Thoracic and Lumbar Spine
Scott W. Eathorne
Back pain, specifically low back pain (LBP), is one of the most frequently encountered presenting symptoms in primary care and sports medicine offices. LBP is second only to the common cold as a reason for visiting the primary care physician (1). With a lifetime prevalence of 60% to 90%, annual incidence estimated at 5%, and estimated direct medical cost of treatment at $25 billion per year, LBP poses a significant challenge to the health care system and its providers (2). This challenge is made even more difficult by the fact that only 5% to 10% of individuals with LBP seek medical care for their symptoms. For the sports medicine provider, recognizing the prevalence of back pain in the overall community and preparing to recognize, diagnose, and effectively manage it in the athletic population is a matter of key competency.
Back pain is a symptom, not a diagnosis. Identifying its cause can be difficult given that potential etiologies include biomechanical, inflammatory, traumatic, infectious, developmental, neoplastic, metabolic, or emotional processes. Table 29.1 lists some of the diagnostic considerations for the athlete presenting with back pain. Considering such factors as the athlete’s age, chosen sport, position played, onset and mechanism of injury, and vocation can provide clues to help narrow the differential diagnosis. Developing a systematic approach to evaluating the athlete with back pain will make the task of sorting out potential causes more manageable.
The U.S. Agency for Healthcare Research and Quality (AHRQ) clinical practice guideline for acute low back problems in adults provides a useful framework for approaching the athlete with LBP. Although the guideline, published in 1994, has undergone scrutiny and other evidence-based guidelines have been developed, it continues to provide a useful approach to evaluating and managing this common problem (3,4,5). It emphasizes stratification of clinical signs and presenting symptoms to focus on those most likely associated with more severe causes of LBP requiring urgent recognition and treatment. The guideline suggests various imaging and treatment modalities evaluated for proven value in establishing a diagnosis and improving outcomes, both short and long term. As the title implies, the guideline only applies to the evaluation of acute pain in adults. This is because adults tend toward a myofascial etiology for their pain, whereas children, adolescents and seniors are more susceptible to developmental, infectious, neoplastic, and inflammatory conditions.
Anticipating which athletes may be at greatest risk for developing a spine injury can assist providers in focusing on prevention through preparticipation evaluation, specific training protocols, rules modification, and protective equipment. Those involved in sports with repetitive hyperextension of the spine (gymnasts, football lineman, dancers) can experience injury to the posterior elements, including facet joint syndrome and stress fractures of the pars interarticularis. Athletes whose sport requires violent trunk rotation (golf, tennis, field events) may suffer discrelated or myofascial injury. Active children and adolescents are vulnerable to stress fractures through the pars interarticularis (traumatic spondylolysis, spondylolisthesis), with seniors susceptible to age-related illnesses that may present as back pain (metastatic disease, osteoporotic fractures, infectious, metabolic, and inflammatory processes). This chapter will focus on the key elements in the evaluation and treatment of back pain in athletes and active individuals and discuss a few specific problems encountered in this population.
TABLE 29.1 Differential Diagnosis of Low Back Pain | ||||||
|---|---|---|---|---|---|---|
|
Anatomy/Biomechanics
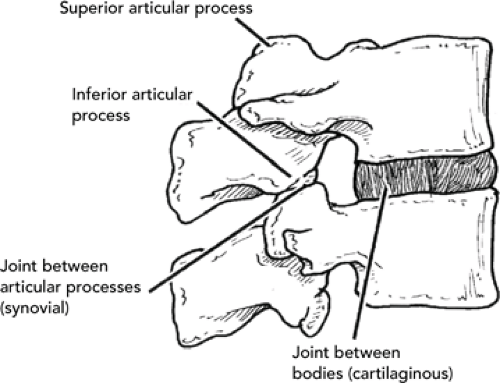
Understanding the anatomy and biomechanics of the spine and its related structures is key to understanding patterns of injury and presenting findings in the athlete with back pain. The basic functional unit of the spine consists of two adjacent vertebrae and the interverterbral disc that separates them (see Figure 29.1). This functional unit is the building block for the entire spine, which as a whole can be further subdivided into anterior and posterior elements to gain a better appreciation of the key functional role that each plays.
The vertebrae of the thoracolumbar spine consist of an anteriorly oriented vertebral body, composed of both cortical and cancellous bone, and the posterior elements, which form the vertebral foramen or spinal canal. Posterior elements include the pedicles, lamina (including the pars interarticularis), superior and inferior articular processes, and the transverse and spinous processes. Vertebral body size and weight-bearing capacity increase with progression from the cervical to lumbar spine. Cancellous bone contributes most to the load-bearing capacity of the vertebrae (6). At the superior and inferior surface of each vertebral body is a cartilaginous endplate, which undergoes circumferential ossification to form a ring apophysis. Fibers of the outer intervertebral disc annulus attach to this apophysis, with the avascular nucleus pulposus receiving nourishment through the central endplate, an important factor in understanding certain injury patterns in the developing spine.
The intervertebral discs consist of an outer annulus fibrosis and inner nucleus pulposus. The fibrocartilaginous annulus, slightly thicker anteriorly than posteriorly, consists of a ring of concentrically aligned outer fibers attached to the vertebral endplate. It is composed of 60% to 70% water, which remains relatively constant with age, and receives sensory innervation posteriorly from the sinuvertebral nerves and laterally by branches of the ventral rami and grey rami communicans (7). The nucleus pulposus consists of a hydrophilic, proteoglycan matrix contained by the lamellar annulus, with a water content that approximates 90% in infancy and follows a linear decline into adult life (8). It possesses an inherent internal pressure that provides separation and shock absorption between the adjacent vertebrae. There is no direct blood supply to the nucleus in adults and no direct innervation. The intervertebral discs are susceptible to failure through desiccation associated with the aging process and exposure to acute and repetitive traumatic effects, including compression, rotation, and shear forces.
Posteriorly, the superior articular process of the vertebrae below and the inferior articular process of the vertebrae above join to form a facet joint. This zygapophyseal joint is a paired synovial joint surrounded by a redundant capsule that allows for flexion and extension movement while restricting lateral flexion and rotation. Between the articular processes lies a fibroadipose meniscus, or meniscal equivalent, that is well innervated with proprioceptive and nociceptive fibers. The vertebral arch, formed by the lamina, the pedicles, and posterior aspect of the vertebral body form the vertebral canal, containing the spinal
cord. The spinal cord terminates at the level of the first lumbar vertebra, becoming the conus medullaris.
cord. The spinal cord terminates at the level of the first lumbar vertebra, becoming the conus medullaris.
The intervertebral foramen is formed by the pedicles above and below, the intervertebral disc and vertebral body anteriorly, and the lamina and anterior facet joint posteriorly. It contains the associated spinal nerve (see Table 29.2 for level) that occupies approximately 35% to 40% of the area, connective tissue, ligamentum flavum, arteries and veins, lymphatic vessels, and the sinuvertebral nerve. The L1–2 foramen has the largest cross-sectional diameter with L5-S1 having the smallest, while housing the largest nerve root (L5). This creates a level of vulnerability to injury from any relative change in the surrounding structures, such as disc protrusion, facet arthropathy, and local soft tissue swelling and edema.
The spinal nerve roots, carrying motor, sensory, and sympathetic fibers, are enclosed in a dural sheath that provides protection and nourishment to the root. The segmental organization of the spinal elements allows a “pattern” recognition of injury to a given level. Table 29.2 lists the more commonly affected lumbar nerve roots and the associated sensory, motor, and reflex changes. It is important to remember that a given nerve root may cross one to two vertebral levels before exiting the intervertebral foramen and may therefore be affected by pathology at a different level than predicted.
In addition to the elements of the columnar functional units, the static, erect spine is stabilized by a variety of other soft tissue structures, including muscular, ligamentous, and fascial supports. The intact spine consists of four physiological curves, a cervical and lumbar lordosis and thoracic and sacral kyphosis, which provide a spring-like mechanism to absorb shock and improve load bearing. Four muscle groups, the erector spinae, multifidus, intersegmental, and quadratus lumborum, compose the thoracolumbar paraspinal muscle mass. The erector spinae group, the predominant extensors of the lumbar spine, lies lateral to the multifidi, consists of longissimus, iliocostalis, and spinalis groups, and attaches from the pelvis to the thoracic and lumbar spinal elements and ribs. The more medial multifidae originate at the lumbar lamina and spinous processes and attach at the sacrum, acting to extend the spine, rotate to the opposite side, and control deceleration of forceful spinal flexion. The intersegmental muscles, intertransversalis and interspinalis, attach to adjacent transverse and spinous processes, and laterally bend to the ipsilateral side and extend the spine, respectively. The quadratus lumborum, a powerful lateral trunk flexor, attaches to the 12th rib, iliac crest, and transverse processes of the lumbar vertebrae.
In addition, various other muscle groups exert effects on the thoracolumbar spine, and include the glutei, hamstrings, quadriceps, latissimus dorsi, iliopsoas, and the anterior abdominals—rectus abdominus and abdominal obliques. Further support is provided by the thoracolumbar fascia that encloses the erector spinae and quadratus lumborum muscles. Additional stability is afforded by the ligaments acting on the bony spine, including the ligamentum flavum, supraspinatus ligament, interspinous ligament, and the anterior and posterior longitudinal ligament (see Figure 29.2).
Coordinating the various structural elements of the spine to produce a functional outcome is a complex, highly integrated system of neurophysiological and biomechanical processes. A three-system theory, consisting of neural, passive, and active components,
has been proposed to help explain this complex interaction (9). The neural component initiates the precise movement and coordinates all motion factors. The passive component consists of the static structures discussed previously, including discs, facet joints and capsules, and ligaments. The active component includes the various muscles and ligaments acting on the passive structures. The effective interaction of the three components constitutes the kinetic or dynamic spine. Any breakdown in the function of one or more components can produce a mechanical irritation that triggers a pain response and altered function.
has been proposed to help explain this complex interaction (9). The neural component initiates the precise movement and coordinates all motion factors. The passive component consists of the static structures discussed previously, including discs, facet joints and capsules, and ligaments. The active component includes the various muscles and ligaments acting on the passive structures. The effective interaction of the three components constitutes the kinetic or dynamic spine. Any breakdown in the function of one or more components can produce a mechanical irritation that triggers a pain response and altered function.
TABLE 29.2 Lumbar Nerve Roots and Associated Sensory, Motor, and Reflex Distribution | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
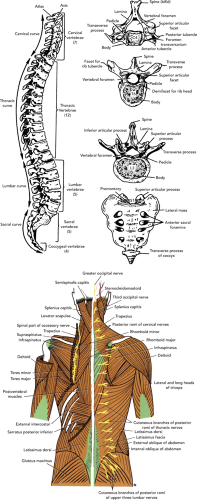 Figure 29.2 Lumbar myofascial anatomy: (A) osseous and ligamentous structures, (B) myofascial anatomy. |
Pain is generated when nociceptive fibers are stimulated by mechanical or chemical means. A number of structures in the back possess such fibers and are therefore potential pain generators. These include the disc annulus, anterior and posterior longitudinal ligaments, facet joint capsule, and various other muscular and other ligamentous groups. Trauma, either micro or macro, activates a cascade of events leading to the release of the chemical mediators of pain, including bradykinins, prostaglandins, leukotrienes, and histamines. In addition, there are psychosocial factors that
impact an individual’s subjective pain experience and may play a significant role in the athlete with back pain.
impact an individual’s subjective pain experience and may play a significant role in the athlete with back pain.
Approach to Diagnosis
A directed history and physical examination, cognizant of key elements needed to rule in or out specific disorders, is key to developing an accurate differential diagnosis and selecting appropriate further diagnostics and treatment interventions. The AHRQ guidelines for acute low back problems in adults provides a useful starting point for developing an initial approach to the athlete with LBP, recognizing the limitations inherent in the guideline, including age restriction and chronicity.
History
Important demographical factors include athlete’s age, sex, sport and position played, skill level, vocation, and other recreational or training activities that may be relevant to their presenting complaint. In evaluating the complaint of back pain, it is imperative to gather information on its onset, duration, nature, location, and severity, as well as any palliative or provocative factors that relate to the pain. Understanding a specific mechanism of injury can target the likely structures injured. Any history of previous back pain episodes and earlier or current interventions is also helpful in establishing a chronic or recurrent pattern of injury and success of treatment. Past medical and surgical history, tobacco and alcohol use, and family history may reveal clues
helpful in assessing the current pain. One of the key aspects of gathering history in acute LBP is the ability to begin differentiating axial back pain from back pain associated with leg pain, an important step in developing an accurate differential diagnosis. Table 29.3 lists various potential etiologies for LBP and associated key features or symptoms.
helpful in assessing the current pain. One of the key aspects of gathering history in acute LBP is the ability to begin differentiating axial back pain from back pain associated with leg pain, an important step in developing an accurate differential diagnosis. Table 29.3 lists various potential etiologies for LBP and associated key features or symptoms.
Key “red flag” historical factors include the presence of fever, chills, night pain and other constitutional symptoms, a history of cancer, recent urinary tract infection, intravenous drug use, age over 50 or under 20 (infection, tumor), saddle anesthesia, recent onset bladder or bowel dysfunction, severe or progressive neurological deficit in the lower extremity (cauda equina syndrome), and major trauma such as motor vehicle accident (MVA) or fall or minor trauma in an osteoporotic individual (fracture) (4). The presence of such factors should warrant timely investigation aimed at ruling out the listed underlying etiology (see Table 29.4).
TABLE 29.3 Potential Pain Syndromes and Their Associated Symptoms | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 29.4 Red Flag Signs and Symptoms | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
A nutritional history may be of value, particularly in the young, female athlete. Decreased caloric intake can be associated with decreased calcium stores and place the adolescent female at risk for osteopenia and stress fractures (pars interarticularis, sacrum) (10,11). Surveying for recent growth spurts in the young athlete may also be of diagnostic value. Athletes should be questioned regarding the use of assistive devices, both for management of back symptoms as well as those used for other purposes as they may impact spine mechanics. The use of patient- or parent-completed questionnaires and pain diagrams can be helpful in gathering historical data and understanding the athlete’s reaction to their symptoms.
Physical Examination
The physical examination of the athlete with back pain should be systematic and driven by historical findings. An overall assessment of the athlete’s appearance, including posture, facial expression, and position when encountered (sitting, standing, supine), is a key step in understanding the severity of pain and degree of disability. Observing




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree