The Trochanteric Slide for Exposure in Revision Total Hip Arthroplasty
Mansour Abolghasemian
Hesham Abdelbary
David Backstein
Oleg Safir
Allan E. Gross
Case Presentation
A 66-year-old patient presenting with worsening right groin pain following a total hip arthroplasty (THA) performed 13 years earlier. Physical examination showed pain originating from the hip joint. Workup for infection was negative. Plain x-rays showed loosening of the acetabular component and severe protrusion with associated pelvic bone loss (Fig. 103.1). The patient was indicated revision of the acetabular component with a trochanteric slide osteotomy (TSO) to facilitate exposure.
Introduction
Most hip revision surgeries require an expansile exposure to allow for proper visualization and reconstruction of the acetabular and femoral sides; the TSO provides such expansile exposure. Originally, Sir John Charnley introduced a transtrochanteric approach for his primary THA, but it was associated with a high rate of complications, especially nonunion (1). One of the biomechanical reasons for this high rate of nonunion is the unopposed superior and anterior shear forces applied by the abductors on the trochanteric fragment (2). Numerous modifications of the transtrochanteric approach have been attempted to reduce the risk of nonunion (3,4,5,6).
 Figure 103.1. Plain x-rays of a 66-year-old male showing loosening of the acetabular component and severe protrusion with associated pelvic bone loss. |
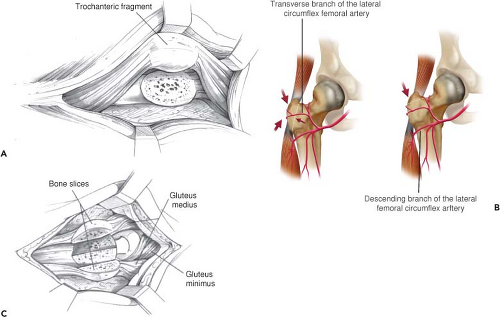
The TSO is a modification of the transtrochanteric approach that has been shown to decrease the risks of nonunion and migration. The principle of the TSO is to maintain a continuous soft tissue sleeve of the abductors and the vastus lateralis attachments to the osteotomized trochanteric fragment (Fig. 103.2A) (5). After the osteotomy of the trochanter is performed, this whole sleeve is mobilized anteriorly as one unit. This approach offers two main advantages over a standard trochanteric osteotomy: (1) maintaining the attachment of the vastus lateralis converts shear forces into compressive forces that provide inherent stability to the osteotomy, and restricts proximal migration of the trochanteric fragment and (2) maintenance of the vascularity to the osteotomy by preserving branches of the internal iliac artery proximally and the descending branch of the lateral circumflex distally (Fig. 103.2B) (7).
McFarland and Osborne (8) first described the technique of preserving a continuous soft tissue sleeve of the gluteus medius and vastus lateralis during a lateral approach to the hip joint, but by elevating the sleeve directly of the greater trochanter (GT). This approach was further modified by English (5) in 1975, where he osteotomized part of the GT with the attachments of the vastus lateralis and gluteal muscles. Glassman (9) in 1987 further popularized this approach for hip revision arthroplasty. His preference, however, was to leave the gluteus minimus attached to the shaft and not to the GT. This was shown later to be unnecessary and a potential cause for nonunion because of damage to the vascular supply of the GT (10).
Fulkerson et al. (11) described a technique of preserving the posterior soft tissues and releasing the anterior attachment of abductor muscles to reflect the GT posteriorly rather
than anteriorly. He thought that posterior translation of the GT during the procedure and its reattachment at the conclusion of the surgery would be easier. This technique has since been abandoned because of the mechanical and biologic disadvantages of detaching the anterior gluteal muscle insertion. Strachathro used a muscle splitting approach in which the GT was cut into anterior and posterior halves and reflected to the corresponding directions with the attached muscles to the proximal and distal borders (Fig. 103.2C) (12). The main advantage was the ease of repair and the low incidence of trochanteric bursitis.
than anteriorly. He thought that posterior translation of the GT during the procedure and its reattachment at the conclusion of the surgery would be easier. This technique has since been abandoned because of the mechanical and biologic disadvantages of detaching the anterior gluteal muscle insertion. Strachathro used a muscle splitting approach in which the GT was cut into anterior and posterior halves and reflected to the corresponding directions with the attached muscles to the proximal and distal borders (Fig. 103.2C) (12). The main advantage was the ease of repair and the low incidence of trochanteric bursitis.
The indications for TSO in revision THA are (1) need for adequate exposure of ischium and ilium for implant removal, acetabular reconstruction, or insertion of a cage or a cup-cage construct, (2) lengthening the limb by more than 3 cm, (3) removal of a well-fixed proximally porous-coated femoral implant, and (4) situations requiring GT advancement. There are a few relative contraindications for performing a TSO including (1) presence of nonunion from previous trochanteric osteotomy, (2) deficiency of the abductor mechanism, (3) radiation treatment to the hip region, (4) deficiency of proximal femoral bone stock as there will be an inadequate bed for healing of the osteotomy; in this situation an extended trochanteric osteotomy is preferred, and (5) severe osteoporosis which can compromise adequate fixation of the GT.
Biomechanics of Trochanteric Slide Osteotomy
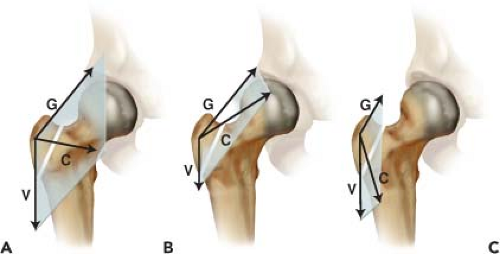
The main biomechanical advantage of TSO over a standard transtrochanteric osteotomy is the conversion of shear forces to compression at the osteotomy site. The magnitude of this compressive force depends on the orientation and the angle formed by the vectors of the two forces pulling on the GT fragment: the abductor force proximally and the vastus lateralis force distally (5). The wider the angle between these two vectors (i.e., closer to 180 degrees), or the greater the imbalance in their forces, will result in less of a total compressive force applied to the osteotomy. Therefore, a decrease in medial offset will diminish the overall compression forces at the osteotomy site. Further, the distal transfer of the hip center of rotation or the detachment/weakening of the vastus lateralis creates an imbalance in the forces pulling on the GT favoring the gluteal muscles, which will increase the shearing force on the GT fragment (Fig. 103.3). A biomechanical study on six cadavers performed by Plausinis et al. (2) calculated that
if 75% of the vastus lateralis attachment to the vastus ridge is intact, the GT fragment can be secured with six interosseous sutures to resist the applied shear forces by the abductors.
if 75% of the vastus lateralis attachment to the vastus ridge is intact, the GT fragment can be secured with six interosseous sutures to resist the applied shear forces by the abductors.
Schoeniger et al. (13) modified the TSO technique by including a 5-mm step to the osteotomy to hinder proximal migration in 20- to 30-degree anteroinferior inclination to resist anterior migration. Clinical results of this technique were assessed by Bastian et al. (14) which showed better results in hips that received a 6-mm step osteotomy, compared to hips treated by a 3- to 4-mm step cut. The fixation was carried out with the use of two 3.5-mm cortical screws. Although the results of this modification is promising to decrease rates of nonunion, it might not be technically feasible in revision hip surgeries where the GT is often thin and does not allow for a 6-mm step cut.
Surgical Technique
Approach
The surgery is performed while the patient is in the lateral decubitus position. The operative limb is prepped and free draped proximal to the iliac crest and to the midline. This wide draping ensures adequate access to extend the incision proximally and posteriorly if required. Either a posterolateral or a direct lateral approach can be used to perform a TSO, but our group prefers the lateral approach because it allows for a more anatomical repair at the end of the procedure, compared to the posterolateral approach.
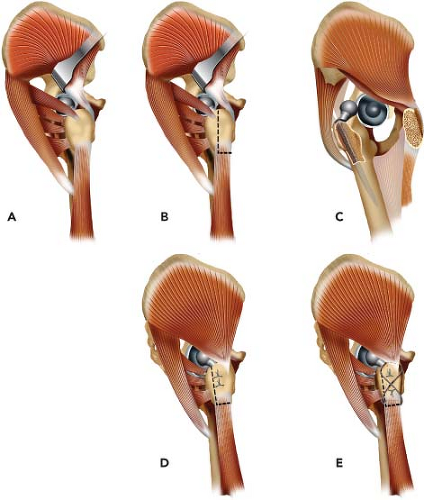
We start with a standard direct lateral incision over the GT incorporating the prior surgical incisions if possible. The iliotibial band is incised longitudinally over the vastus lateralis ridge and curving slightly posteriorly and proximally. The hip is rotated internally in slight flexion by placing a bolster under the shin. This position helps the visualization of the posterior structures, which are all protected during this approach to decrease the risk for posterior instability (15). The next step is to identify the interval between the piriformis and the gluteus minimus tendons. The posterior borders of the gluteus medius and minimus are elevated anteriorly with a right-angle retractor (Fig. 103.4A) to expose the location for the TSO, which starts just anterior to the silver-white tendon of the piriformis muscle and courses about 1 cm anterior to the insertion of short external rotators (Fig. 103.4B). This is our modification of the TSO that preserves the posterior soft tissue attachment to the proximal femur. The osteotomy will extend distally along the posterolateral border of the GT and exit just distal to the vastus lateralis ridge (Fig. 103.4B).
Before performing the osteotomy, the vastus lateralis should be elevated distally from the lateral intermuscular septum for about 10 cm from the ridge. The fascia of the vastus lateralis is incised approximately 1 cm anterior to the attachment of the septum to the linea aspera, and the muscle fibers are swept off the lateral intermuscular septum using a Cobb elevator. Perforator vessels arising from the profunda femoris should be visualized and carefully cauterized to avoid their retraction behind the intermuscular septum causing bleeding in the posterior compartment. Using an oscillating saw, the GT is osteotomized from posterior to anterior starting at the interval between the piriformis tendon medially and the gluteal tendons laterally. The direction of the osteotomy is anteriorly toward the trochanteric tubercle, where part of the gluteus minimus tendon attaches. The trochanteric tubercle can be easily palpated deep to the anterior portion of the gluteus medius fibers. The osteotomy line should exit immediately deep to this tubercle to preserve the gluteus minimus attachment to the osteotomized GT fragment, which also helps to protect the vascular supply to the osteotomy (10).
We prefer the thickness of the osteotomized GT fragment to be approximately 1.5 cm. However, when TSO is performed for a cup revision only in the presence of a proximally porous-coated or a cemented stem, a thinner osteotomy should be planned to leave a bed of bone for reattachment as well as to avoid damaging the fixation of the femoral component. Internal rotation of the hip joint facilitates further access for the osteotomy. The osteotomized GT fragment is translated anteriorly with the continuous sleeve of abductors proximally and vastus lateralis distally. The hip joint is then externally rotated to expose the anterosuperior capsule. The attachment of the vastus intermedius is elevated off the anteromedial surface of the capsule and a generous anterior capsulectomy is performed. The hip joint is dislocated anteriorly using external rotation, adduction, and flexion (Fig. 103.4C).
The posterolateral approach can also be utilized to perform the TSO, which is performed by curvature of the skin and fascial incisions more posteriorly to enhance access and exposure of the posterior structures. The standard posterolateral approach is slightly modified, so that the starting point for the posterior curvature of the skin and fascial incisions
is placed at the anterosuperior angle of the tip of the GT rather than its midpoint. This facilitates the anterior translation of the GT throughout the procedure. With a posterolateral approach, the timing for the TSO can be performed at three different stages of the procedure: (1) prior to hip capsulotomy and dislocation, (2) after dislocation but prior to extraction of stem, and (3) after stem removal. Therefore, one advantage for this approach is that it provides the surgeon with the flexibility to choose the ideal timing for the TSO based on its necessity intraoperatively. Unlike in the lateral approach, to dislocate the hip posteriorly, the attachments of the short external rotators need to be released from the posterior femur. This release is performed by incising the tendons 1 cm medial to their insertion to allow for their repair. Careful repair of the short external rotators and the posterior capsule decreases the rate of posterior dislocation (16,17). The technique for the osteotomy is the same as what was described earlier for the lateral approach. The only difference is that the anterior fibers of gluteus minimus can be left attached anteriorly to the proximal femur since it does not interfere with the exposure of the hip joint.
is placed at the anterosuperior angle of the tip of the GT rather than its midpoint. This facilitates the anterior translation of the GT throughout the procedure. With a posterolateral approach, the timing for the TSO can be performed at three different stages of the procedure: (1) prior to hip capsulotomy and dislocation, (2) after dislocation but prior to extraction of stem, and (3) after stem removal. Therefore, one advantage for this approach is that it provides the surgeon with the flexibility to choose the ideal timing for the TSO based on its necessity intraoperatively. Unlike in the lateral approach, to dislocate the hip posteriorly, the attachments of the short external rotators need to be released from the posterior femur. This release is performed by incising the tendons 1 cm medial to their insertion to allow for their repair. Careful repair of the short external rotators and the posterior capsule decreases the rate of posterior dislocation (16,17). The technique for the osteotomy is the same as what was described earlier for the lateral approach. The only difference is that the anterior fibers of gluteus minimus can be left attached anteriorly to the proximal femur since it does not interfere with the exposure of the hip joint.
As the gluteus medius and minimus muscles are reflected anteriorly, TSO provides excellent exposure of the acetabulum, supra-acetabular area of the iliac wing and the proximal femur. However, access to the anterior part of the iliac wing and pubic rami is not possible due to the limited anterior displacement of the GT that is tethered by the superior gluteal neurovascular bundle. This might be considered a shortcoming of TSO compared to the standard TO, but sufficient acetabular reconstruction is usually possible without complete exposure of the anterior column and wall.
Reattachment of the GT
The hip is internally rotated to facilitate approximation of the GT to its bed. For the posterolateral approach, repair of posterior capsule and short external rotators can be accomplished more easily before reattachment of the GT. In revision situations, the GT can be tethered anteriorly by the scarred gluteus minimus, causing anterior migration of the GT when the hip is externally rotated to neutral. This can be addressed by a limited release of gluteus minimus to the anterior GT fragment. In case of significant lengthening of the limb, subperiosteal release of the gluteal muscles off the iliac wing is gently performed to allow for the advancement and anatomic reattachment of the GT fragment without damaging the superior gluteal neurovascular bundle. If needed, removing a thin layer of bone from the GT or its bed is the next step.
The aforementioned biomechanical data supports the importance of achieving strong initial stability of the GT fragment via solid fixation to the femur to decrease the risk for nonunion and migration of the trochanter. Our preferred
method for repairing the osteotomy is by circumferentially wrapping two or three cerclage 18-gauge double-looped wires around the GT fragment and the calcar (Fig. 103.4D) (18). Although there have been no studies that have compared the clinical results of double-loop wiring to other wiring methods, there is biomechanical evidence to support that the double-looped wiring technique is superior to simple wiring (19). The wires should sit 2 to 3 cm apart to apply compression across the entire osteotomy. After tensioning the wires, we prefer to bury the knot anteriorly on the proximal femoral metaphysis to decrease the rate of GT bursitis. It is important to pass the wires medially distal to the LT to prevent them from loosening and migrating proximally. If the LT is not present, a bone tunnel is created in the calcar for passing the wire through. In case of complete lack of medial bone, we tend to avoid doing a TSO, because there would not be enough bone for union of the osteotomy; in this situation we prefer using an extended trochanteric osteotomy (20).
method for repairing the osteotomy is by circumferentially wrapping two or three cerclage 18-gauge double-looped wires around the GT fragment and the calcar (Fig. 103.4D) (18). Although there have been no studies that have compared the clinical results of double-loop wiring to other wiring methods, there is biomechanical evidence to support that the double-looped wiring technique is superior to simple wiring (19). The wires should sit 2 to 3 cm apart to apply compression across the entire osteotomy. After tensioning the wires, we prefer to bury the knot anteriorly on the proximal femoral metaphysis to decrease the rate of GT bursitis. It is important to pass the wires medially distal to the LT to prevent them from loosening and migrating proximally. If the LT is not present, a bone tunnel is created in the calcar for passing the wire through. In case of complete lack of medial bone, we tend to avoid doing a TSO, because there would not be enough bone for union of the osteotomy; in this situation we prefer using an extended trochanteric osteotomy (20).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree