The Transfemoral Approach to Revision Total Hip Arthroplasty
S. Douglas Werner
Thomas Satterly
William Skakun
David J. Jacofsky
Case Report
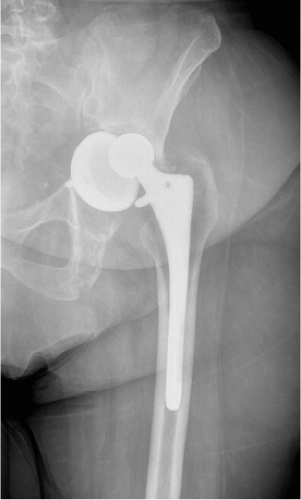
A 74-year-old female with a history of uncemented left THA performed 9 years ago presented with a chief complaint of progressive right groin and thigh pain that had increased over a 2-month period. Initial radiographs demonstrated a THA with significant polyethylene wear and proximal femoral osteolysis with a grossly loose cup and subluxation (Fig. 105.1). The absence of infection was confirmed on preoperative diagnostic evaluation. The patient was indicated for revision with the use of a transfemoral approach to facilitate the procedure.
Introduction
Surgical exposures used in total hip arthroplasty (THA) have gone through many variations in the past. The extended trochanteric osteotomy (ETO) has been one of the keystones to adequate exposure of the hip for a variety of surgical indications. The increasing complexities of surgical hip procedures that are now performed have necessitated techniques to optimize exposure and subsequent component removal. Indications for an ETO include removal of well-fixed components, enhanced exposure, and to accommodate proximal femoral deformities during revision such as varus and retroversion; preparation of the femoral diaphysis for the revision component is also felt to be enhanced with the use of an ETO (1).
The standard ETO procedure was described by Younger et al. in 1995. They utilized a standard posterolateral approach; however, the technique is now used in conjunction with a variety of surgical approaches to the hip. The osteotomy is performed from posterolateral to anterolateral beginning just anterior to linea aspera. The objective is to produce an osteotomy fragment of the lateral 1/3 of the femur with the osteotomy perpendicular to the anteversion of the hip. The anterior cortex is etched so that a greenstick-type fracture can be generated anteriorly when levered from the posterior osteotomy. The distal transverse limb of the osteotomy is made with a pencil-tipped burr to round off the corners and minimize the generation of stress risers (1).
After the placement of a revision component the ETO is repaired with the use of cerclage wires. Typically one cerclage wire is placed 1 to 2 cm distal to the distal extent of the ETO to minimize hoop stresses during implantation of press-fit revision prostheses. To minimize anterior impingement, the osteotomy fragment is initially reduced posteriorly and then sequentially fixated with cerclage wires in a distal to proximal pattern. The distal most wire is typically 2 to 3 cm proximal to the tip of the osteotomy while the proximal most wire is just distal to the vastus ridge. The distal wire may be tightened securely as it will have diaphyseal fixation.
However, the proximal wire is usually tightened the least as this segment of the osteotomy fragment is the most fragile and is the most common site of fracture. Any additional wires are evenly spaced between these two boundary wires.
However, the proximal wire is usually tightened the least as this segment of the osteotomy fragment is the most fragile and is the most common site of fracture. Any additional wires are evenly spaced between these two boundary wires.
Results of the standard ETO have been variable. When performed correctly the standard ETO can provide satisfactory union rates. In 2004, Sporer reported on 122 femoral component revisions that were approached through a standard ETO with an average follow-up with 2.6 years. There was no evidence of nonunion and no proximal migration >2 mm. Twenty-five iatrogenic fractures were identified, all of which were treated with additional cables and strut allograft if bone stock was deemed deficient. The cohort was reevaluated and at an average of 3.9 years of follow-up there were two nonunions and one malunion. All others achieved bony union (2). Although good results are obtainable the procedure is fraught with complications including nonunion rates as high as 15% to 20%, iatrogenic fractures, osteotomy fragment migration, abductor weakness, and lateral hip pain (3,4,5).
In an effort to improve upon the standard ETO, the coronal plane transfemoral modification has been developed. There are multiple similar indications for a transfemoral approach to the femur during hip arthroplasty which include removal of a well-fixed cemented or cementless implant, proximal femoral deformity which may interfere with cement removal or straight reaming of the distal canal, abductor muscle weakness or instability that would benefit trochanteric advancement, or greater trochanteric compromise that would lead to an increased risk of fracture during extraction of the implant (6,7). In addition to femoral exposure, this approach can be used to facilitate acetabular exposure during complex reconstructions such as removal of implants with intrapelvic protrusion or placement of pelvic cages (8).
The standard ETO myo-osseous flap contains the lateral aspect of the proximal femur and encompasses 1/3 of the circumference of the shaft. In the transfemoral approach, the myo-osseous flap is performed in the coronal plane and is ½ of the circumference of the shaft. This can also be performed in the sagittal plane if the goal is to improve proximal femoral varus when a standard ETO does not correct enough of the deformity (3,4,8). The wider flap allows greater access to the implant to be removed and the improved ability to correct proximal femoral deformities (3). When performed in the coronal plane, the transfemoral approach allows access to the medial calcar and metaphyseal bone–implant interface that is often the most well-fixed and challenging portion of revision exposure. Both coronal and sagittal techniques are associated with decreased surgical time, decreased iatrogenic intraoperative femur fractures and cortical perforations, and increased rates of osteotomy union compared to a standard ETO (4,5). The contraindication for a transfemoral approach is the absence of an indication to perform an osteotomy usually because of a femoral implant and/or cement mantle that can be easily removed with a low risk of iatrogenic trochanteric fracture.
Surgical Technique
Preoperative planning for this approach should include radiographs consisting of an anteroposterior (AP) pelvis, and an AP and lateral of the hip to include the most distal aspect of the femoral component and cement mantle, if present. These radiographs are necessary to measure the length of the osteotomy that will be needed for implant removal. The measurement should begin at the tip of the greater trochanter, or a similar femoral landmark that is easy to locate, and continue distally to the tip of the implant for cemented stems. For cementless stems, the measurement should extend 2 to 3 cm distal to the junction of the porous coating if the distal stem is not fully porous or distally ingrown (7). For fully porous-coated stems, it is easier to extend the osteotomy distal to the tip of the stem. The planned osteotomy fragment should be long enough to allow for the placement of at least two cables or wires for fixation. Additional instruments needed for the approach may include an oscillating saw, a Gigli saw, thin flexible osteotomes, a pencil-tipped burr, multiple wide flat osteotomes, Moreland-type cement removal osteotomes, a slap hammer, and cerclage wires or cables that will be needed for fixation of the osteotomy at the end of the procedure. If a stem will be transected to assist with removal, one should also have trephines and a metal cutting burr or diamond cutting wheel available. Cortical strut grafts and claw plates should be available but often are not needed. A longer osteotomy is preferred if it will allow for distal cable fixation instead of a claw plate, as these devices have a high incidence of postoperative bursitis and pain from soft tissue irritation.
A direct lateral approach is utilized (Fig. 105.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree