Chapter 9. The thoracic spine
SUMMARY
This chapter sets out to explain the anatomy of the thoracic spine and highlights the somatic structures which are a common cause of pain. Pain patterns are discussed and the non-mechanical causes of thoracic back pain are presented to aid diagnosis and appropriate management.
The clinical examination procedure is outlined and interpreted, the contraindications are emphasized and the treatments used in orthopaedic medicine are described, with notes on the indications for their use.
ANATOMY
There are 12 thoracic vertebrae which gradually increase in size from above down, marking a transition between cervical and lumbar vertebrae. A typical thoracic vertebra is easily recognized by its costal facets, its heart-shaped superior surface and waisted vertebral body (Fig. 9.1). The vertebral canal in the thoracic region is round and smaller than that found in either the cervical or lumbar spine. Short pedicles pass almost directly backwards and thick, broad laminae overlap each other from above down.
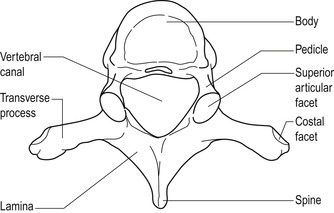 |
| Figure 9.1 Typical thoracic vertebra. From Anatomy and Human Movement by Palastanga N, Field D and Soames R. Reprinted by permission of Elsevier Ltd. |
The slope of the long spinous processes gradually increases downwards with the 5th to 8th spinous processes overlapping each other. The 8th spinous process is the longest, while the 12th is shorter, horizontal and similar to the lumbar spinous processes.
Long, rounded, club-like transverse processes are directed posterolaterally and slightly superiorly. Except for the 11th and 12th vertebrae, oval, anterior facets lie at the tips of all transverse processes. These facets articulate with the tubercles of the corresponding ribs.
Flat articular processes project superiorly and inferiorly to form the thoracic zygapophyseal joints. Their direction facilitates the movement of rotation, which is coupled with side flexion, while also permitting a range of flexion and extension. Rotation is a particular feature of the thoracic spine and is facilitated by the direction of the articular facets and rotation of the fibres in the intervertebral discs. The shearing movement common to lumbar discs does not occur so readily in the thoracic spine (Kapandji 1974). The 12th thoracic vertebra is a transitional vertebra with the upper surface being typical of a thoracic vertebra but the lower surface having lumbar characteristics for articulation with L1. A dramatic change of direction of the plane of the zygapophyseal joints occurs over one level at the thoracolumbar junction permitting rotational stresses between T11 and T12 which are disallowed between T12 and L1. This makes the 12th thoracic vertebra susceptible to fracture (Agur & Dalley 2009).
The thoracic intervertebral joints consist of the vertebral body above and below and the intervertebral disc. These joints are supported by anterior and posterior longitudinal ligaments, supraspinous, interspinous and intertransverse ligaments and the ligamentum flavum that connects adjacent laminae internally. Further support is gained by the costovertebral joints and ligaments which directly involve the intervertebral disc.
Nakayama et al (1990), Maiman & Pintar (1992), Oppenheim et al (1993), Bogduk & Valencia (1994) and Boriani et al (1994) all share the opinion that disc lesions are relatively uncommon in the thoracic spine, in contrast to the claim that disc lesions account for a higher proportion of thoracic pain than is often realized (Cyriax & Cyriax 1993, Mellion & Ladeira 2001). The bony anatomy, including the primary kyphotic curve, and the surrounding ligamentous structures related to the costovertebral joints may have a stabilizing effect on the intervertebral disc, making displacement less likely in this region. The rib cage also exerts a stabilizing effect by restricting movement, particularly in the upper segment where the ribs are firmly attached anteriorly and posteriorly.
Movement in the thoracic spine is limited. This is due in part to the thoracic disc height relative to vertebral body height being less than in the cervical or lumbar spines with the ratio of disc diameter to height 2–3 times greater than in the lumbar spine. The acute angle of orientation of the annular fibres and the relatively small nucleus in the thoracic spine contribute to this lack of mobility. The angle of the zygapophyseal joints in the thoracic spine facilitates rotation while limiting flexion and anterior translation and having little influence on side flexion (Edmondston & Singer 1997). Little has been written about the structure and function of the thoracic disc, so it is not covered in depth here.
Twelve pairs of ribs normally attach posteriorly to the thoracic spine. The upper seven pairs are termed true ribs and attach anteriorly to the sternum. The lower five pairs consist of false and floating ribs, the false ribs attaching to the costal cartilage above.
A typical rib consists of a shaft and anterior and posterior ends. It is the posterior end that concerns us here. The posterior end of the rib typically has a head, neck and tubercle and articulates with the thoracic vertebrae, forming the posterior rib joints. The head of the rib is divided into two demifacets by a horizontal ridge that is attached to the disc via an intra-articular ligament. The lower facet articulates with its corresponding vertebra; the upper facet articulates with the vertebra above.
The tubercle of the rib is at the junction of the neck with the shaft and articulates with the transverse process of the corresponding vertebra. Just lateral to the tubercle the rib turns to run inferiorly forwards; this point is the angle of the rib.
A cervical rib may be present as an extension of the costal elements of the seventh cervical vertebra. It generally passes forwards and laterally into the posterior triangle of the neck where it is crossed by the lower trunk of the brachial plexus and the subclavian vessels. Compression of these structures may produce motor and sensory signs and symptoms.
Posterior rib joints
Two joints, the costovertebral and costotransverse joints, attach the rib firmly to the vertebral column (Fig. 9.2). These assist stabilization of the intervertebral joint while being relatively unstable themselves. Minor subluxations of these joints may be responsible for the mechanical pattern of signs and symptoms associated with a thoracic pain. This minor instability may also account for the ease with which subluxations occur and can be reduced in this region.
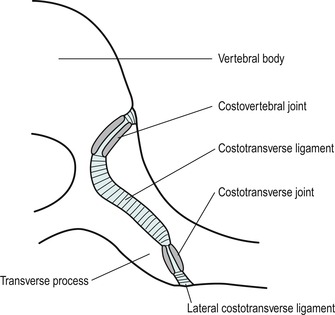 |
| Figure 9.2 Posterior rib joints. Costovertebral and costotransverse joints, horizontal section. From Anatomy and Human Movement by Palastanga N, Field D and Soames R. Reprinted by permission of Elsevier Ltd. |
The costovertebral joint is a synovial joint formed between the head of the rib and two adjacent vertebral bodies, except at the first, 11th and 12th ribs, where a joint is formed with a single vertebral body. The joint surfaces are covered by articular cartilage and surrounded by a fibrous capsule. The capsule is thickened anteriorly by the radiate ligament while the posterior aspect of the capsule blends with the nearby denticulation of the posterior longitudinal ligament. An intra-articular ligament divides the joint and attaches the transverse ridge of the rib head to the intervertebral disc.
The costotransverse joint joins the upper 10 ribs to the transverse processes of their corresponding vertebra. The joint is surrounded by a fibrous capsule that is reinforced posteriorly by the lateral costotransverse ligament. The joint is further stabilized by the costotransverse ligament which joins the transverse process to the neck of the rib, and the superior costotransverse ligament which connects the rib to the transverse process of the vertebra above. Movements occur concurrently at the costovertebral and costotransverse joints and are determined by the shape and direction of the articular facets. This amounts to small rotary and gliding movements in association with the ‘bucket handle’ action of the ribs during respiration.
Three thin musculotendinous layers occupy the intercostal space between adjacent ribs and may become symptomatic due to strain (Fig. 9.3). The external intercostal muscle is the most superficial, with fibres running in an oblique direction downwards and forwards. The internal intercostal muscle lies beneath with fibres running in the opposite direction, and the thinnest and deepest layer is formed by the innermost (intimi) intercostal muscle, which is thin and possibly absent, with fibres running in the same direction as the internal intercostal muscle.
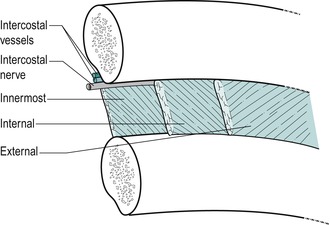 |
| Figure 9.3 Layers of intercostal muscles. From Anatomy and Human Movement by Palastanga N, Field D and Soames R. Reprinted by permission of Elsevier Ltd. |
Differential diagnosis at the thoracic spine
Orthopaedic medicine treatment techniques for the thoracic spine are aimed at reducing a mechanical lesion, i.e. subluxation of a posterior rib joint or herniations of the intervertebral disc.
Minor subluxation of the posterior rib joints
Subluxation of one or other of the posterior rib joints is a common cause of thoracic pain. The articulating surfaces of these joints are relatively shallow and unstable, rendering them susceptible to minor subluxations. The relatively trivial incidents that provoke thoracic mechanical pain and the relative ease with which it is reduced leads us to this hypothesis. Differential diagnosis of thoracic pain is difficult because of the numerous conditions that refer pain to the area and the lesions that mimic mechanical pain.
Patients present with a sudden onset of pain; the precipitating event is usually trivial and they often feel a pop or click. More gradual onset can be associated with working in rotated postures. The pain presents a typical mechanical picture of pain aggravated by movement and posture and eased by rest. In common with a thoracic disc lesion, a deep breath often provokes the pain, presumably because the ‘bucket handle’ action of the ribs during respiration translates aggravating movements to the rib joints at the spine.
On examination there is a non-capsular pattern of limited movement involving one rotation more than the other and these simple mechanical lesions usually respond rapidly to manipulation. Provided that there are no contraindications present (see below), the manipulative techniques described in this chapter can be applied. The usual postural and management advice should also be given to prevent recurrence, which is also a typical feature.
Thoracic disc lesions
It is important to reduce a thoracic disc displacement because of the potential for the displaced fragment to compromise the spinal cord. The thoracic vertebral canal is relatively small; therefore central prolapse poses the most threat.
In a review of the literature, Oppenheim et al (1993) reported an estimated annual incidence of one case of thoracic disc herniation per 1 million population. However, Mellion & Ladeira (2001) present a more current review of the literature which suggests that thoracic disc herniations are more common than previously thought and that in many cases these may be asymptomatic. It is primarily a condition of middle age, occurring between the third and fifth decade, and affects the lower thoracic levels more frequently. This is probably because the lower thoracic spine is free of the restriction of the rib cage, making it more mobile, and the transition to the non-rotational lumbar spine produces greater torsional stresses here. The most common level reported was T11, 12, and 75% of thoracic disc lesions occurred below T8.
Positive diagnosis of a thoracic disc lesion is difficult. There is no regular pattern to the history, signs and symptoms, as found at the cervical and lumbar spine, and it is not possible to produce a clinical model on which to base differential diagnosis. Wilke et al (2000) reported a case of shoulder pain associated with a lower thoracic disc herniation.
Central disc prolapse is most likely to compress the spinal cord and produce signs of myelopathy which include progressive paraparesis, increased reflexes, decreased sensation and bladder dysfunction. Although thoracic disc herniations are rare, Ozturk et al (2006) highlight the potential danger of their being missed as they could possibly result in the progressive myelopathy and paralysis mentioned above. A posterolateral prolapse produces segmental signs and symptoms.
To support the possible confusion arising from thoracic referred pain, Ozturk et al (2006) presented a case study of a patient with left flank pain, compatible with urinary system disorder. The cause of the pain could not be identified until magnetic resonance imaging (MRI) revealed a left T10–T11 lateral disc herniation with associated nerve root compression. They warn that thoracic disc herniation should be considered in the differential diagnosis of patients with pain more likely to be associated with visceral disorders, especially if basic diagnostic studies do not reveal the cause.
A further example is provided by Whitcomb et al (1995) who describe a patient with a 7-year history of severe disabling chronic epigastric abdominal pain attributed to chronic pancreatitis for which a 95% pancreatectomy was performed for pain control. Previous attempts to identify and treat the pain led to extensive radiographic, pharmacological, endoscopic and surgical interventions. Pain control was poor despite implantation of a continuous intrathecal morphine infusion pump. A focused physical examination eventually raised the suspicion of thoracic disc disease, which was confirmed with computed tomography. Disruption of the T7–T8 disc with protrusion into the vertebral canal and displacement of the spinal cord was identified. A microsurgicaI thoracic discectomy was performed and immediately the pain began resolving with the patient being pain-free and off all medication within several weeks.
In a review of the literature, Mellion & Ladeira (2001) highlight degenerative change, traumatic incidents, lifting, rotation, falls, exercise, rugby tackles and road traffic accidents as precipitating factors for thoracic disc lesions. The onset may be sudden and severe or insidious and slowly progressive. Mellion & Ladeira mention that Cyriax was the first author to describe the clinical presentation of a thoracic disc lesion. They suggest it may give four classical presentations: intermittent thoracic back pain which may be aggravated by sitting and relieved by standing; acute thoracic ‘lumbago’ with the thoracic spine fixed in flexion following a bending or twisting motion; thoracic root pain and paraesthesia; and symptoms of spinal cord compression. Chest pain may be constant or intermittent and may be central, localized or diffuse. A band-like dermatomal chest pain is not uncommon and abdominal referral may occur. If accompanied by cord compression, complaints of bladder involvement, lower limb paraesthesia and gait disturbance can be reported and findings may include spastic muscle weakness, hyperreflexia and a positive Babinski sign.
Mellion & Ladeira (2001) suggest that upper thoracic disc lesions are less common. Radiculopathies involving T1 share similarities with those occurring at C8, with numbness and weakness in the hand and pain in the arm and medial forearm. Weakness of the intrinsic hand muscles may be involved with T1, but this is an uncommon finding and the clinician must exclude non-mechanical causes such as Pancoast’s tumour. Horner’s syndrome (miosis and ptosis of the eye) is associated with T1 involvement but not C8. Presence of Horner’s syndrome is therefore contraindicated in manipulation or mobilization of the thoracic joints until the cause of the symptoms has been determined.
Disc lesions at the T2 and 3 levels are even less common and there are few reports in the literature of the features of involvement of T3–T8; symptoms of nerve root involvement at these levels may produce intercostal neuralgia. If there is involvement of the dura mater or dural nerve root sleeve, their mobility will be impaired and signs provoked on flexion of the cervical spine and scapular approximation. T9–T11 may produce a dermatomal pattern of pain and can include the abdomen and groin, often being confused with visceral symptoms. These lower levels may also mimic lumbar presentations including low back and leg pain.
In summary, small uncomplicated thoracic disc lesions may present with sudden or gradual onset of pain that may be felt posteriorly, anteriorly or radiating laterally. Pressure on the dura mater produces multisegmental reference of pain. The pain should have a typical mechanical behaviour, i.e. aggravated by movement and posture and eased by rest. Dural symptoms of increased pain on a cough, sneeze or deep breath may be present.
On examination, a non-capsular pattern of limited movement will be found, with one rotation being significantly more painful or limited than the other. Dural signs of pain on neck flexion and/or scapular approximation may be present if the dura mater is compromised. If there are no neurological signs and signs of cord compression are absent, the treatment techniques described in this chapter may be used. Alternatively, since lower thoracic displacements are more common, they may be treated using the techniques described for the lumbar spine.
Urgent surgical intervention is necessary for patients showing signs of spinal cord compression. Otherwise, uncomplicated thoracic disc lesions follow a path of recovery similar to that seen in cervical and lumbar disc lesions, responding to physical treatments and eventually stabilizing with time (Brown et al 1992).
Other causes of thoracic pain and associated signs and symptoms
Cervical disc lesions commonly refer pain into the thoracic region and this is particularly indicative of dural reference producing unilateral or bilateral scapular pain. The patient has a typical mechanical picture, with cervical movements increasing the pain felt in the thoracic region. Pain is not reproduced by thoracic movements. Minor chest wall pain may frequently be recognized as referred from the cervical spine, and Yeung & Hagen (1993) reported two cases of herniated C6–C7 disc producing major neuropathic chest wall pain which were treated surgically.
Subluxations of the posterior rib joints are a common cause of thoracic pain. They tend to present with unilateral central pain and tenderness and a non-capsular pattern of pain and limitation of movement. They respond quickly to the manipulative techniques described below.
Arthritis presents with the capsular pattern of limited movement.
• Equal limitation of rotations.
• Equal limitation of side flexions.
• Some limitation of extension.
• Usually full flexion.
• Degenerative osteoarthrosis can affect the spinal joints, causing secondary signs and symptoms. Gross degenerative changes may produce central osteophytes that may cause gradual cord compression. Anterior and lateral lipping of the vertebral body, as well as wedging of mid-thoracic vertebrae, has been associated with degenerative osteoarthrosis of the thoracic spine (Osman et al 1994).
• Inflammatory arthritis can involve the thoracic spine. Rheumatoid arthritis commonly affects the costovertebral, costotransverse and zygapophyseal joints. Reiter’s disease can affect the spinal joints, although it is more frequently seen in the lower limb joints. Ankylosing spondylitis, when it involves the thoracic cage, causes a reduction in chest expansion. Thoracic pain and stiffness may be its presenting symptoms.
Serious non-mechanical conditions can affect the thoracic area and suspicions are alerted when the patient appears unwell, has a fever, night pain with or without night sweats, or reports an unexpected weight loss. The pain is not affected by movement or postures and is often unrelenting.
• Malignant disease, both primary and secondary, may be a cause of pain in the thoracic spine. Bronchial carcinoma accounts for 95% of all primary tumours of the lung and may present with a cough and chest pain (Kumar & Clark 2002). Tumours in the bronchus, breast, kidney, prostate and thyroid commonly metastasize to bone. Intradural and extradural neoplasm, although relatively rare, may produce symptoms similar to nerve root irritation. Watanabe et al (1992) reported a case of benign osteoblastoma in the sixth thoracic vertebra presenting with thoracodorsal pain in a 19-year-old woman, increased by coughing and shifting sleeping positions. Hodges et al (1994) reported a case of intraspinal, extradural synovial cyst at the level of T4–T5 in a 51-year-old woman experiencing intermittent mid-thoracic and lumbar pain after lifting.
• Spinal infections may include osteomyelitis or epidural abscess. The organism responsible may be Staphylococcus aureus, Mycobacterium tuberculosis or, rarely, Brucella (Kumar & Clark 2002).
Bone conditions can include acquired conditions or congenital abnormalities. These conditions may be asymptomatic and a chance finding on X-ray.
• Scheuermann’s disease is vertebral osteochondritis, most commonly seen in males aged 12–18 years. It usually involves the lower thoracic vertebrae, often T9. The disc may move forwards between the cartilage end-plate and the anterior longitudinal ligament, producing wedging. It may produce minor thoracic backache and a local dorsal kyphosis may be evident on spinal flexion (Corrigan & Maitland 1989). Scheuermann’s disease has been associated with Schmorl’s nodes and degenerative lumbar disc disease in relatively young patients (Heithoff et al 1994).
• Schmorl’s nodes are protrusions of the intervertebral disc into the cancellous bone of the vertebral body. This may produce an anterior prolapse, causing separation of a small fragment of bone, seen on X-ray as a limbus vertebra (Taylor & Twomey 1985).
• Osteoporosis is a reduction in bone mass that may present a problem in postmenopausal women, who lose bone density faster than men. It is common in the sixth and seventh decades of life. Pain is not due to the condition itself, but usually to secondary wedge compression fractures of the vertebral body (Turner 1991). The patient presents with moderate to severe episodes of thoracic back pain that gradually resolve over the course of approximately 6 weeks. Fracture produces wedging of the vertebral body on X-ray and a characteristic increase in thoracic kyphosis is seen.









