The Use of Cages and Reconstruction Rings for Acetabular Revision
Kenneth A. Estrera
Michael H. Huo
Case Presentation
The patient was a 64-year-old male with a complex history related to his left total hip arthroplasty (THA) that was implanted over 30 years ago. He underwent multiple revisions with his most recent surgery involving a jumbo cup with a posterior column augment to address a massive acetabular defect. This reconstruction failed with progressive migration of the acetabular implants at a year following the revision. He was presented to clinic for preoperative evaluation denying any history of venous thromboembolism, infection, or nerve injury. Laboratory results for infectious serology testing were not elevated.
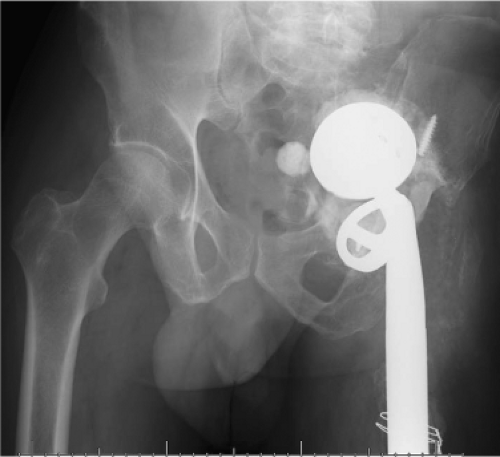
On physical examination he had a significant leg-length discrepancy with his left leg being over 4 cm shorter than his right. Radiographic evaluation demonstrated massive bone deficiency with a severe medial defect and superomedial migration of the hip center (Fig. 113.1). This particular pattern of bone deficiency was assessed to be Paprosky type IIIB with violation of Kohler line, osteolysis affecting the ischium, and loss of the teardrop. The plan for revision included the use of an acetabular cage for reconstruction.
Introduction
Total hip arthroplasty (THA) is one of the most successful reconstructive operations in orthopedic surgery over the past 5 decades. Based on projected population data between 2005 and 2030, the annual volume of primary THAs is projected to increase by 174%. The burden of revision hip arthroplasty is estimated to double by the year 2026 (1). It is believed that revision THAs will not only increase in volume, but also in the complexity of the reconstruction as THAs have been extended to younger and more active patients who could potentially require multiple revisions over their lifetime.
The demand for an effective long-term solution in acetabular revision THAs led to the evolution of porous-coated uncemented components. Uncemented cups in revision THAs have had excellent overall success with greater than 90% implant survival at 10 years or longer (2,3,4). Despite the overall success of uncemented cups in revision surgery, the same success has been inconsistent in the subset of patients with severe acetabular bone loss. Insufficient bone support in these patients compromises cup fixation stability eventually leading to mechanical fixation failure. A variety of surgical techniques have been utilized to address major acetabular bone deficiencies. These options include the following: (1) uncemented or cemented cups at a high hip center, (2) jumbo uncemented cups, (3) oblong cups, (4) adjunct modular metallic porous augments, (5) custom triflange components, and (6) pelvic reinforcement cage devices. Moreover, in many cases the use of structural allograft is also required to provide the necessary support for durable cup fixation. The wide array of surgical options are indicative of the challenges associated with these complex acetabular revisions. This chapter will focus on the use of pelvis cages in acetabular revision surgery.
Indications
The surgical principles of any revision THA include the following: (1) stable component fixation, (2) restoration of the normal hip center and biomechanics, (3) equalization of leg lengths, and (4) preservation and if possible, restoration of bone stock. Patients with severe acetabular deficiencies pose a formidable challenge to the surgeons in achieving these reconstructive goals. Uncemented cups have proven to be a reliable option in revision surgery by providing durable long-term fixation stability through osseointegration of the implants. The main indications for the use of reconstruction rings and cages are in cases with severe acetabular structural bone loss or pelvic discontinuity that will not predictably support an uncemented cup.
The antiprotrusio cage was developed over 30 years ago for the purpose of managing large acetabular deficiencies (5). It has been established with clinical and laboratory testing studies that less than 50% host bone support is one of the principle indications for the use of pelvic reinforcement devices (6,7,8). Several classification systems have been developed to evaluate the acetabular defects and to guide surgical decision making. The three most commonly used classification systems are the American Academy of Orthopedic Surgeons (AAOS) system, the Gross system, and the Paprosky system (9,10,11).
The AAOS system provides a description of the bone defects based on either cavitary and/or segmental patterns. The contained cavitary patterns describe defects with a volumetric loss and preserved acetabular rim. The uncontained segmental patterns are associated with defects involving the structural support of the acetabulum (10). The lack of quantifiable information regarding the deficiency has made the AAOS classification less helpful in guiding treatment plans (12). The Gross system also identifies contained or uncontained deficiencies. This system further defines the percentage of the defects by quantifying whether they involve greater or less than 50% of the host acetabulum (10). The Paprosky classification is a more complex system based on specific radiographic patterns that can effectively be used to predict the location and extent of bone loss assessed intraoperatively. Tear drop osteolysis, ischial osteolysis, superior migration of the hip center, and migration beyond the Kohler line all represent specific areas of acetabular bone loss that can be assessed prior to surgery (12). The radiographic evaluation can be used as a guide for preoperative planning, but the definitive assessment of the acetabular defect should be determined intraoperatively after excision of the fibrous membrane, retained cement, and other hardware from the acetabular fossa. The inherent cup stability should also be assessed with intraoperative testing of the trial components. Paprosky Type II defects have inherent fixation stability as there is intact rim support and >50% host bone contact. Paprosky Type III defects lack predictable cup stability due to insufficient rim and host bone support (13).
Based on the Gross classification, contained defects (Type II) and uncontained defects involving less than 50% of the acetabulum (Type III) can be treated with uncemented cups with adjunct screw fixation (14). In the Paprosky classification, the Type I, II, and IIIA defects have the potential for biologic fixation with uncemented cups (12). Gross Type IV, Paprosky Type IIIB, and pelvic discontinuity represent the patterns and the severity of bone deficiency that will not predictably provide long-term structural support for conventional uncemented cups. Cages, custom implants, augments, structural grafts, and other reconstructive options are necessary in these most severe acetabular deficiencies.
Reconstruction cages are also ideal for cases where there has been pelvic irradiation. In cases where high-dose irradiation has led to necrosis of the acetabular bed, biologic ingrowth will not occur and in these cases both cemented and cementless constructs perform poorly (15). Hence the strong mechanical construct provided by a reconstruction cage is ideal in this situation.
Several design characteristics of a pelvis reinforcement cage are suitable in addressing major bone deficiencies (16




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree