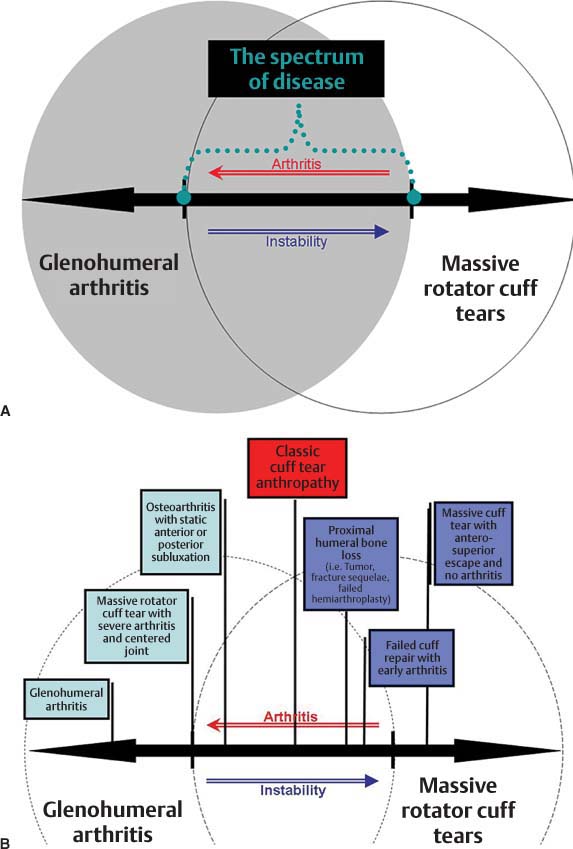
6 The Spectrum of Disease in the Rotator Cuff–Deficient Shoulder The understanding of the relationship between the rotator cuff (RC) deficient shoulder and glenohumeral arthritis continues to evolve. Early attempts at defining this pathology resulted in a variety of nomenclature used to describe a similar clinical presentation: Milwaukee shoulder, l’épaule sénile hémorragique (the hemorrhagic shoulder of the elderly), cuff tear arthropathy (CTA), apatite-associated destructive arthritis, and so on. These clinical descriptions were focused on disease characteristics that typify what has become known as CTA: severe glenohumeral arthritis with joint collapse, a hemorrhagic-crystalline effusion, and a massive RC tear. Classic CTA actually represents one of several disease processes that can be present in the rotator cuff deficient shoulder. In fact, a spectrum of disease exists for the RC-deficient shoulder (Fig. 6–1). Classic CTA, as originally described by Neer and colleagues,1 represents the patient with a massive RC tear with severe glenohumeral arthritis that advances with collapse of the articular surface. However, several other manifestations within the spectrum of the RC-deficient shoulder may result in a similar loss of function (Table 6–1). These include instability due to massive RC tears, RC tears with minimal arthritis, RC deficiency with anterior superior escape, and a variety of conditions that result in proximal humeral bone loss and subsequent RC deficiency (i.e., nonunion of greater tuberosity or tumor resection). My goal in this chapter is to first review the established knowledge on the disease. I will then focus on utilizing my group’s experience in managing this population of patients to establish key principles necessary to understand the pathology, pathophysiology, and treatment of the RC-deficient shoulder. By clearly defining the pathology present, one can begin to understand how aspects of the pathology contribute to the pathophysiology of the disease. This introduction will serve as a foundation for other chapters, as these principals are paramount in the diagnosis and management of the RC-deficient shoulder. Although Neer et al1 first coined the term cuff tear arthropathy, the description of such pathology was reported previously. In the 19th century, Adams and Smith described a patient with a localized form of rheumatoid arthritis involving the shoulder.2–5 In 1934, Codman reported a patient with a subacromial space hygroma who had recurrent swelling, RC deficiency, severe glenohumeral arthritis, and cartilaginous bodies of the synovium.3 In 1981, McCarty coined the term Milwaukee shoulder seen in 4 patients with identical clinical presentations and joint fluid with active collagenase, neutral proteinase, and hydroxyapatite crystals.4 In 1983, Neer et al1 introduced the term cuff tear arthropathy to describe the presentation of 26 patients with massive RC tears and glenohumeral arthritis treated with a total shoulder replacement. Over the last century, several reports of similar clinical presentations established various theories as to how patients developed the condition. Several theories on the etiology of CTA have been discussed. There exists no consensus among reports. The rheumatologic literature has emphasized the biochemical aspects of the condition, whereas the orthopedic descriptions have emphasized the mechanical factors.5–12 Reports of a hemorrhagic theory for CTA focused on the presence of a hemarthrosis in patients with severe glenohumeral arthritis and massive RC tears. In 1967, DeSeze6 first described this in 3 patients; however, later reports by Baudin5 in 1969 and Lamboley7 in 1977 noted similar presentations. Another group of reports focused on the inflammatory nature of the disease process. The Milwaukee shoulder was introduced in the rheumatology literature by McCarty in 1981.4 This condition, reported mostly in women, consisted of massive RC tear, glenohumeral arthritis, bony destruction, and joint instability. The hemarthrosis present contained calcium phosphate crystals, active collagenase, protease activity, and inflammatory cells.4,8,9 The description of the Milwaukee shoulder emphasized the central role of calcium phosphate crystals. These crystals are phagocytized by synovial cells activating the release of destructive enzymes, which act on periarticular tissue and joint surfaces.4,8–17 Antoniou et al10 noted an association between the apatite crystals, massive RC tears, and glenohumeral arthritis. These crystals were seen with high levels of PGE2 in the synovial fluid of patients with CTA. The result is a picture of severe degenerative arthritis with significant bone loss and soft tissue destruction. Figure 6–1 (A) The spectrum of disease. (B) Classic cuff tear arthroplasty. The nutritional theory emphasizes the role of the RC as a structural barrier. As noted by Neer and colleagues,1 extravasation of synovial fluid in the presence of massive RC tears results in an inadequate diffusion of nutritional components necessary for articular cartilage metabolism. Additionally, by not using the joint, alterations in articular content (i.e., water content) and disuse osteopenia develop. This results in cartilage atrophy, subchondral osteopenia, and collapse of the humeral head. Perhaps the most significant role that the RC plays in CTA is described in the mechanical theory. Neer et al1 was the first to emphasize this role. The instability that results from RC deficiency is the first step toward the development of CTA. Loss of RC function results in a loss of the balanced force couples needed to establish a stable fulcrum for the glenohumeral joint.11 In this setting, the deltoid moment results in glenohumeral instability with excessive upward migration of the humeral head. Mechanical factors of glenohumeral instability from RC dysfunction and proximal migration of the humeral head to the point of acromial impingement result in degenerative changes seen on the humeral head, superior glenoid, and undersurface of the acromion. The end result is acetabularization of the shoulder joint with severe joint destruction. Table 6–1 Other Presentations of Cuff Deficient Shoulder
Historical Background
Classic Cuff Tear Arthropathy
Tendon loss |
Massive rotator cuff tear with minimal arthritis |
Massive rotator cuff tear with anterosuperior escape |
Infection |
Muscle loss |
Infection |
Severe glenohumeral arthritis with severe fatty infiltration of |
intact rotator cuff |
Bone loss |
Fracture sequelae |
Failed hemiarthroplasty for fracture |
Failed hemiarthroplasty with rotator cuff tear |
Failed hemiarthroplasty for cuff tear arthropathy |
Failed bipolar hemiarthroplasty |
Tumor resection |
Infection |
Nerve loss |
Chronic Erb palsy |
Suprascapular nerve palsy |
Post-polio |
The connection between massive RC tears and the development of classic CTA has not been clearly elucidated. Neer et al1 estimated that 4% of patients with RC tears would develop CTA. Hamada and colleagues,12 however, noted progressive degenerative changes in 5 of 7 patients with massive RC tears, suggesting that massive RC tears would ultimately lead to progressive degenerative changes. In a cadaveric study, Feeney et al13 showed a strong correlation between tears of the RC and articular cartilage degenerative changes, as they found articular cartilage damage in all 10 shoulders that had RC tears. Nonetheless, Rockwood and colleagues14 noted no progression of glenohumeral degeneration in patients with massive RC tears 6.5 years after open acromioplasty and débridement of the RC. The mere presence of a massive RC tear may not be enough to develop the progressive degenerative changes seen in classic CTA; however, these massive tears may result in severe functional loss. One would suspect that as the aging population increases, the incidence of problems related to the RC-deficient shoulder will surge.
Other Disease Presentations of the Rotator Cuff Deficient Shoulder
Several conditions result in disability due to RC deficiency (Table 6–1). The central role of the RC in providing shoulder function is clear. RC deficiency results in variable degrees of weakness and instability that result in a significant loss of function for the patient. Burkhart introduced the concept of balanced force couples to distinguish functional from dysfunctional massive RC tears.15 Once a balanced force couple is lost, the RC becomes dysfunctional.
Whether the massive RC tear occurs with minimal arthritis, severe arthritis (i.e., classic CTA), or isolated instability (i.e., anterosuperior escape), the function of the RC will ultimately determine the functional outcome. Reconstructive options must strongly consider the ability to restore a functional RC for reliable improvements to be achieved.
In cases where the RC tendon is intact, severe muscular atrophy of the RC may result in its dysfunction. This has been recognized in patients with severe osteoarthritis and an intact RC.16,17 In these patients when the arthritis is treated with a total shoulder arthroplasty, instability results. It is thought that the friction created by the severe arthritis creates a static stability. When this friction is replaced with a smooth articulating surface, RC dysfunction results in joint instability and failure of the joint replacement.
RC deficiency may also develop after failure of a RC repair or subacromial decompression. This may be the result of the natural history of the disease. However, the important role of the coracoacromial arch in preventing anterosuperior instability of the glenohumeral joint has been described.18 In cases where both the RC and the coracoacromial arch are deficient, the resulting anterosuperior instability results in significant disability and loss of shoulder function, often with pseudoparesis of the shoulder.
Several disease processes result in significant proximal humeral bone loss. The importance of proximal humeral bone is based on the RC insertion. As proximal humeral bone loss becomes more severe, the loss of RC insertion becomes greater. In severe cases of proximal humeral bone loss, significant weakness and instability will result. This is seen in cases of proximal humeral tuberosity malunion, nonunion, or resorption, where the RC becomes dysfunctional due to loss of its secure attachment. Similar findings are seen in cases of failed hemiarthroplasty for proximal humerus fracture, after tumor resection, and as a result of infection. Infections of the shoulder can be particularly devastating, as loss of RC is coupled with significant joint destruction and bone loss with limited reconstructive options.
Classification of Rotator Cuff Deficiency
To date, the only attempts at classifying RC deficiency have been based on radiographic classifications. Two attempts have been made to classify the RC-deficient shoulder into distinct radiographic groups.19,20 It has been reported that these radiographic distinctions may help to guide shoulder surgeons in selection of appropriate treatment plan.20 Both radiographic classification systems describe several grades of degeneration, bone loss, and fixed instability.
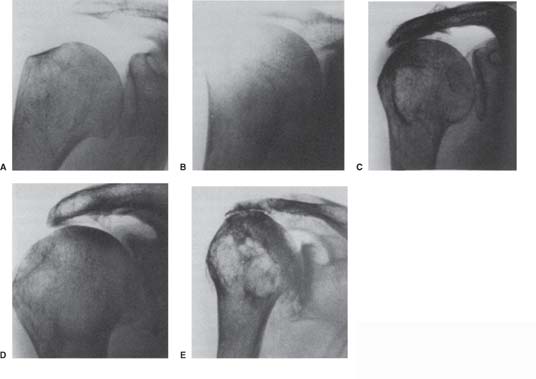
In 1990, Hameda et al19 proposed the first classification of massive RC tears. The classification was based on a series of 22 massive cuff tears that were treated nonoperatively. Five radiographic grades were described (Fig. 6–2). They noted progression to CTA in one patient. They concluded that patients with massive RC tears will ultimately progress to CTA. Along the way, progressive radiographic changes develop due to rupture of the long head of the biceps, establishment of an abnormal fulcrum of the humeral head against the acromion and the coracoacromial ligament, and progressive weakness of external rotation.19
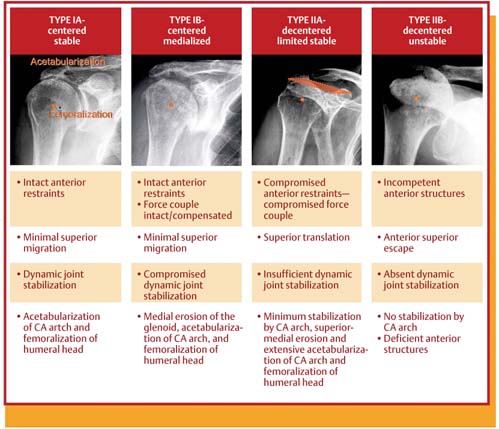
Seebauer et al20 was the first to emphasize the importance of joint stability. The Seebauer classification of CTA (Fig. 6–3) has four radiographic stages with two types and two subtypes. Patients with type 1 have centered joints that are stable, whereas patients with type II have lost stability of the joint. Patients with type IA have developed acetabularization of the coracoacromial arch with rounding of the humeral head. These patients have maintained joint stability with intact anterior structures as noted by the minimal amounts of superior migration of the humeral head. Type IB differs in progressive loss of the anterior restraints. These patients have compromised, but maintained dynamic joint stabilization with minimal superior migration of the humeral head. As the anterior structures of the shoulder become compromised, progressive instability results. Thus patients with type IIA and type IIB show radiographic evidence of fixed instability. In type IIA, superomedial erosion and extensive acetabularization of the coracoacromial arch are seen. The humeral head is superior translated. Instability is the hallmark of type IIB, as the arthritic changes are minimal. The humeral head is described in an anterosuperior position due to a deficient coracoacromial arch.20
The Seebauer classification has been used to establish algorithms for the management of CTA.20,21 Based on these algorithms, patients with type IA can be successfully managed using hemiarthroplasty, because the joint remains centered. On the other hand, patients with radiographs classified as type IIB should be managed with a reverse prosthesis to treat the underlying joint instability.
Figure 6–2 (A–E) Hamada classification of massive rotator cuff tears.
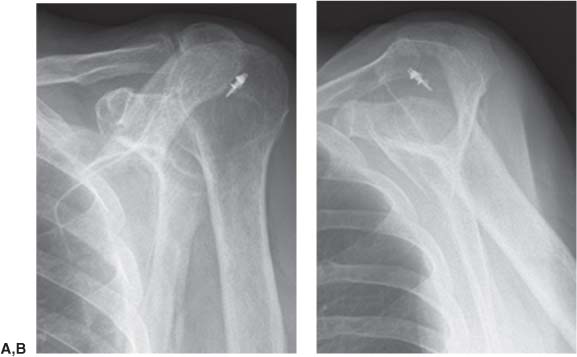
The use of any radiographic classification system as a treatment algorithm should be done so with caution. Treatment of CTA requires a clear understanding of the pathology present. Although aspects of this are seen on radiographs (i.e., bone loss and loss of smooth articulating surfaces), much of the pathology is not seen. A clear example is a patient with anterosuperior instability due to RC and coracoacromial arch deficiency. This patient may have seemingly normal radiographs (Fig. 6–4). This radiograph does not fit into any current classification system. However, when a dynamic radiograph is performed in attempted forward elevation, the dynamic instability clearly becomes evident (Fig. 6–5).
Figure 6–3 Seebauer classification of cuff tear arthropathy. CA, coracoacromial. From Visotsky JL, Basamania C, Seebauer L, Rock-wood CA Jr., Jensen KL. Cuff tear arthropathy: pathogenesis, classification, and algorithm for treatment. J Bone Joint Surg Am 2004; 86:38. Adapted by permission.
Although radiographic classification systems may be useful, they do not accurately represent the spectrum of disease seen in the RC-deficient shoulder. To classify RC deficiency accurately, a proper understanding of the pathology present is necessary. A more reliable classification system would grade each of the pathological changes present and incorporate relevant radiographic findings.
Pathology
Identification and understanding the pathological changes seen in the RC-deficient shoulder are essential for proper diagnosis and management of the disease. The structures that may undergo pathological change include the RC muscle and tendon, articular surfaces of the glenohumeral joint, bone support of the glenoid and humeral head, surrounding capsule, position of the glenohumeral joint, the deltoid muscle, and the subdeltoid, subacromial, and subcoracoid space (Table 6–2). Each of these pathological changes plays significant roles in the disease process and may dramatically influence selection of treatment plan. Once the extent of the pathology present in the involved shoulder can be asserted, information from the clinical picture can be integrated to form a logical treatment strategy.
Figure 6–4 Static anteroposterior (A), Y (B), and axillary (C) radiographs of 6-month follow-up after subacromial decompression and mini-open rotator cuff repair.
Loss of Rotator Cuff Muscle and Tendon
The essential component of RC deficiency is directly related to the amount of RC function lost. The size of the RC tendon tear is the most obvious aspect of this pathology, because the larger the RC tendon tear, the more the functional loss.22,23 However, the degree of muscle loss may be even more significant. Fatty infiltration of the RC muscle after RC tendon tears has been previously described by Goutallier et al24 based on computed tomography (CT) scans (Table 6–3). These muscular changes seen after RC tendon tears may be irreversible, even after a successful tendon repair.25,26 A critical level of RC muscle and tendon loss will result in significant functional loss including weakness and joint instability.27
Figure 6–5 Dynamic forward elevation anteroposterior (A) and Y (B) radiographs demonstrating clear anterosuperior escape.
In patients with RC deficiency, the RC is unable to provide these important roles. Reconstructive efforts must thus consider whether these functions can be reliably restored, or whether efforts should be made to compensate for the loss of strength and stability. Once instability has developed from RC deficiency, the reliability of soft tissue procedures at restoring stability becomes diminished. Preoperative magnetic resonance imaging (MRI) or CT scans are useful in predicting the size of the tendon tear and the degree of fatty infiltration present in the RC muscle.24 Additionally, intraoperative decision making may be useful in determining if the RC is salvageable.
Table 6–2 Pathology Present in the Rotator Cuff Deficient Shoulder
Rotator cuff deficiency |
Massive tear without loss of force couples |
Massive tear with loss of force couples |
Fatty infiltration |
Humeral head |
Cartilage loss – complete, superior, eccentric, central |
Bone loss–eccentric, central |
Femoralization |
Sclerosis |
Peripheral osteophytes |
Subchondral cysts |
Glenoid |
Cartilage loss – central, eccentric (anterior, superior, posterior, anterosuperior) |
Bone loss – central, eccentric (anterior, superior, posterior, anterosuperior) |
Sclerosis |
Peripheral osteophytes |
Subchondral cysts |
Joint position |
Central |
Static superior |
Static anterosuperior |
Dynamic anterosuperior |
Static posterior |