Thermoregulation
considerations for aging people
John Sanko
Introduction
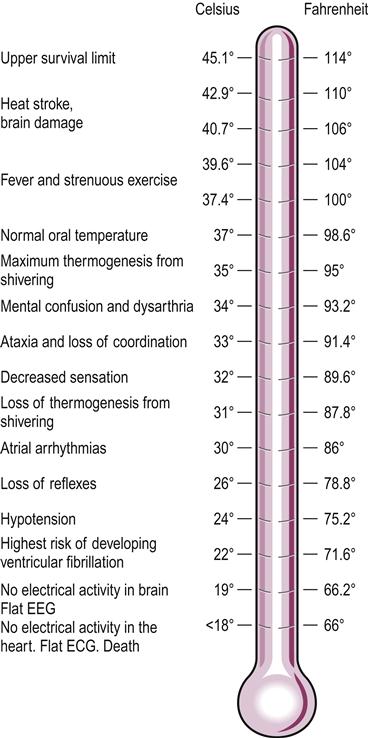
Core body temperature is a relatively stable physiological function and one of the most frequently measured vital signs. Core temperature normally does not vary by more than±0.55°C (±1°F) unless a febrile illness develops (Gonzalez et al., 2001). Humans like other mammals are warm-blooded homeotherms, which means they must maintain their internal temperature within a narrow range, which in humans hovers near 37°C (98.6°F). Life-sustaining biochemical processes are altered if the internal environment deviates from the optimal. Internal temperatures above 45–50°C (113–122°F) denature the protein structure of various enzymes, which results in biochemical breakdown, tissue destruction, severe illness and death (Fig. 10.1). Body temperatures below 33.9°C (93°F) slow metabolism to dangerously low levels and disrupt nerve conduction, which, in turn, results in decreased brain activity. Life-threatening cardiac arrhythmias begin to appear at temperatures near 30°C (86°F) (see Fig. 10.1).
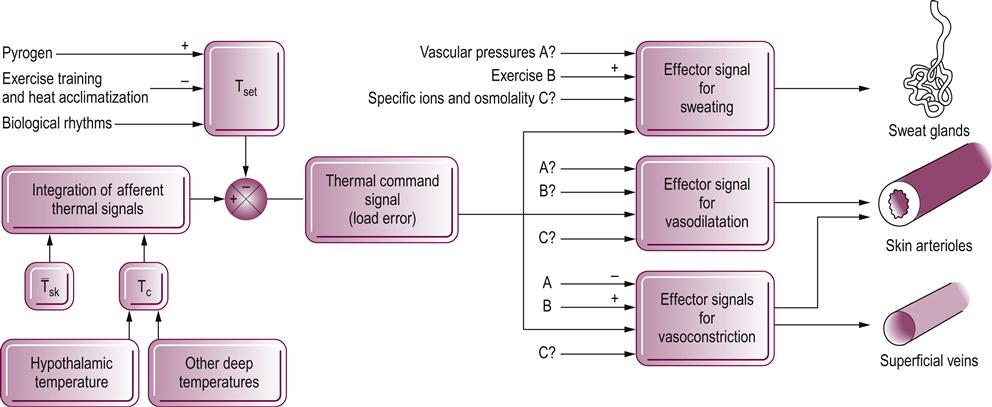
All warm-blooded animals, including humans, live only a few degrees away from death (Astrand et al., 2003). Core temperatures falling outside the normal range are indicative of some pathology or the failure of the thermoregulatory system to maintain homeostatic thermal balance. The complexity of the physiological mechanisms involved in thermoregulation is shown in Figure 10.2. The effect of aging and the interaction of normal aging with and lifestyle changes on an individual’s ability to regulate body temperature are not fully understood. Changes in body composition, decreased aerobic capacity, sedentary lifestyle and the increased prevalence of chronic diseases such as heart disease, diabetes and decreased kidney function along with the increased use of prescription drugs makes it difficult to determine the true impact aging has on thermoregulation (Kenney & Munce, 2003). It is clear, however, that the fitter, more active and healthy an older individual, the more able they will be able to withstand a thermoregulatory challenge.
Hyperthermia
Hyperthermia is the condition in which internal core temperature exceeds the normal range. Hyperthermia can be caused by infections, brain lesions, environmental conditions or heavy exercise. When caused by an infection, the responsible microorganisms release toxins called pyrogens into the bloodstream; they reach the temperature control centers of the brain and raise the thermal set point. This state, known as fever, is actually beneficial and is part of the immune system’s response (see Chapter 11). Higher core temperatures adversely affect the invading microorganism’s ability to replicate. This generally limits the extent of the infection and leads to its suppression.
In the older adult, the fever response is often diminished or absent, which may explain the increased morbidity and mortality rates associated with infections in the elderly (Blatteis, 2011). When the ambient temperature rises above 30°C (86°F), progressive vasodilatation of the cutaneous vasculature commences and is followed by sweating and evaporation (Gonzalez et al., 2001). Factors such as high humidity and physical activity magnify the effects of ambient temperature, taxing the thermoregulatory mechanisms. This is an especially important factor in home healthcare when treating debilitated patients. Unlike fever, non-febrile rises in body temperature are not beneficial and threaten homeostasis. If normal thermal regulation is in any way impaired, these increases can reach dangerous levels. With core temperatures above 40.7°C (106°F), heat stroke and irreversible brain damage becomes imminent (see Fig. 10.1).
If the internal core temperature drops below 34.1°C (94°F), the ability of the hypothalamus to regulate body temperature is also severely impaired (Gonzalez et al., 2001). If the body temperature continues to fall unchecked, loss of motor control, sensation and consciousness will be followed by ventricular fibrillation and death see (Fig. 10.1).
Hypothalamus and thermal regulation
The hypothalamus normally acts as the body’s thermostat, initiating heat-dissipating, heat-conserving, or heat-generating mechanisms in relation to internal core and body surface temperatures (Gonzalez et al., 2001). The temperature-reduction mechanisms include vasodilatation, sweating, inhibition of shivering, and decreased chemical thermogenesis. When body temperature begins to rise, sympathetic outflow from the hypothalamus to the cutaneous vasculature is inhibited, allowing for vasodilatation and increased heat transfer from the skin to the external environment. This mechanism is capable of increasing heat dissipation through the skin by as much as 800%. Sweating and evaporative loss further enhance the skin’s ability to dissipate heat. When the challenge of cold is presented to the body, the hypothalamus conserves or generates body heat by measuring sympathetic tone, which results in vasoconstriction of the cutaneous circulation, piloerection, shivering and increased metabolism through the secretion of thyroxine (Gonzalez et al., 2001; Hall, 2010). The efficiency of these mechanisms may be altered by skin atrophy, diminished vascular tree and reduced muscle mass, which are discussed in greater detail below.
Mobility and psychosocial factors
In spite of the exquisite physiological mechanisms for dealing with temperature change, behavioral modification may be human beings’ greatest defense against environmental challenges to thermoregulatory homeostasis. When our surroundings become too warm or too cold we try to avoid such conditions by moving to a more comfortable location or changing the thermostat or control for the heating or air conditioning. In addition, we may add or remove clothing as conditions warrant. The very young, the elderly and those physically or mentally unable to take care of themselves are at the greatest risk when exposed to extremes of environmental conditions. This may be due in part to their inability to recognize the magnitude of the situation and take appropriate action.
