7 The Stomach The esophagus is located in the posterior mediastinum. It lies medial in front of the spinal column until the tracheal bifurcation (T4), after which it moves to the right side, to make room for the heart. Lastly, it crosses the diaphragm to the left of the median line. At the level of T7–T8, the aorta squeezes in between the spinal column and the esophagus. The abdominal part is only about 2 cm long. The esophagus remains mobile in the lengthwise direction. These nodes all drain into the right/thoracic lymphatic duct. Division into:
Anatomy
 Anatomy of the Esophagus
Anatomy of the Esophagus
Location
Topographic Relationships
Thorax
 trachea
trachea
 left main bronchus
left main bronchus
 mediastinal pleura
mediastinal pleura
 pericardium
pericardium
 spinal column
spinal column
 aorta
aorta
 right lung (in the area of the esophageal hiatus)
right lung (in the area of the esophageal hiatus)
 vagus nerve, right and left
vagus nerve, right and left
Abdomen
 peritoneum in the front
peritoneum in the front
 liver
liver
 crus to the left of the diaphragm
crus to the left of the diaphragm
 left side: left triangular ligament
left side: left triangular ligament
 right side: lesser omentum
right side: lesser omentum
 T10 and T11
T10 and T11
Attachments/Suspensions
 organ pressure
organ pressure
 turgor
turgor
 mediastinal connective tissue
mediastinal connective tissue
 phrenoesophageal ligament (ring-shaped disk in the hiatus).
phrenoesophageal ligament (ring-shaped disk in the hiatus).
Circulation
Cervical
 inferior thyroid artery
inferior thyroid artery
 small branches from the subclavian/communal carotid/vertebral arteries, etc.
small branches from the subclavian/communal carotid/vertebral arteries, etc.
 inferior thyroid vein (from the superior vena cava)
inferior thyroid vein (from the superior vena cava)
Thoracic
 bronchial arteries
bronchial arteries
 aorta
aorta
 azygos/hemiazygos/accessory hemiazygos vein (from the superior vena cava)
azygos/hemiazygos/accessory hemiazygos vein (from the superior vena cava)
Abdominal
 left gastric artery
left gastric artery
 inferior phrenic artery
inferior phrenic artery
 celiac trunk
celiac trunk
 left gastric vein (main drainage) to the portal vein
left gastric vein (main drainage) to the portal vein
Lymph Drainage
 deep cervical cord (internal jugular vein–parotid gland–clavicle)
deep cervical cord (internal jugular vein–parotid gland–clavicle)
 intercostal, thoracic nodes near the spinal column
intercostal, thoracic nodes near the spinal column
 paratracheal nodes along the recurrent laryngeal nerve
paratracheal nodes along the recurrent laryngeal nerve
 tracheobronchial nodes
tracheobronchial nodes
 nodes around the celiac trunk (cisterna chili—thoracic duct)
nodes around the celiac trunk (cisterna chili—thoracic duct)
Innervation
 sympathetic nervous system from T4 to T6
sympathetic nervous system from T4 to T6
 further path of sympathetic innervation: pharyngeal plexus–superior cervical/stellate ganglion–greater splanchnic nerve–celiac plexus
further path of sympathetic innervation: pharyngeal plexus–superior cervical/stellate ganglion–greater splanchnic nerve–celiac plexus
 vagus nerves accompany the esophagus into the abdomen
vagus nerves accompany the esophagus into the abdomen
 Anatomy of the Stomach
Anatomy of the Stomach
Location
 cardia (stomach entrance)
cardia (stomach entrance)
 fundus (cranial region, filled with air)
fundus (cranial region, filled with air)
 body
body
 antrum
antrum
 pylorus
pylorus
 greater curvature
greater curvature
 lesser curvature
lesser curvature
| Structure | Projects to |
| Greater tuberosity | Fifth ICS on the left |
| Front of cardia | Left seventh costochondral joint |
| Back of cardia | T11 on the left costovertebral joint |
| Lesser curvature | Below the cardia at the level of the seventh costochondral joint on the left parallel to the spinal column up to L1 (T10–L1) |
| Pylorus | When standing about L3, when lying down L1–L2 |
ICS, intercostal space.
Cardia and pylorus are relatively fixed points; in between, great variability is possible depending on the state of fullness.
Topographic Relationships
 diaphragm
diaphragm
 indirect: pleura and left lung, pericardium and heart
indirect: pleura and left lung, pericardium and heart
 ribs 5–8 and costal cartilage 9 on the left
ribs 5–8 and costal cartilage 9 on the left
 liver
liver
 celiac trunk and plexus
celiac trunk and plexus
 omental bursa
omental bursa
 left crus of the diaphragm
left crus of the diaphragm
 left adrenal gland
left adrenal gland
 left kidney
left kidney
 pancreas
pancreas
 transverse colon
transverse colon
 transverse mesocolon
transverse mesocolon
 left colic flexure
left colic flexure
 duodenum (horizontal and ascending part)
duodenum (horizontal and ascending part)
 duodenojejunal flexure and start of the jejunum
duodenojejunal flexure and start of the jejunum
 spleen
spleen
Attachments/Suspensions
 organ pressure
organ pressure
 turgor
turgor
 gastrophrenic ligament
gastrophrenic ligament
 lesser omentum
lesser omentum
 greater omentum
greater omentum
 gastrocolic ligament
gastrocolic ligament
 gastrolienal ligament
gastrolienal ligament
 left phrenicocolic ligament
left phrenicocolic ligament
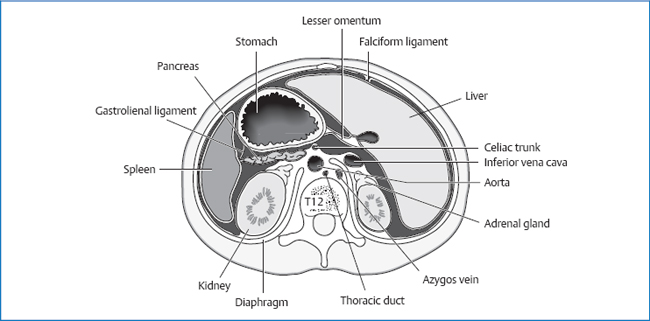
Fig. 7.1 Upper abdominal organs, transverse section.
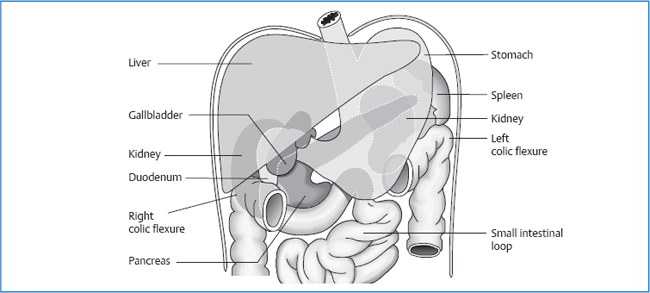
Fig. 7.2 Topographic relationships of the stomach.
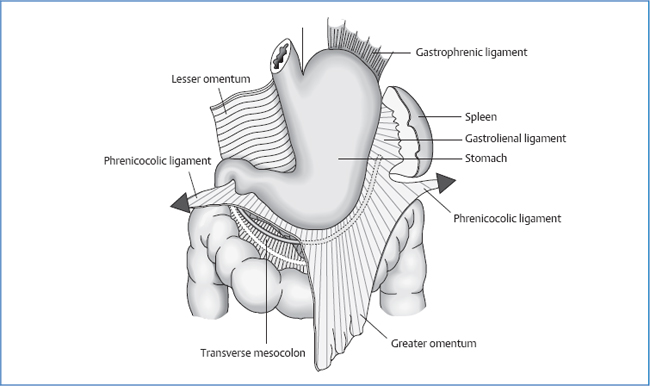
Fig. 7.3 Attachments of the stomach.
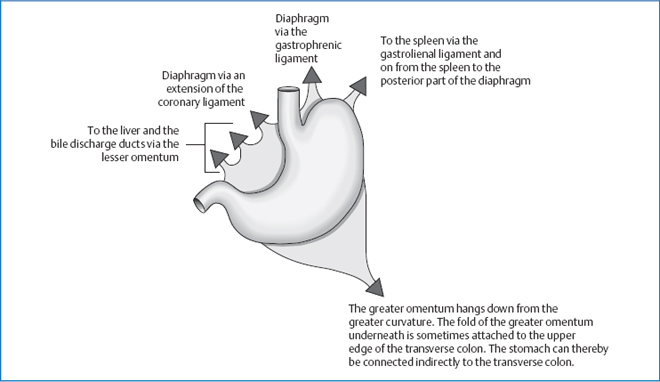
Fig. 7.4 Attachments of the stomach, schematic.
Circulation
Arterial
 right gastric artery (from proper hepatic artery)
right gastric artery (from proper hepatic artery)
 left gastric artery (from celiac trunk, anastomosed with the right gastric artery)
left gastric artery (from celiac trunk, anastomosed with the right gastric artery)
 right gastro-omental artery (gastroduodenal artery)
right gastro-omental artery (gastroduodenal artery)
 left gastro-omental artery (splenic artery—celiac trunk)
left gastro-omental artery (splenic artery—celiac trunk)
 gastroduodenal artery (common hepatic artery—celiac trunk)
gastroduodenal artery (common hepatic artery—celiac trunk)
Venous
Portal vein.
Lymph Drainage
 paracardial lymph nodes
paracardial lymph nodes
 pancreatic lymph nodes
pancreatic lymph nodes
 splenic nodes
splenic nodes
 celiac nodes—thoracic duct (main drainage)
celiac nodes—thoracic duct (main drainage)
Innervation
 sympathetic nervous system from T6 to T9 via the greater and lesser splanchnic nerves
sympathetic nervous system from T6 to T9 via the greater and lesser splanchnic nerves
 further path of sympathetic innervation runs to the celiac and superior mesenteric ganglion
further path of sympathetic innervation runs to the celiac and superior mesenteric ganglion
 vagus nerve
vagus nerve
Organ Clock
Maximal time: 7–9a.m.
Minimal time: 7–9p.m.
Organ–Tooth Interrelationship
For basic information, see page 34.
- Second premolar in the lower jaw on both sides
- Second molar in the upper jaw on both sides
Movement Physiology according to Barral
Mobility
The esophagus has lengthwise mobility. During movements of the head and neck, it must be able to adjust its length.
To transport food, peristaltic waves run through the esophagus during the act of swallowing.
The stomach shows mobility in three planes: frontal, sagittal, and transverse.
Frontal Plane
During inhalation, the diaphragm guides the lateral parts of the fundus of the stomach inferomedially. The distance between the lesser and greater curvature decreases, as does the distance between the fundus and antrum. Looked at from the front, the stomach rotates in a clockwise direction.
Sagittal Plane
In this plane, the stomach performs a tilt with the cranial parts of the fundus in an anterior direction, accompanied by a simultaneous shift posteriorly in the antral area. The frontotransverse axis of movement runs roughly through the center of the stomach.
Transverse Plane
The stomach performs a rightward rotation along a frontosagittal axis through the inferior part of the esophagus.
Motility
The motions of motility correspond in direction and axis to those of mobility.
Physiology
Proximal and Distal Stomach
The relief structure of the stomach wall serves as a “slide” for the chyme in the direction of the pylorus. The proximal stomach acts as food storage and is marked by continuous tension in the walls.
The distal stomach has the task of mixing, homogenizing, and emulsifying the food. For this purpose, peristaltic waves run from a central pacemaker through the distal stomach. A distension in the stomach stimulates these waves; a distension in the small intestine inhibits the activity of the distal stomach (enterogastric reflex).
The pylorus does not close so tightly that fluids are unable to pass. It relaxes synchronously with each contractile wave of the distal stomach, but only far enough that small food particles can still pass while the large parts are thrown back.
Main Functions of the Stomach
 grinding up solid food, emulsification of fats, predigestion of proteins
grinding up solid food, emulsification of fats, predigestion of proteins
 secretion of gastric juice
secretion of gastric juice
Gastric Juice
Mucus
Mucus is secreted by the epithelial cells on the surface of the stomach, the side cells of the fundic glands, and the cardiac and pyloric glands.
Bicarbonate
Bicarbonate is secreted by the epithelial cells in the stomach mucosa.
Both components of gastric juice serve to protect the stomach walls from hydrochloric acid (HCl). An H+ gradient exists across the mucosa, from strongly acid on the lumen side to slightly alkaline on the epithelium side (effect of bicarbonate).
Pepsinogen
Pepsinogen is secreted by the chief cells of the fundic and body glands. At a pH < 3, it is activated into pepsin and cleaves proteins.
Hydrochloric Acid
Hydrochloric acid is secreted by the parietal cells in the fundic glands.
Intrinsic Factor
The intrinsic factor is necessary for the absorption of vitamin B12 in the small intestine.
Regulating the Secretion of Gastric Juice
The secretion of gastric juice has several trigger mechanisms.
Cephalic Phase
The secretion of gastric juice is stimulated via the vagus nerve by smell, taste, and glucose deficiency in the brain.
Gastric Phase
Distension of the stomach, amino acids (especially tryptophan and phenylalanine), and Ca2+ ions increase the secretion of gastric juice.
Intestinal Phase
This is stimulation by the voiding of chyme into the duodenum. The secretion of gastric juice is inhibited by a strongly acid pH balance in the stomach which inhibits the release of gastrin; this, in turn, inhibits the secretion of HCl in the parietal cells.
Hormones
Gastrin
Gastrin is secreted by the antral glands (two-thirds) and the duodenal mucosa (one-third).
Release Stimulation
 presence of peptides or certain amino acids
presence of peptides or certain amino acids
 vagal efferents
vagal efferents
 high catecholamine concentration in the plasma
high catecholamine concentration in the plasma
Release Inhibition
The pH of gastric juice is < 3.
Functions
 stimulates HCl secretion in the parietal cells
stimulates HCl secretion in the parietal cells
 increases strength and frequency of antral peristalsis
increases strength and frequency of antral peristalsis
 promotes epithelial growth in the stomach and duodenum
promotes epithelial growth in the stomach and duodenum
 stimulates the pancreatic acini, bile secretion, and gallbladder contraction
stimulates the pancreatic acini, bile secretion, and gallbladder contraction
Cholecystokinin
Cholecystokinin (CCK) is secreted in the duodenal and jejunal epithelia.
Release Stimulation
Presence of free fatty acids, peptides, aromatic amino acids, or glucose in the duodenal lumen.
Release Inhibition
Trypsin in the intestinal lumen (protein-cleaving enzyme from the pancreas).
Functions
 stimulates the acinar cells of the pancreas (neutral chloride-rich juice with proenzymes)
stimulates the acinar cells of the pancreas (neutral chloride-rich juice with proenzymes)
 stimulates the secretion of alkaline pancreatic juice rich in bicarbonate
stimulates the secretion of alkaline pancreatic juice rich in bicarbonate
 releases all pancreatic hormones
releases all pancreatic hormones
 promotes pancreatic growth
promotes pancreatic growth
 stimulates the chief cells of the stomach (⇒ pepsinogen ↑)
stimulates the chief cells of the stomach (⇒ pepsinogen ↑)
 inhibits HCl secretion
inhibits HCl secretion
 strong stimulator of gallbladder contraction, opens the sphincter of Oddi
strong stimulator of gallbladder contraction, opens the sphincter of Oddi
 satiety hormone
satiety hormone
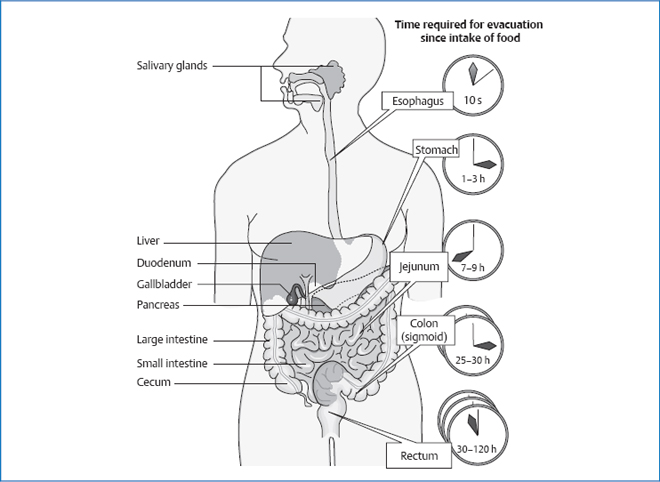
Fig. 7.5 Voiding times from ingestion.
Secretin
Secretin is secreted in the duodenal and jejunal epithelium.
Release Stimulation
Acid chyme.
Functions
 stimulates the secretion of alkaline pancreatic juice rich in bicarbonate
stimulates the secretion of alkaline pancreatic juice rich in bicarbonate
 alkalizes the bile in the bile duct system
alkalizes the bile in the bile duct system
 inhibits the resorption of water and salt in the gallbladder
inhibits the resorption of water and salt in the gallbladder
 slows down the emptying of the stomach by inhibiting the stomach muscles
slows down the emptying of the stomach by inhibiting the stomach muscles
 antitrophic effect on the gastric mucosa
antitrophic effect on the gastric mucosa
Pathologies
 Symptoms that Require Medical Clarification
Symptoms that Require Medical Clarification
Hiatus Hernia
Definition
Prolapse of parts of the stomach or of the entire stomach (possibly even of other organs) through the esophageal hiatus into the thorax.
Forms
Sliding Hernia
Movement of the cardia and fundus into the rear mediastinum, with the pointed angle of His being lifted.
Frequently asymptomatic. About 25% of patients develop reflux symptoms; reflux esophagitis is possible (5% of cases).
Paraesophageal Hernia or Rolling Hernia
Protrusion of parts of the fundus into the thorax (past the esophagus and the cardia, which is fixed in its normal location), with a pointed angle of His.
The sphincter continues functioning and reflux is unlikely to occur. Cardinal symptoms are pain in the epigastrium and iron deficiency anemia.
Hybrid forms between the two are possible.
Functional Hernia according to Barral
In cases with similar symptoms, the radiological signs of a hiatus hernia are absent. Such conditions can be caused by a spasm in the gastroesophageal transition or nonphysiologic tissue pulls in the peritoneum, ligaments, or fascia.
Prerequisites for a Healthy Sphincter Function according to Barral
 physiologic pressure conditions in the abdomen and thorax
physiologic pressure conditions in the abdomen and thorax
 causes for pathologic changes: pregnancy, cough, obstipation with impaired defecation
causes for pathologic changes: pregnancy, cough, obstipation with impaired defecation
 soft anatomic surroundings that are free from nonphysiologic tissue pulls
soft anatomic surroundings that are free from nonphysiologic tissue pulls
 causes for pathologic changes: surgery or effects of inflammation
causes for pathologic changes: surgery or effects of inflammation
 physiologic lengthwise tension in the esophagus
physiologic lengthwise tension in the esophagus
 causes for pathologic changes: kyphotic posture or inflammation
causes for pathologic changes: kyphotic posture or inflammation
 functional diaphragm tension and position
functional diaphragm tension and position
 for healthy sphincter function, the angle of His must be pointed
for healthy sphincter function, the angle of His must be pointed
 normotonic muscle tension at the gastroesophageal transition
normotonic muscle tension at the gastroesophageal transition
Clinical. Roughly 95% of all reflux patients have a hiatus hernia; by contrast, only about 5% of patients with hiatus hernia have reflux disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




