Chapter 5 The Shoulder
The shoulder is a complex series of joints that provide an extraordinary range of motion. This extreme mobility is accomplished, however, at the expense of some stability. This lack of stability, combined with its relatively exposed position, makes the shoulder vulnerable to injury and degenerative processes. Pain may develop not only from primary disease of the shoulder but also by referral from disorders of thoracic and abdominal origin, and these sources should be kept in mind, especially when more obvious causes are not apparent.
Anatomy
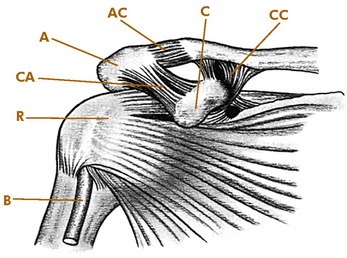
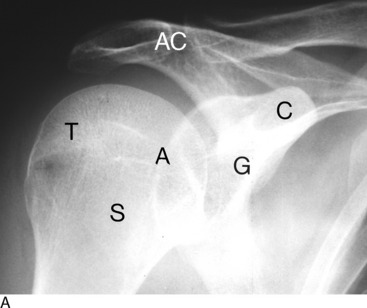
Four articulations constitute the shoulder joint: the glenohumeral, scapulothoracic, acromioclavicular (AC), and sternoclavicular joints. The stability of these joints is provided by a series of ligaments and muscles (Fig. 5-1).
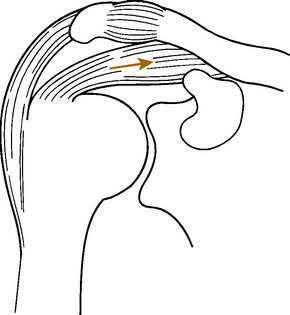
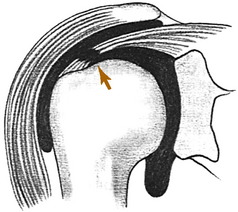
Motion of the arm results from the coordinated efforts of several muscles. With the initiation of shoulder motion, the scapula is first stabilized. The muscles of the rotator (musculotendinous) cuff, especially the supraspinatus, then steady the humeral head in the glenoid cavity and cause it to descend (Fig. 5-2). This prevents the rotator cuff from impinging against the acromion. Elevation of the arm results from a combination of scapulothoracic and glenohumeral joint movements. One third of total shoulder abduction is provided by forward and lateral movement of the scapula. The remaining two thirds occurs at the glenohumeral joint through progressively increasing activity of the deltoid and supraspinatus muscles. Thus, even in the complete absence of glenohumeral motion, scapulothoracic movement can still abduct the arm approximately 60 to 70 degrees.
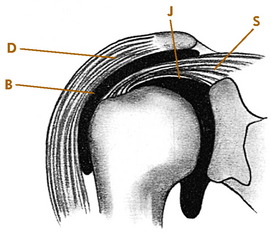
The coracoid, coracoacromial ligament, and underneath surfaces of the acromion and AC joint form a structure sometimes called the “coracoacromial arch.” The muscles of the rotator cuff (supraspinatus, teres minor, infraspinatus, and subscapularis) are separated from this overlying arch by the subacromial space. Bursal tissues occupy some of this space and may be affected by lesions of the musculotendinous cuff, AC joint, and adjacent structures (Fig. 5-3). They are frequently referred to as the subacromial bursa. Primary diseases of this bursa are rare, although secondary involvement is quite common. If bony abnormalities encroach on the subacromial space from above, the rotator cuff could be compressed as abduction occurs. When injections are given for rotator cuff disorders, it is the subacromial space that is injected.
Examination
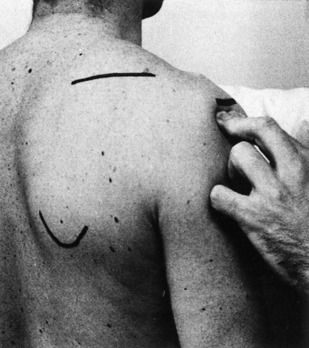
The examination is performed with both shoulders widely exposed (Fig. 5-4). The general contour of the shoulder is noted, as well as any atrophy or swelling. The shoulder is thoroughly palpated, and any areas of tenderness are determined. These are frequently located over the AC joint and the rotator cuff.
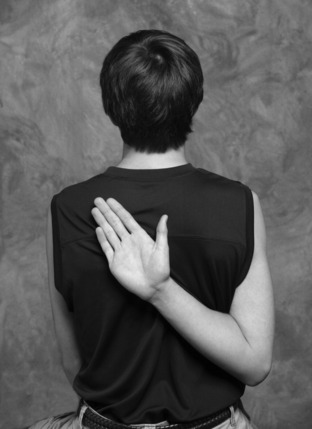
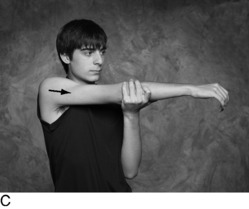
Active and passive ranges of motion are tested and compared with those of the opposite arm. The examiner should determine whether the scapula and humerus move together or independently. Any crepitus during the examination is also noted. Active motion is measured in abduction, forward flexion, and extension. External and internal rotation can be measured by instructing the patient to reach behind the head and then backward behind the shoulder blades. Limited internal rotation is often seen in conjunction with rotator cuff disorders. Involvement of the AC joint is tested by directing the patient to adduct the arm across the front of the chest and touch the opposite shoulder (Fig. 5-5). Pain with this test suggests AC or sternoclavicular disease. The strength of the shoulder, especially at 90 degrees of forward flexion and then at 90 degrees of abduction, is tested and compared with the opposite arm.
Roentgenographic Anatomy
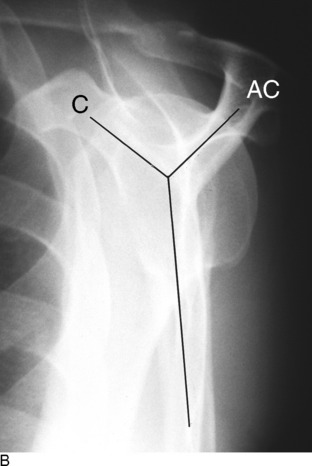
The shoulder is routinely examined by anteroposterior views with the arm rotated externally and internally (Fig. 5-6). A lateral view of the shoulder joint should always be taken. This may be obtained by utilizing a transaxillary or lateral scapular Y exposure. The scapular Y view is helpful in evaluating the shape of the acromion as well as assessing any bony abnormalities that could narrow the subacromial space. It is also valuable in determining if the humeral head is dislocated or not.
Disorders of the Rotator Cuff
TENDINITIS
A painful rotator cuff can develop at any age, although it is rare in children. It is sometimes related to chronic overuse. The term tendinitis has typically been used for this diagnosis, but the terminology is changing to reflect knowledge regarding the underlying pathology. Because the cellular changes associated with inflammation are often absent in these cases, the terms tendinopathy or tendinosis have been proposed. Small degenerative separations or “tears” of the rotator cuff may even develop over time. Scarring and thickening of the involved area of tendon and bursa occur, decreasing the distance between the cuff and the overlying coracoacromial arch. Bony abnormalities of the acromion may also be a factor in compromising this space. Pain and crepitus (“impingement”) may be noted when motions of the arm, especially abduction, squeeze and pinch these tissues between the humerus and the overlying arch. Even with an intact cuff, impingement may develop if the supraspinatus does not function effectively, allowing the humeral head to be pulled upward with deltoid contraction.
CLINICAL FEATURES
The major clinical manifestations are pain (especially at night for unknown reasons), tenderness, and occasionally atrophy. The patient is often unable to lie on the affected shoulder and may feel a locking or catching sensation with certain motions, especially abduction. The pain is often referred down the deltoid muscle. When abducting the shoulder, the patient may automatically turn the palm up, thereby externally rotating the shoulder, a maneuver that gives the rotator cuff more room beneath the coracoacromial arch. Active, palm-down abduction is frequently painful. Forced passive elevation of the arm may cause the supraspinatus to impinge against the acromion, causing pain. Pain may also be reproduced by internal rotation and forward flexion (Fig. 5-7).
Maximum tenderness is usually noted over the supraspinatus insertion at the acromiohumeral sulcus because this is the most common area of involvement, although palpable tenderness may be difficult to elicit in obese or muscular individuals. Internal rotation is often decreased because of contracture of the posterior capsule (Fig. 5-8). There is usually little actual loss of muscle power. The pain and crepitus are most severe in the arc of motion between 60 and 120 degrees of abduction. This is where the traumatized soft tissues are maximally compressed between the tuberosity and the overlying arch.
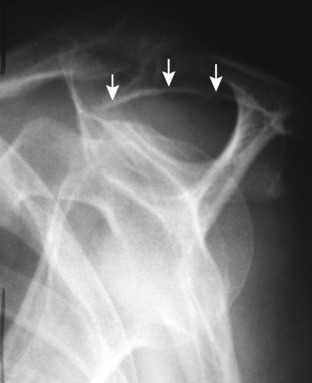
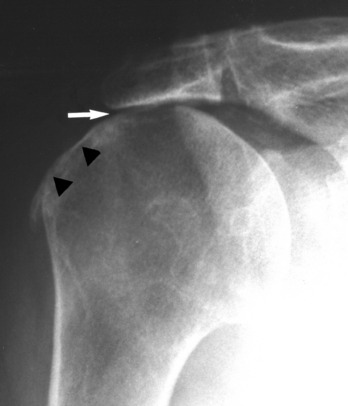
The roentgenogram is usually normal, but some sclerosis may be present in the tuberosity secondary to long-standing local irritation. Osteophytes or abnormalities in the shape of the acromion may be noted (Fig. 5-9).
TREATMENT
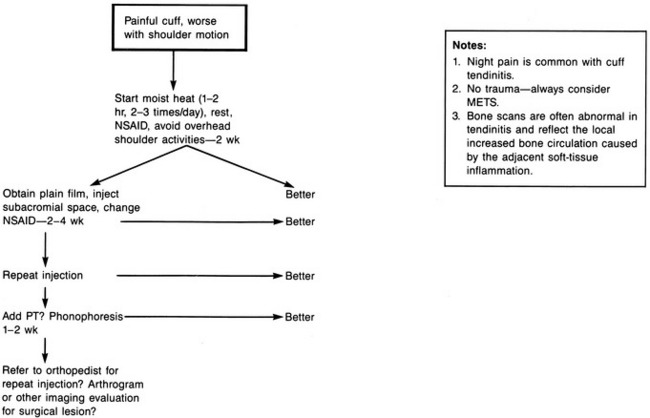
Improvement is usually seen within 3 to 5 weeks (Fig. 5-12). If it is not, a more serious cuff lesion, such as a rupture, should be suspected. At this point, the patient should be referred for orthopedic evaluation and possible magnetic resonance imaging (MRI). Surgery is reserved for those cases that fail to respond to conservative treatment and patients who have reparable underlying pathology.
RUPTURES OF THE ROTATOR CUFF
Ruptures of the rotator cuff are almost always chronic in nature and result from continued deterioration and degeneration (Fig. 5-13). The separation may be partial or complete. Ruptures are uncommon before the age of 40 years, although they may occur in young athletes. Acute tears are rare. Many ruptures are completely asymptomatic.
CLINICAL FEATURES
Obtaining a history sometimes reveals a fall on the outstretched hand or an attempt to lift a heavy object, but usually there is no obvious injury. Pain and weakness may become progressively worse, and the patient notes an inability to abduct or flex the shoulder, depending on the area of the rupture. The pain is often referred down the deltoid muscle. Occasionally, the patient may have had a previous history of chronic impingement pain, and the diagnosis of rupture is often considered only when the patient fails to respond to the usual treatment for tendinitis.
If the rupture is partial, the clinical findings are similar to those seen in chronic tendinitis, and even with complete rupture, the shoulder may have a full range of motion because of continued function of the other rotator muscles and deltoid. Usually, however, with both partial and complete ruptures, there is at least some weakness in abduction or flexion. The weakness is usually most severe in abduction, because the muscle most commonly torn is the supraspinatus. (Supraspinatus rupture or weakness causes loss of the depressor effect, allowing the head to ride up, which increases the sense of grinding.) If the rupture is more anterior into the subscapularis, forward flexion may also be weak. Weakness against external rotation suggests rupture of the infraspinatus. It may be impossible to actively abduct the arm more than 45 to 50 degrees, after which further abduction is obtained by scapulothoracic motion. Tenderness at the site of the tear is a common finding, and with complete ruptures a defect in the cuff may be palpated through the deltoid muscle. Passive range of motion is frequently normal in the pain-free shoulder, although there is usually a positive impingement sign. Sometimes in complete massive tears, the patient can only “shrug” the shoulder and may have to use the opposite hand to raise the arm any further.
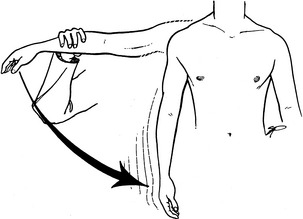
Atrophy of the cuff muscles is frequently present, and the “drop-arm” test may be positive if the tear is significant (Fig. 5-14). In this test, the arm is passively abducted to 90 degrees with the thumb pointing down, and then released. If the shoulder can maintain abduction, slight downward pressure is applied to the forearm, and the strength of the affected shoulder is compared with the normal shoulder. If pain is severe during the examination, lidocaine infiltration of the tender area can relieve the pain. The strength is then measured again. Inability to maintain shoulder abduction with this test is suggestive of a significant rotator cuff tear. Atrophy in the young is rare and should suggest nerve injury.
SPECIAL STUDIES
TREATMENT
Partial or small complete tears may respond to the conservative treatment program outlined for chronic tendinitis including occasional injections. Physical therapy (PT) and exercise are probably contraindicated in the presence of a separation. Occasionally, it is necessary to surgically repair the rupture and remove any impinging structures beneath the coracoacromial arch, especially in the young, active patient with high functional needs. Complete tears may also need repair if they are sufficiently disabling at any age. Often, however, there is very little loss of function and minimal pain, even with a complete rupture. In these patients, especially if they are relatively inactive, operative intervention is probably not justified.
CALCIFIC DEPOSITS IN THE ROTATOR CUFF
Calcium deposits in the rotator cuff tendon may be associated with pain and stiffness in the shoulder. Whether the calcific changes are a cause of symptoms or simply the result of degeneration is not known. Benign calcific deposits are a common incidental finding and probably result from degenerative changes in the same area where ruptures take place. They are most frequently found in the supraspinatus tendon. Most deposits remain small and deep in the tendon, and pain may be absent. Others may produce an inflammatory reaction and swelling, perhaps as the process of resorption takes place. Impingement of these swollen tissues against the overlying coracoacromial arch may then occur.
CLINICAL FEATURES
Roentgenographic examination in internal and external rotation usually reveals the deposit (Fig. 5-18). If the deposit is anterior in the subscapularis muscle or posterior, a transaxillary or Y view may be necessary to demonstrate it.
Disorders of the Biceps Tendon
TENOSYNOVITIS
CLINICAL FEATURES
The most common symptom is pain over the anterolateral aspect of the shoulder that may be referred down the anterior aspect of the arm. (Rotator cuff disorders usually refer pain down the lateral arm.) The most constant physical finding is tenderness to palpation over the bicipital groove. Active and passive shoulder motions are often restricted because of pain. Maneuvers that stretch the biceps tendon or cause it to glide in the groove may be painful. Forceful extension or abduction against resistance with the elbow extended and the forearm supinated may reproduce the pain (Fig. 5-19). Backward movement with the elbow extended may also be painful. The roentgenograms are usually normal.
TREATMENT
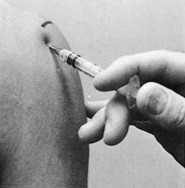
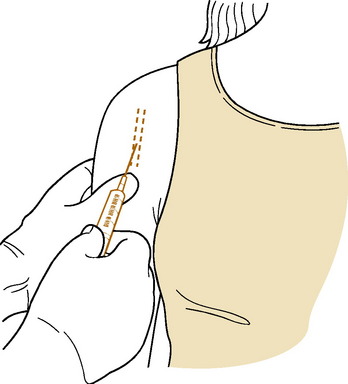
In the acute stage, treatment consists of rest, moist heat, and gentle range of motion exercises. All motions that stretch the biceps tendon should be avoided. A sling may be used temporarily. NSAIDs may be helpful, and local steroid injections into the tendon sheath are frequently beneficial (Fig. 5-20). The majority of cases respond well to conservative treatment. Surgery is recommended for those cases that fail to improve.
RUPTURE OF THE BICEPS TENDON
CLINICAL FEATURES
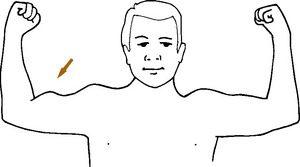
The onset is usually sudden. A sharp snap may be felt by the patient, followed by pain and weakness of the arm. The diagnosis is easily made by the observation of an abnormally large mass in the arm that represents the retracted muscle belly of the long head of the biceps (Fig. 5-21). There may be some loss of elbow flexion power, but after the discomfort subsides, the amount of weakness is usually minimal.