletes, thus suggesting a spectrum of variation, often with no clear distinction from the adaptive to the pathologic changes.
Internal Impingement
Internal impingement is a topic that has been controversial and also can be very confusing. Originally described by Walch et al. (4) as naturally occurring impingement between the posterior superior rotator cuff and the glenoid rim with arm in position of abduction and external rotation. Others noted this same occurrence in asymptomatic throwing athletes.
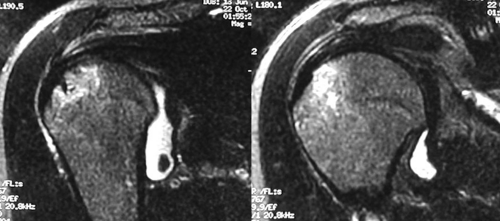
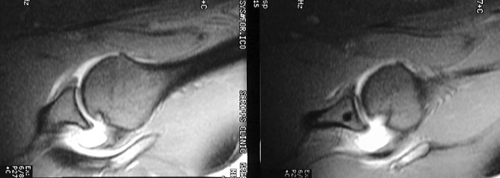 Fig 21-5. MRI study, two adjacent images demonstrate the Hill-Sachs defect seen in abduction and external rotation. |
Jobe (5) later popularized the term as a pathologic condition occurring in overhead athletes leading to throwing injury. In this model, anterior capsular insufficiency was the inciting occurrence that subsequently led to further disability and the “dead arm.” Loss of integrity of the capsule is a direct result of hyperangulation of the throwing arm. The symptoms are exacerbated by the loss of the posterior rollback, which leads to anterior translation and results in greater internal impingement posteriorly. If untreated, it may lead to posterior labral tears, Superior Labrum Anterior and Posterior (SLAP) lesion due to peel-back, and partial thickness articular-sided rotator cuff tears. Treatment is focused at correcting the underlying instability and treating any additional pathology. Reports of capsulolabral reconstruction have shown some success in allowing pitchers to return to their previous level of competition (6,7).
The Morgan-Burkhart model (7a, 7b) suggests that the posterior capsular contracture is the inciting occurrence in the cascade of disability and injury. Posterior capsule tightness has long been recognized as a component of the throwing shoulder (8,9,10,11,12); at what point this becomes pathologic has been less well delineated. As the shoulder develops progressively worsening posterior contracture, the glenohumeral contact point is shifted further posterior and superior when the shoulder is in abduction and external rotation. A relative redundancy of the anterior capsule is observed due to the tightening of the posterior capsular structures—this is what has been observed as anterior capsular stretching in the Jobe model. As the thrower attempts to reach his or her set point for throwing, hyperangulation and hyperexternal rotation forces cause tensile overload of the rotator cuff leading to partial tears; additionally, a dynamic peel-back phenomenon generates SLAP lesion of the labrum. Glenohumeral Internal Rotation Deficit (GIRD) is defined as the loss in degrees of internal rotation as compared with the contralateral shoulder, with the arm positioned in 90 degrees of abduction and external rotation. Burkhart et al. (13) believe that symptomatic GIRD is present when the deficit is 25 degrees or greater. Treatment focuses on stretching the posterior capsule with the use of “sleeper stretches.” Although the nonsurgical treatment is usually successful, those who do not respond to relative rest, stretching, and strengthening programs may be candidates for arthroscopy, debridement, and occasional posterior capsulotomy, which is often performed with treatment of other coexistent pathology.
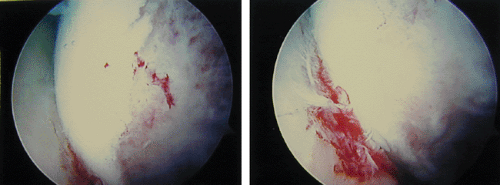
Labral pathology is well recognized as a component of the disabled throwing shoulder. The acromym SLAP describes the location of pathology, Superior Labrum Anterior and Posterior. It was first observed by Andrews (13a) in throwing athletes and was later named by Snyder. Multiple subtypes have been described. Some believe that SLAP lesion is the most common pathologic entity associated with the throwers “dead arm” (9,13,14). If left untreated, athletes typically cannot return to throwing. Debate has existed concerning the mechanism of injury during throwing. Fleisig et al. (15) and Andrews et al. (16) proposed a deceleration mechanism of injury, as the bicep contracts to slow down the arm in follow through. This tensile load acts to pull the biceps and superior
labral complex from the bone. Burkhart et al. (13) support an acceleration mechanism of injury. As the shoulder is positioned in abduction and external rotation coinciding with late cocking and acceleration, the labrum is peeled off the glenoid rim. Kuhn et al. (17) performed experimental comparison of the two mechanisms in a cadaveric model; their results support the acceleration mechanism. Treatment is dictated by the stability of the biceps/labral complex. If complex is unstable, a repair is necessary; if stable, a débridement of damaged tissue may be adequate. Surgical repair has been very successful in allowing return to throwing, some reports approaching 90% (14).
labral complex from the bone. Burkhart et al. (13) support an acceleration mechanism of injury. As the shoulder is positioned in abduction and external rotation coinciding with late cocking and acceleration, the labrum is peeled off the glenoid rim. Kuhn et al. (17) performed experimental comparison of the two mechanisms in a cadaveric model; their results support the acceleration mechanism. Treatment is dictated by the stability of the biceps/labral complex. If complex is unstable, a repair is necessary; if stable, a débridement of damaged tissue may be adequate. Surgical repair has been very successful in allowing return to throwing, some reports approaching 90% (14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree