The Shoulder and Upper Extremity
David J. Petron
Umar Khan
Section A The Shoulder
The shoulder is the most vulnerable joint in the human body. It is also one of the most complicated anatomical and biomechanical joints. Sports medicine specialists have begun to redirect their attention from the problems of the knee to the complexities of the shoulder. Advances in arthroscopy have changed treatment protocols and extended the competitive lives of athletes, especially throwing athletes. The shoulder is a site of major injury in competitive sports, including a variety of injuries ranging from those involving joints (e.g., glenohumeral [GH] dislocations, acromioclavicular [AC] separations), to those involving bones (e.g., fractures of the clavicle, upper humerus), to those involving muscles and tendons (e.g., rotator cuff injuries). In a study involving 336 elite college football players, approximately half had a history of shoulder injuries. The most common injuries were AC separation (41%), anterior instability (20%), rotator cuff injury (12%), clavicle fracture (4%), and posterior instability (4%). The most common surgeries performed were anterior instability reconstruction (48%), Mumford/Weaver-Dunn surgery (15%), posterior instability surgery (10%), and rotator cuff surgery (10%) (1).
Anatomy/Biomechanics
To put the anatomy of the shoulder in perspective, one needs to consider evolution. As we evolved from a quadruped to a biped, we ceased to use our upper extremity for weight bearing. The shoulder remains a ball and socket joint but the borders of the socket have fallen back to allow the greatest range of motion (ROM) of any body joint. In contrast, the hip joint maintains much of its stability because it is a deep ball and socket joint. To make up for a loss of dynamic stability, the shoulder relies heavily on the musculature of the rotator cuff. What the shoulder has given up in stability, it gains in ROM.
The shoulder exhibits the following three planes of motion:
Sagittal—flexion, extension, and elevation
Coronal—adduction and abduction
Medial—internal and external rotation
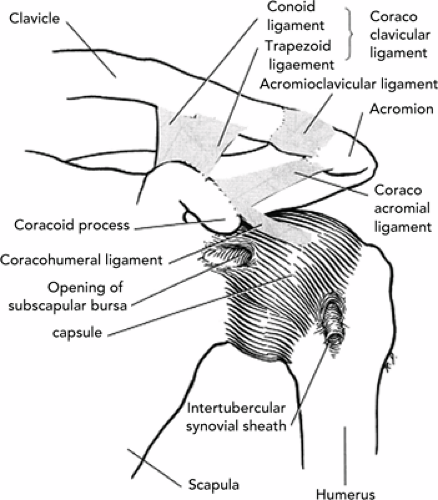
The functional anatomy of the shoulder includes five articulations (see Figure 25A.1). From distal to proximal these are as follows:
Glenohumeral. The shoulder joint and major articulation of the upper extremity. This joint can be described as an incongruent joint that uses a gliding motion about a nonfixed axis of rotation. It is made up of the concave surface of the glenoid fossa and the more circular convex surface of the humeral head. During motion only a small portion of the humeral head is in contact with the fossa at any one time. Supporting soft tissue structures intimate to the joint include the glenoid labrum, joint capsule, and the anterior placed GH ligament. The joint capsule is normally loose, becoming taut only in extreme movements (the external rotation and abduction of throwing) beyond the normal ROM of the joint. Movement between the shoulder and elbow is coordinated by the long head of the biceps muscle. The long head of the bicep’s proximal tendon runs intracapsularly but extrasynovially through the GH joint.
Suprahumeral. Not a true joint but a physiological one. This protective articulation is between the humeral
head and the coracoacromial ligament. It allows the greater tuberosity of the humerus to pass under the coracoacromial ligament without compression during abduction. This is the site where most shoulder impingement occurs.
Scapulothoracic. Another physiological joint. The motion of the scapula is to glide along the posterior thoracic wall when there is motion and rotation of the clavicle. This movement is produced by the coordinated movement of two muscles—the trapezius and serratus anterior muscles.
Acromioclavicular. A plane joint containing a meniscoid structure. This meniscoid structure rapidly degenerates and disappears by the fourth decade of life. The AC joint is stabilized by the AC and coracoclavicular (CC) ligaments. The physiological movement of the clavicle is by rotation when the arm is adducted or elevated.
Sternoclavicular. A plane joint that acts as a ball and socket joint. The anterior and posterior sternoclavicular ligaments reinforce a loose fibrous capsule making up the joint. Stability is aided by the costoclavicular and infraclavicular ligaments.
Bursae. There are usually a total of eight bursae present around the shoulder joint.
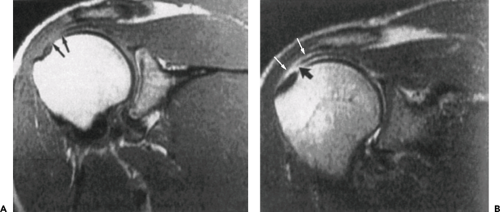
Only the large subacromial bursa is clinically significant (see Figure 25A.2B).
Glenoid labrum (Figure 25A.2A). The fibrocartilaginous labrum acts to expand depth and increase the area of the glenoid. It is triangular on cross section with a thin, free intra-articular apex and three sides that face the humeral head, the joint capsule, and the glenoid surface, respectively. The labrum is anchored to the glenoid at the periphery. The presence of an intact labrum increases humeral contact area by up to 75% in the vertical plane and 56% in the transverse plane. This additional contact area improves GH joint stability without compromising motion.
Joint capsule. Mobility is further enhanced by a thin joint capsule that has almost twice the surface area of the humeral head. This allows tremendous ROM. The passive stability is provided by selective tightening of various portions of the joint capsule depending on arm position. At rest, with the arm in a dependent position, the superior portion of
the capsule is taut and the inferior region is lax. With overhead elevation this relation is reversed. External rotation tightens the anterior and releases the posterior capsule whereas horizontal flexion does the opposite.
GH ligaments. Structural reinforcement of the anterior capsule is provided by folds in its inner wall that have been designated as the superior, middle, and inferior GH ligaments. The most significant of these structures is the inferior GH ligament. It is the primary restraint to external rotation at 90 degrees of shoulder abduction. Overhead athletes often place their arm in this position and risk injury of the inferior GH ligament.
Important Muscles
Deltoid. Acts as an elevator of the arm. This is a superficial muscle that normally contributes the round, contoured look to the anterior and lateral profile of the shoulder. It initiates abduction.
Supraspinatus. Initiates arm elevation and primarily depresses the humerus during abduction. It passes under the acromion and coracoacromial ligament and can be easily “pinched” between these structures and a moving humeral head. This is the main tendon affected with impingement syndrome.
Subscapularis, infraspinatus, and the teres minor act synergistically as a conjoined tendon to compress the joint and displace the upper extremity downward: (a) subscapularis—responsible for internal rotation; (b) infraspinatus and teres minor—responsible for external rotation.
Note: The latter four muscle attachments to the humerus make up the rotator cuff of the shoulder (see Figure 25A.3).
Generic Examination
Because of the complexity of the shoulder, we will discuss the important subjective and objective aspects without relation to any specific shoulder diagnosis (see Table 25A.1).
History
When confronted with an undiagnosed shoulder injury, the physician must elucidate the exact mechanism of injury and position of the shoulder at the time of injury. The history should include the following:
Mechanism of injury. Did the patient fall on the outstretched hand? (“FOOSH” injury) This could indicate shoulder dislocation or fracture injury. Did the patient fall directly on the tip of the shoulder or did he/she land on the elbow, driving the humerus upward? This finding may indicate an AC disruption or subluxation. Did the shoulder feel loose or like it was “coming out?” This may indicate instability. Was the onset insidious and, now, the patient has pain only with overhead motion? This may be impingement syndrome. Please see Appendix 25A.1 for images.
Movements. Are there movements that cause pain or problems? Cervical spine movements may cause pain in the shoulder. Abduction and external rotation of the shoulder may lead to apprehension, which indicates anterior instability. Pain during certain phases of throwing such as cocking or acceleration phases) may indicate anterior instability or internal impingement. Pain with simple overhead motion may indicate impingement syndrome. Instability and impingement frequently occur together. Night pain and resting pain are often associated with rotator cuff tears, subacromial
bursa pain (impingement syndrome), and, on occasion, tumors.
Handedness. A key element in the historical review. A conditioned athlete using his or her arm in sport (pitcher, volleyball player) will often have restriction in the ROM in their dominant as compared to the nondominant arm. The examiner should not attribute such alterations to a pathological state.
Occupation/position. Certain positions played in sports lend themselves to certain injury. A baseball catcher throwing overhand may be at more risk than a shortstop for an overuse injury or impingement syndrome. Overhead activity, such as swimming, volleyball, and throwing sports are at particular risk for injury. In an older patient, a simple overhead activity such as painting may start the cycle of impingement type pain.
Review of systems. Specific inquiry should be made of history of rheumatoid arthritis, diabetes mellitus, gout, or other systemic diseases. Also, the physician needs to know about previous surgery or trauma to the area.
Medication use. A history of both oral and injected medications is useful.
Age. Many problems of the shoulder are related to the patient’s age. Rotator cuff degeneration usually occurs in patients between 40 and 70 years of age. Calcium deposits frequently occur between the ages of 20 and 40. Rotator cuff tears, in patients under the age of 40, are almost nonexistent unless
associated with trauma. Frozen shoulder is seen in persons between the ages of 40 and 60 years if it results from causes other than trauma.
Inherent ligamentous laxity. Some individuals (and some sports) may possess generalized joint laxity (swimming). Do “loose joints” run in the family?
Pain. The characterization of pain, onset, and specific biomechanical actions generating the pain are obviously important. Training habits in relation to pain should be asked. The specific character of the pain can vary as follows:
Dull pain may indicate a rotator cuff tear.
Burning pain may indicate cervical radiculopathy.
An audible snap may indicate subluxation of the GH joint or biceps tendon.
Crepitation with passive motion may indicate a passive bursitis or scapular dyskinesia.
Referred pain (see Table 25A.2).
TABLE 25A.1 Differential Diagnosis of Rotator Cuff Degeneration, Frozen Shoulder, Atraumatic Instability, and Cervical Spondylosis | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 25A.2 Shoulder Pain from Other Disease Processes | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Physical Examination
Specific and unique aspects of examination of the shoulder include the following:
Inspection. Both shoulders should be exposed to allow comparison and to detect any signs of asymmetry. The authors recommend Y-style tank tops for female patients whenever possible. Also, an examination room mirror allows the physician to face the patient and still observe the posterior motion of the scapula on abduction and ROM testing. Look from both sides, back, and front especially noting muscle atrophy, erythema, swelling, or deformity.
With the patient sitting, look for atrophy in three sites; the supraspinatus fossa, the infraspinatus fossa, and the deltoid. This demonstrates weakness due to either a rotator cuff tear, or neurological deficit.
Palpation. The primary care physician should think of the topographical anatomy and, whenever possible, palpate both shoulders at the same time while the patient describes differences in sensation of tenderness. Feel for crepitation and spasm. The order of examination from proximal to distal on the upper extremity should be sternum, sternoclavicular joint, clavicle, AC joint, coracoacromial ligament, coracoid process, GH joint (passively abducting the upper extremity), biceps tendon and groove (passively performing external rotation), and scapula. The presence of pain, swelling, crepitation, muscle spasm, tenderness, or warmth may indicate underlying pathology (see Table 25A.3).
Neurovascular examination. This should include palpation of the pulses and a determination of the sensory and motor functioning, as well as of the deep tendon reflexes of the upper extremity. Test for deep tendon reflex and sensory perception (see Figure 25A.4 for dermatome distribution)
Axillary nerve—loss of sensation over the lateral aspect of the upper arm
Long thoracic nerve—winging of the scapula (serratus anterior muscle dysfunction).
Neck. ROM should be examined for any shoulder pain and for alignment of cervical vertebrae. Note any pain or tenderness over the paracervical muscles or spinous process. Abnormal movement patterns of the head and neck should be examined closely. Spurling’s test should be elicited to rule out cervical disc/nerve disease as a cause of shoulder pain.
Active range of shoulder motion. Evaluate: (a) abduction—determined by raising the outstretched arm laterally overhead while observing from behind; (b) flexion—assessed by having the patient raise the arms forward until they touch overhead; (c) internal rotation—the patient places the thumb as high as possible on the opposite scapula; (d) external rotation—the patient places his/her
hand on the same shoulder; (e) AC and sternoclavicular joints—the patient places the hands across the chest on the opposite shoulder; (f) horizontal flexion with the arm in abduction—ask the athlete to place his/her arm on the opposite shoulder; (g) protraction and retraction (see discussion on scapular motion); (h) shrug the shoulders—testing the 11th cranial nerve innervating the trapezius) ask the athlete to perform movements that cause pain or those that are believed to be associated with the condition (tennis serve or baseball pitch) (see Table 25A.4).
Passive range of shoulder motion. If the patient has difficulty performing any of the tests mentioned earlier in the active ROM segment, passively repeat each of the movements on the patient yourself.
Scapular motion. It functions as a stable base to allow (a) appropriate positioning of the glenoid; (b) maximize rotator cuff function. Alterations in scapular position and/or motion can occur both as a result or as a cause of injury. There are six possible motions in three different planes. (a) anterior/posterior (A/P) tilt in the sagittal plane; (b) interior/exterior rotation in the transverse plane; (c) upward/downward rotation in the frontal plane. One should observe the dynamic scapula motion from behind a seated patient. During abduction, as the scapula elevates it should tilt posteriorly, externally rotate, and upwardly rotate. Scapular dysfunction occurs when there is alteration in position and/or motion that deviates from normal. Proper stabilization and movement of the scapula is critical to maintain healthy shoulder mechanics. Its role in the function of the shoulder cannot be over emphasized. Scapular dyskinesia is the abnormal movement pattern of the scapula. There are three general patterns/types of dyskinesia. Type 1—winging or prominence of the inferior angle. Type 2—winging/prominence of the entire medial border. Type 3—winging/prominence of the superior medial border. These different patterns will guide the rehabilitation of the shoulder. Scapular dyskinesia has clinical implications in all sports, especially pitching. A lack of scapular retraction in pitching will lead to an inability to achieve a full set position during the late cocking phase and will diminish eccentric control (protraction) during follow-through. This places both the shoulder and elbow at risk for injury. Loss of inferior force couple (inferior scapula winging) leads to a loss of control of elevation with a relatively protracted scapula which can lead to impingement problems. Scapular dysfunction must be addressed as a part of the patients’ rehabilitation. Experienced physical therapists are helpful in retraining the scapula stabilizing muscles and returning normal scapular function. Scapula dyskinesia can be either a primary or secondary cause of dysfunction. Identification and treatment of causative factors is crucial to restoring proper scapulohumeral mechanics. Look beyond the shoulder complex as pain is often the symptom of dysfunction somewhere in the kinetic chain.
Muscle testing
Supraspinatus—resistance to initiation of abduction. The athlete’s arm should be placed at 90 degrees abduction, 60 degrees of horizontal flexion, and full internal rotation. The examiner directs the force downward with two fingers, not the whole hand (empty can sign).
External rotators (infraspinatus and teres minor muscles act as a unit)—arm should be adducted to the side, elbow at 90 degrees with the patient externally rotating against resistance.
Internal rotator (subscapularis)—with the arm still abducted to the side, the elbow at 90 degrees, and the forearm externally rotated, ask the patient to internally rotate against resistance. The Lift-Off test can also be performed. This involves having the patient place the
back of the hand against the lower back and attempt to move the hand away from the lower back. Failure to do so is a sign of subscapularis injury.
Palpate the long head of the biceps in the groove—external rotation is necessary to find the groove (see discussion on Speed’s test in the following text).
Deltoid—resistance/tenderness to abduction past 30 degrees. The deltoid initiates abduction.
Scapula stabilizing muscles, such as the serratus anterior (protraction) lower trapezius and rhomboids—essential to maintain normal scapular kinematics.
Tests
Apprehension. To test the stability of the GH joint, the arm is abducted and externally rotated while an anterior force is applied. A positive sign is when the patient resists rotation in apprehension of the pain (see Figure 25A.5). This may be performed either seated or supine (referred to as the crank test).
Load-and-shift test (see Figure 25A.5). The patient should sit with no back support and with the hand of the test arm resting on the thigh. The examiner stands behind the patient and stabilizes the shoulder with one hand over the clavicle and scapula. With the other hand the examiner grasps the head of the humerus. The humerus is gently pushed into the glenoid to seat it properly in the glenoid fossa. This is the load portion of the test, and this “seating” of the humerus allows true translation to occur. The examiner then pushes the head anteriorly or posteriorly noting the amount of translation. This is the “shift” portion of the test.
Sulcus sign. The patient’s arm is held at his side in a position of rest. The arm is gently pulled downwards while the examiner looks and palpates for a depression below the acromion.
Impingement tests. The arm is brought in extreme forward flexion with the humerus externally rotated (Neer’s impingement sign see Figure 25A.6). The arm is forward flexed to 90 degrees and medially rotated (Hawkin’s impingement sign—see Figure 25A.6) A positive sign is eliciting pain during movement (Painful arc see Figure 25A.6).
Roos maneuver. This test is used to assess for thoracic outlet syndrome. With this test the arms are abducted to 90 degrees laterally, the shoulder is rotated and the elbows are flexed to 90 degrees so the elbow is behind the frontal plane. Then the patient opens and closes the hands looking for ischemic pain on the affected side in less than 3 minutes.
Speed’s test for bicipital tendonitis. The shoulder is flexed forward to 90 degrees with the arm extended at the elbow and palm facing up. Pain in the region of the bicipital groove on downward force against resistance suggests bicipital tendonitis.
Hyperabduction. A test for thoracic outlet syndrome. Abduction of the arm causes numbness.
Crossover test. A test that differentiates impingement from AC/sternoclavicular injury. This can be done by asking the patient to flex the arm at the shoulder at approximately 90 degrees and adduct across the chest to try to touch the opposite shoulder. A positive test isolates pain to the AC joint.
Test for labral tears. The tests generally lack both specificity and sensitivity. Various tests include Clunk test, compression rotation test, anterior slide test, and O’Brien’s test.
The O’Brien’s test (see Figure 25A.7) evaluates for AC joint and/or labral abnormalities. The patient’s shoulder is flexed to 90 degrees with the elbow fully extended. The arm is then adducted 15 degrees and the shoulder is internally rotated so that the patient’s thumb is pointing down (like pouring out a glass). Downward force is applied against the arm against the patient’s resistance. The shoulder is then externally rotated so that the palm is facing up, and the examiner applies a downward force on the patient’s arm, which the patient is instructed to resist. A positive test is indicated by pain during the first part of the maneuver with the patient’s thumb pointing down, which is then lessened or eliminated when the patient resists a downward force with the palm facing up. Pain in the region of the AC joint is indicative of AC pathology, whereas pain or painful clicking deep inside the shoulder suggests labral pathology (2).
TABLE 25A.3 Suspected Injuries Based on Anatomical Location of Pain | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 25A.4 Normal Range of Motion at The Shoulder Joint and Muscles Involved | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Diagnostic Injections
Occasionally, injection of an anesthetic agent (Xylocaine) into a painful area can assist in making a diagnosis (see Figure 25A.8). It may be possible to determine if the pain origin is the GH or AC joint, subacromial bursae, long head of the biceps tendon, or the result of the biomechanics of an impingement syndrome (Barth, 1989). This is a procedure that should only be done by a physician who is comfortable with the anatomy of the shoulder and who has experience with injections.
Radiographic Studies
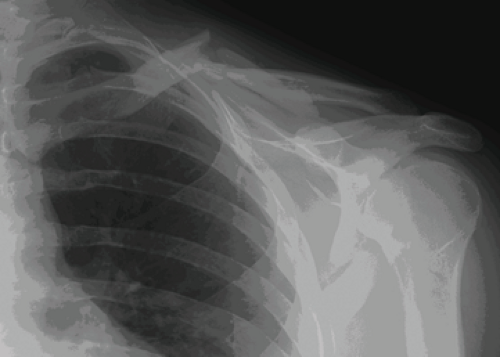
Standard x-ray studies should include the following four views:
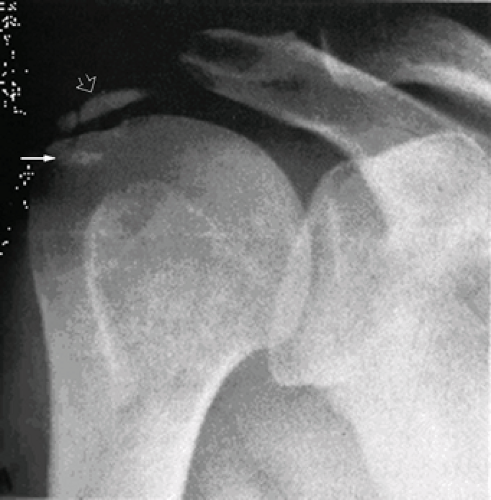
Anteroposterior views. One is in internal rotation and one in external rotation (see Appendix 25.1.7).
Lateral view/scapular-Y view. The Scapular-Y view is the best view for evaluating impingement and the type of acromion. The Hill/Sachs lesion (see Appendix 25.1.3) is also nicely evaluated. The Hill/Sachs lesion is caused when the humeral head is impacted against the glenoid of the shoulder. This lesion is an injury that causes damage to the head of the humerus. It is usually a complication of a shoulder dislocation. When the shoulder dislocates, the smooth cartilage surface of the humerus is impacted against the rim of the glenoid.
Radiographically it demonstrates an impaction fracture on the posterior humeral head.
Axillary view. Taken with the arm abducted and the radiographic beam passing inferiorly to superiorly through the axilla to the cassette placed on the superior aspect of the shoulder. This is another lateral view of the shoulder and is excellent for evaluating the position of a shoulder dislocation, as well as glenoid fractures, os acromial, Hill/Sachs lesions, and the lesser tuberosity of the humeral head.
Other Diagnostic Tests
Other diagnostic tests may be performed for specific indications and they include the following:
Arthrogram—usually to show full thickness rotator cuff tears. It is invasive and has essentially been replaced with magnetic resonance imaging (MRI) or ultrasound.
MRI—is proving to be most useful in diagnosing soft tissue injuries to the shoulder. It is the gold standard method for noninvasive assessment of the rotator cuff. It is possible to differentiate partial from full thickness rotator cuff tears. Sensitivity of the test increases with MRI arthrogram, which is the test of choice when looking for labral pathology.
Ultrasound—notably helpful for partial or full thickness rotator cuff tears. The test requires experience for accurate interpretation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree