CHAPTER 17 The Role of Wrist Arthroscopy in Intra-Articular Distal Radius Fracture Management
Introduction
Lafontaine has described several radiographic features that signify when a fracture of the distal radius is unstable.1 These include initial dorsal angulation greater than 20 degrees, extensive dorsal comminution, associated ulnar styloid fracture, significant intra–articular involvement, and older patients greater than the age of 60.
The prognosis for intra–articular fractures of the distal radius has been shown to depend on numerous factors.2 These include the amount of radial shortening, residual extra–articular angulation, articular congruity of both the radiocarpal and radioulnar joints, and associated intra–articular soft–tissue injuries. Trumble et al., in their review of 52 intra–articular fractures, noted that factors that strongly correlated with a successful outcome included the amount of residual radial shortening and intra–articular congruity.3
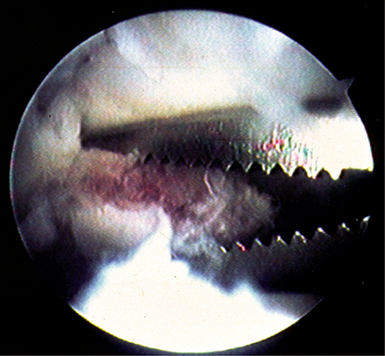
The use of wrist arthroscopy as an adjunct in the management of displaced intra–articular distal radius fractures takes advantage of its ability to view the articular surface with bright light and magnified conditions with minimal surgical morbidity.4 Fracture hematoma and debris may be arthroscopically lavaged, which potentially can improve the patient’s final range of motion5 (Figure 17.1). In addition, associated intra–articular soft–tissue injuries may be detected and managed at the same sitting6 (Figure 17.2). Pathology not readily identified on plain radiographs is frequently discovered during arthroscopic–assisted reduction and internal fixation of distal radius fractures. In most instances, it is much easier to manage an acute soft–tissue injury that occurs with a distal radius fracture than chronic pathology. The purpose of this chapter is to review the rationale and technique in the application of wrist arthroscopy as a useful adjunct in the management of displaced intra–articular fractures of the distal radius.
Two millimeters of articular displacement has over the past several years become a well–established critical threshold for articular incongruity of the distal radius. Knirk and Jupiter, in their classic article, demonstrated the importance of an articular reduction within 2 mm or less.7 A patient whose articular reduction is greater than 2 mm at final follow–up visit has a significantly higher incidence of degenerative changes within the wrist. Bradway and Amadio further substantiated these findings in their study.8
In their series of 40 patients, Fernandez and Geissler noted that the critical threshold may be as low as 1 mm or less.9 They reported in their study that the incidence of complications was substantially lower and articular reduction was within 1 mm or less.
Edwards et al. described the advantage of viewing intra–articular reduction by wrist arthroscopy compared to monitoring under fluoroscopy alone.10 In their series, 15 patients underwent arthroscopic evaluation of the articular surface of the distal radius following reduction and stabilization under fluoroscopy. They found that 33% of the patients had an articular step–off of 1 mm or more as viewed arthroscopically. Frequently, the fragment was rotated. Wrist arthroscopy is particularly useful in judging the rotation of fracture fragments, which is not readily identifiable under fluoroscopy. Edwards et al. concluded that utilizing wrist arthroscopy as an adjunct may detect residual gapping not previously identified under fluoroscopy alone.
A high incidence of associated intra–articular soft–tissue injuries involving the triangular fibrocartilage complex and the interosseous ligaments has been shown by several studies of displaced intra–articular fractures of the distal radius.11 Mohanti and Fontes, in two separate wrist arthrogram studies, noted a high incidence of tears of the triangular fibrocartilage complex associated with distal radius fractures. Fontes, in his series, noted a 66% incidence of tears of the triangular fibrocartilage complex in 58 patients.12 Similarly, Mohanti noted an injury of the triangular fibrocartilage complex in 45% of 60 patients in his series.13
Several recent arthroscopic studies have documented incidences of associated intercarpal soft–tissue injuries with fractures of the distal radius. In three recent published studies, an injury to the triangular fibrocartilage complex seems to be the most common associated intra–articular soft–tissue injury. Geissler et al. reported their experience in 60 patients with displaced intra–articular fractures of the distal radius undergoing arthroscopic–assisted reduction and evaluation.14 The criterion for surgical stabilization in his series was an intra–articular fracture displaced 2 mm or more that cannot be reduced by closed manipulation. In Geissler et al.’s series, 49% of the patients had a tear of the triangular fibrocartilage complex. An injury to the interosseous ligaments was less common. Tears to the scapholunate interosseous ligament were present in 32% of patients, and injury to the lunotriquetral interosseous ligament was identified in 15%.
Lindau, in a similar arthroscopic study of 50 patients, noted that tears of the triangular fibrocartilage complex were present in 78% of patients, injuries to the scapholunate ligament were identified in 54% of patients, and tears of the lunotriquetral interosseous ligament were less common and seen in 16% of patients.15 Hanker, in a series of 65 patients, noted that tears of the triangular fibrocartilage complex were very common and were present in 55% of the patients in his series.16 Although it is clearly documented that associated soft–tissue injuries are common with displaced intra–articular fractures of the distal radius, how they may affect the final outcome in patients is still unknown.
Geissler et al. described an arthroscopic classification of an interosseous ligament injury based on their work on arthroscopic management of fractures of the distal radius.14 They noted that a spectrum of injury may occur to the interosseous ligament. The ligament attenuates, and then eventually tears, and the degree of rotation between the carpal bones increases. The scapholunate interosseous ligament appears to tear from volar to dorsal. This arthroscopic classification of carpal instability is based on observation of interosseous ligaments from both the radiocarpal and midcarpal spaces (Table 17.1).
Table 17.1 Geissler Arthroscopic Classification of Carpal Instability
| Grade | Description | Management |
|---|---|---|
| I | Attenuation/hemorrhage of interosseous ligament as seen from the radiocarpal joint. No incongruency of carpal alignment in the midcarpal space. | Immobilization |
| II | Attenuation/hemorrhage of interosseous ligament as seen from the radiocarpal joint. Incongruency/step-off as seen from midcarpal space. A slight gap (less than width of a probe) between the carpal bones may be present. | Arthroscopic reduction and pinning |
| III | Incongruency/step-off of carpal alignment is seen in both the radiocarpal and midcarpal space. The probe may be passed through gap between the carpal bones. | Arthroscopic/open reduction and pinning |
| IV | Incongruency/step-off of carpal alignment is seen in both the radiocarpal and midcarpal space. Gross instability with manipulation is noted. A 2.7-mm arthroscope may be passed through the gap between the carpal bones. | Open reduction and repair |
The normal scapholunate and lunotriquetral interosseous ligaments have a concave appearance between the carpal bones as viewed from the radiocarpal space. The scapholunate ligament is best seen with the arthroscope in the 3–4 portal. The lunotriquetral interosseous ligament is best observed with the arthroscope placed in either the 4–5 or 6–R portal. The lunotriquetral interval will not be adequately seen with the scope in the 3–4 portal alone. In the midcarpal space, the scapholunate interval should be tight and congruent without any articular step–off. Similarly, the lunotriquetral interval should be congruent, but usually a 1–mm step–off or slightly increased play may be seen between the lunate and triquetrum as observed from the radial midcarpal space. A probe or needle may be inserted in the ulnar midcarpal space to evaluate the amount of play between the carpal bones.
A traction tower is very useful in the arthroscopic–assisted management of intra–articular fractures of the distal radius. A traction tower allows the surgeon to flex, extend, and radial and ulnar deviate the wrist to help reduce the fracture fragments while maintaining constant traction to allow visualization. A new traction tower was designed to allow the surgeon to simultaneously evaluate arthroscopically the articular reduction and to monitor the reduction under fluoroscopy (Figure 17.3). The traction bar is uniquely placed at the side of the wrist rather than at its center, so that it does not block fluoroscopic evaluation and the surgeon does not need to work around a central bar. In addition, by having the traction bar at the side rather than centrally allows the surgeon to simultaneously arthroscope the wrist and stabilize the fracture while obtaining access through a standard volar approach.
The surgeon can fluoroscopically evaluate the position of the plate and screw insertion during stabilization. This new traction tower allows a surgeon to perform arthroscopic–assisted fixation in both the vertical and/or horizontal planes, depending on the surgeon’s preference.(Figure 17.4). If a traction tower is not available, the wrist may be suspended with finger traps attached to a weight over the end of a hand table in the horizontal position, or with a shoulder holder in the vertical position. A small bump is useful to place under the wrist if weights are being utilized over the end of the table to maintain the wrist in slight flexion.
Fractures without extensive metaphysial comminution are most ideal for arthroscopic–assisted management. Radial styloid fractures, die punch fractures, three–part T fractures, and four–part fractures are all amenable to arthroscopic–assisted reduction and internal fixation.17 Some three–part fractures and most four–part fractures are managed through a combination of open reduction and arthroscopic–assisted fixation. In these instances, the fracture is stabilized by a volar plate through a volar approach (but the joint capsule is not incised). Articular reduction may be arthroscopically fine–tuned, and the distal screws inserted to stabilize the fracture. Associated soft–tissue injuries are detected and managed in the same sitting.