Older adults often find themselves dependent upon others for their wellbeing, commonly as a result of deficits in physical or cognitive function. The incidence of chronic disease increases dramatically with age. Over 50% of those beyond 65 years of age report some limitation in mobility due to arthritis and a significant number have other orthopedic problems that limit their ability to carry out the normal activities of daily living (ADLs) (Guccione, 2011). Musculoskeletal and neurological conditions often reduce the older adult’s functional level to a point where he or she becomes partially, if not fully, dependent upon others to carry out the ADLs. Thermoregulatory stress may be one of many reasons why elderly people who are dependent on others for help with ADLs have a four times greater chance of dying within a 2-year period than those who are totally independent. In addition, approximately 15% of the population over 65 years of age are in some way cognitively impaired. The incidence of cognitive impairment rises rapidly with age. Some deterioration in mental function is seen in nearly 50% of those individuals 85 years of age and older (Guccione, 2011). These physical and mental impairments, as well as others, combined with a reduction in the functional capacity of various organ systems make the older adult particularly vulnerable to thermoregulatory stress. Thermoregulation and aging has been studied from a physiological basis for some time, but added emphasis has recently focused on the area of behavioral thermoregulation. A great deal of research needs to be done on the relationship between thermal comfort and thermal sensation. Thermal comfort is defined as a state of mind of whether the individual feels satisfaction or dissatisfaction with ambient conditions while thermal sensation is the perception resulting from the stimulation of the body’s thermoreceptors (Flouris, 2010). Autonomic response to temperature change, although essential, may not be as powerful and important to our survival as behavioral thermoregulation (Romanovsky, 2007; Van Someren, 2007).
Thermal injury
Heat stroke, heat exhaustion and hypothermia are most prevalent among the elderly population and are inversely related to socioeconomic status. A study in Hong Kong showed an increase in mean environmental temperature of 1°C above 28.2°C (82.76°F) resulted in a 1.5% increase in mortality over a 2-week period. Those affected most were individuals over 75 years of age, the unmarried and women (Chan et al., 2011). Similarly, a study of ambulance calls, emergency department visits and mortality in Australia during a 12-day heatwave in 2011 once again showed those over 75 years of age to be the most impacted (Schaffer et al., 2012). When elderly individuals on fixed incomes turn the heat down in the winter because they cannot pay high heating bills, they are certainly predisposing themselves to hypothermia. Conversely, elderly people unable to afford air conditioning are 50 times more likely to die of heat stroke than those who have access to air conditioning (Wongsurawat, 1994). Although it has been stated that numerous predisposing physiological factors share responsibility, many temperature-related threats to health could undoubtedly be prevented if elderly individuals just stayed indoors, turned the heat or air conditioning up or down, and dressed more appropriately (Gonzalez et al., 2001). In cases in which economic status or physical or mental condition makes these actions impossible, those involved should be referred to the appropriate agencies for their protection, safety and welfare.
Physiological factors
Skin receptors and circulatory response
Even when they are healthy and mentally alert, the elderly are less able to sense changes in skin temperature, and this makes them more susceptible to thermoregulatory problems (Gonzalez et al., 2001). Thermoreceptors for both hot and cold are found in the skin, the spinal cord and the hypothalamus itself. Skin temperature, unlike core temperature, is extremely variable. Receptors in the skin provide the hypothalamus with important feedback regarding the need to dissipate, conserve, or generate heat. Numerous bare nerve endings just below the skin are sensitive to heat and cold. They are classified as warm or cold receptors, depending on their rate of discharge when exposed to variations in temperature. It is not known whether the effectiveness of these thermoreceptors declines with age. However, because their function depends on an adequate oxygen supply, it seems reasonable to assume that any age-associated impairments in cutaneous circulation would reduce the effectiveness of thermoreceptors. It is known that the dermis becomes thinner and less vascularized with age (Farage et al., 2010).
The changes in skin thickness and circulation along with reduced autonomic nervous system function alter the effectiveness of the vasomotor response. The vasomotor mechanism can alter cutaneous blood flow from near zero when exposed to extreme cold to increases of 500–1000% when exposed to vigorous warming. The evaporative loss of sweat from the skin surface helps to dissipate heat in the cutaneous circulation. A study that compared men aged 45–57 years with men aged l8–23 years indicated that the older men required twice as long before the onset of sweating during moderate intensity exercise. Subsequent studies of older women showed even greater impairments in the sweating mechanism. The number of sweat glands does not appear to change significantly with aging. Therefore, it is reasonable to assume that the decline in autonomic nervous system function reduces the performance of sweat glands and alters the body’s ability to dissipate excess heat. In addition, the hypothalamus appears to become less sensitive to temperature variations, and there is evidence of age-correlated reductions in autonomic nervous system function (Hall, 2010).
It is unclear how much of the thermoregulatory impairment seen in the elderly is age-related and how much is the result of chronic disease processes and a sedentary lifestyle. The efficiency of the cardiovascular system’s ability to dissipate body heat is enhanced by aerobic fitness. Resistive exercise has been found to be particularly beneficial in maintaining or retarding muscle loss in the elderly and should be considered when not contraindicated. Muscle is a significant tissue not only for heat generation, but also for the mobility needed for thermoregulation.
Other physiological factors
The ingestion of food, alcohol and medications to control blood pressure, cardiac function, depression and pain all exert influence on thermal balance and regulation. A sufficient, well-balanced diet is essential to provide the calories needed to generate heat and maintain adequate levels of metabolically active muscles. Muscle, which is the major organ of metabolism and heat generation, can decrease by 10–12% in the older adult. One-third of the US population over 65 has some form of nutritional deficit, often eating inappropriate quantities of foods low in nutritional values. Reduced caloric intake, lower basal metabolic rate, reduced lean body mass and lower cardiac output may all contribute to thermoregulatory changes in the aging adult (Novieto & Zhang, 2010). Because 80% of the calories consumed go toward the maintenance of body temperature, this deficit can further contribute to the thermoregulatory inadequacies experienced by some older adults. The shivering mechanism, which can increase metabolism and heat generation by 300–500%, is also adversely affected by the loss of muscle tissue (Gonzalez et al., 2001).
Possible effects of medication
Although there is still a great deal to be learned regarding the effects of aging on the thermoregulatory function, it appears that physical conditioning and adequate nutrition help to preserve this function in healthy older adults. All older individuals are, however, not healthy or physically fit. Many have chronic conditions that interfere with their abilities to deal with even mild variations in temperature (Kenny et al., 2010). In addition, various medications can interfere with the normal physiological responses necessary to maintain thermal homeostasis. Dehydration may occur in individuals taking diuretics for the management of congestive heart failure or hypertension. Beta-antagonists are another category of medication commonly prescribed for elderly individuals with heart disease and hypertension. Because they slow the heart rate and affect circulation they can have an effect on thermoregulation.
Although the use of illicit drugs is lowest among the elderly, the misuse of prescription drugs is a major problem for this group. In one survey of elderly persons living independently in the community, 83% reported they were using two or more prescription drugs, with an average of 3.8 medications per person (Hooyman & Kiyak, 2010). Many elderly people have been found to misuse prescription and nonprescription over-the-counter drugs. Surveyed individuals reported taking two to three times the recommended dosages of aspirin, laxatives and sleeping pills. Misuse of laxatives could further increase the rate and severity of dehydration and sedatives defeat the autonomic nervous system’s ability to react to environmental conditions. In addition, psychotropic drugs are often prescribed for depression in the elderly. Several studies have demonstrated that the inhibition of the sweating reflex by these drugs increases the risk of death during prolonged heatwaves (Nordon et al., 2009).
Alcohol also inhibits the body’s ability to regulate temperature by interfering with the vasomotor system and altering cutaneous blood flow, which impairs the body’s ability to dissipate or conserve heat. The dehydrating effects of alcohol can also contribute to an inadequate thermoregulatory response by reducing plasma volume and decreasing the sweat response. Combined with prescription and nonprescription medications, alcohol can create serious problems for any individual.
Postsurgical considerations
A number of geriatric patients receiving physical therapy in acute and extended care facilities are postsurgical patients. The tremendous advancements and successes in joint replacement surgery have made these procedures relatively commonplace. Plasma lost during surgery may result in some degree of dehydration, but anesthetics present the greater challenge to thermoregulation for these patients. Most anesthetics and sedatives impair the body’s ability to maintain core temperature by blocking the normal heat-generating activity. There are some benefits of mild hypothermia for the surgical patient, but there are also increased risks for the elderly. A 2°C (3.6°F) drop in core temperature has been shown to substantially increase blood loss during hip arthroplasty surgery. The incidence of ischemic myocardial events increases for a 24-hour period following intraoperative hypothermia. Higher rates of wound infections, delayed healing and immunosuppression are also seen following anesthesia-induced hypothermia. The elderly appear to be at the greatest risk for developing one or more of these complications because of their predisposition to hypothermia, even when exposed to only moderately cold conditions (Mayer & Sessler, 2004).
Clinical considerations
In spite of the fact that numerous age-correlated alterations in thermoregulation have been identified, the ability to regulate internal core temperature appears to remain within acceptable limits in the healthy, fit older adult. Furthermore, few of the changes seen in autonomic, circulatory and thermal function are solely the result of biological aging. Reduced physical work capacity, body composition changes, chronic illness, the use and misuse of various medications, and alterations in cognitive function become more prevalent with advancing age and influence the function of various body systems involved with thermoregulation. Studies on thermoregulation and aging have generally shown that aging reduces sweat gland output, skin blood flow, cardiac output, peripheral vasoconstriction and reduced muscle mass. In spite of these changes, healthy older individuals seem to be able to handle most variations in ambient temperature. Gender may also play an important role. Although both males and females lose muscle mass as they age, females tend to have a greater increase in percentage body fat, which may account for their ability to better maintain core temperature when exposed to cooler ambient temperatures (Kenney & Munce, 2003).
Whenever treating any individual with exercise or thermal modalities, age should be a consideration. Ideally, the ambient temperature in exercise areas should be 19.8–22°C (68–72°F) with a relative humidity of 60% or less. When exercise is to be performed outdoors, appropriate clothing is a necessity. Planning outdoor activities during moderate weather is also important. It would not be prudent to exercise in mid-afternoon on a hot summer day or late in the evening on a cold winter day. Because older adults may build up heat more quickly and take longer to dissipate it than their younger counterparts, frequent rest periods in well-ventilated areas should be incorporated into any exercise regimen.
Conclusion
The safe and effective use of exercise, heat, cold, or hydrotherapy requires thorough assessment of the individual’s condition, medical history, and ability to withstand thermal or cryogenic stress. A past medical history of hypersensitivity to heat or cold, Raynaud’s disease, urticaria, wheals, diabetes or heart disease requires further consideration prior to intervention. Pain and temperature sensation should be assessed.
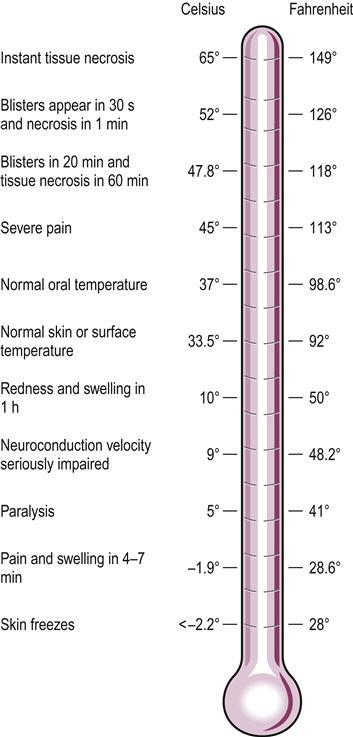
The normal effects of direct heating and cooling of the tissue may be altered in some elderly individuals (Fig. 10.3). Vital signs should be monitored along with skin temperature, sensation, color, sweat rate, and rate of perceived exertion (RPE). Additional care should be taken with individuals on medication and those who have impaired cognitive and mental function. Physiologically elderly individuals will have changes in their ability to regulate the internal temperature that will be magnified by a host of comorbidities and other factors, so ensuring appropriate thermoregulation behaviors may become the responsibility of the caregiver.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree