Pressure ulcers remain a significant secondary complication for many individuals with spinal cord injury (SCI). Technological advances have the potential to affect both the prevention and treatment of pressure ulcers. The focus of this article is hi-tech devices and methodologies. The current state-of-the-art methods are discussed and conceptual approaches are presented.
Pressure ulcers remain a significant secondary complication for many individuals with spinal cord injury (SCI). Technological advances in nonmedical fields, such as nanotechnology, are proceeding rapidly. Such hi-tech developments have the potential to affect both the prevention of future chronic wound development and the care of existing pressure ulcers. There is also a potential benefit in using developments that are initialized outside of the medical field, because high research and development costs are more readily absorbed by high-volume applications and may then be available at lower relative cost for comparatively low-volume medical care. For example, sensors developed for the automotive industry may have applications in the field of wound care.
The focus of this chapter is hi-tech devices and methodologies, which have the potential to have a significant impact on the field of pressure ulcer prevention and treatment. The current state-of-the-art methods are discussed with descriptions of currently available methods and research study findings. Conceptual approaches will also be presented, including therapeutic methods and devices that could become available in the next 5 to 10 years.
The options for pressure ulcer prevention are currently limited; however, as multidisciplinary approaches are integrated with improved clinical care, the potential impact of nontraditional approaches is great. There are many current options for treatment, and more continue to be developed that incorporate recent advances in fields such as biotechnology, imaging, and device design. In the current review, both the current state-of-the-art and conceptual approaches are discussed. Novel drug therapies are outside the scopes of this review and are not discussed.
Prevention of pressure ulcers
The assessment of techniques and devices to prevent pressure ulcer formation faces the challenges inherent in any attempt to determine the effectiveness of a prevention strategy. The initial basic research must develop efficacious techniques to reduce morbidity and improve quality of life. It is relatively straightforward to define the concept of pressure ulcer prevention as delaying or averting the development of a pressure ulcer. However, in practice, it is very difficult to objectively measure nonoccurrence of events without either controls or very large subject groups. Pressure ulcer development is known to be multifactorial, with applied pressure, duration of applied pressure, and blood flow (or tissue oxygenation) being among the primary factors. However, the relative weight of different factors has not been established fully. Surrogate indicators of changes in risk status may be used; however, care must be taken to ensure that outcomes measures are reliable, objective, and quantifiable.
Current state-of-the-art methods
Interface pressure mapping and monitoring of pressure ulcer risk status
Applied pressure has been used most frequently as a primary outcome measure in studies of devices, such as cushions, to prevent pressure ulcer development. The primary reason for this choice is pragmatic, namely that interface pressure mapping systems are widely available and established in both research and clinical settings.
The Skin Care Research Team (SCRT) at the Louis Stokes Cleveland DVA Medical Center has been investigating the use of a four-channel gluteal electrical stimulation system (GSTIM) to decrease risk factors associated with pressure ulcer development for individuals with SCI . The semi-implanted system comprised implanted percutaneous electrodes together with an external stimulator. Assessment of seating posture was performed both during quiet sitting (static mode) and during use of the GSTIM system for weight shifting by alternate gluteal contractions (dynamic mode). To determine the sustained effects of long-term use of the GSTIM system, repeated measures were made over a period of several months and years.
In this research study there was a requirement to monitor the effect of using the GSTIM system over time. Multiple outcomes measures were used, including interface pressure mapping. The research methodology has many similarities with the use of interface pressure mapping as an assessment tool in wheelchair and seating clinics . In the clinic setting, patients often are evaluated several times, either on different cushions or over repeated visits to the clinic. There is a need to compare multiple assessments reliably using objective outcomes variables. To meet the research need in the GSTIM study, the Longitudinal Analysis with Self-Registration (LASR) statistical algorithm was developed to compare multiple pressure mapping datasets. This software tool also has the potential for widespread clinical implementation.
It is very challenging to ensure that the individual who is being assessed sits in exactly the same position at each assessment, particularly when assessments are at intervals of several weeks. In our research study, we were interested in both the short-term effects of GSTIM-induced weight shifting produced by alternating side-to-side gluteal contractions and the long-term effects of dynamic GSTIM use. It was therefore necessary to align pressure map images in both space (seated position) and time (phase of weight shifting).
The multistage LASR algorithm provides both spatial and temporal self-registration of pressure maps to allow comparison of repeated assessments over time for a single patient. The LASR output map shows the locations of statistically significant pressure changes across the entire mapped region without the requirement to predefine regions of interest. This allows clinicians and researchers to obtain more comprehensive, objective information including significantly different overall pressure distributions and the relative efficacy of pressure relief maneuvers. Output maps can be viewed as two-dimensional or three-dimensional “snapshots” of a single data frame or as movies ( Fig. 1 ). Application of the LASR algorithm to paired pressure data sets requires a total processing time of 2 to 3 minutes after input of the raw data to production of the LASR output map, thus making it feasible for use in clinical settings.
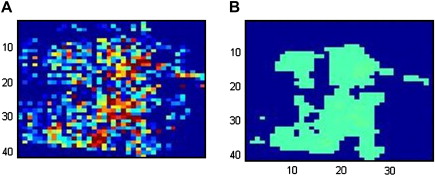
LASR movies are particularly useful for determining the effectiveness of weight-shifting procedures; in our research study, weight-shifting was achieved using the GSTIM system. In the clinical setting, the efficacy of independent pressure relief procedures or dynamic cushions could be determined from LASR output movies. Examples can be found at http://stat.case.edu/lasr/ . As seen in Fig. 1 , the LASR algorithm showed that long-term use of the GSTIM system produced a significant decrease in ischial region seating interface pressures; these changes were sustained with routine daily GSTIM usage for more than 7 years in an individual with a C4 American Spinal Injury Association (ASIA) A tetraplegia .
Dynamic pressure cushions and pressure alert systems
To minimize the risk of pressure ulcer development, a regime of regular pressure relief is essential. Adequate pressure relief can be achieved either by total removal of body weight from the loaded area or by weight-shifting to redistribute pressures. Individuals with spinal cord injury are recommended to change position every 2 hours when lying in bed and to perform pressure relief procedures every 15 to 20 minutes when seated in the wheelchair.
Individuals with impaired sensation and mobility often find it very hard to adhere to such a rigorous regime, because they do not feel pain or discomfort and also because they are unable to effectively weight-shift independently. For example, people with tetraplegia do not have sufficient upper body strength or trunk stability to perform independent pressure relief maneuvers. The current state-of-the-art method for independent pressure relief includes tilt-and-recline wheelchairs and dynamic pressure relief systems. There are a number of dynamic pressure-alternating support systems currently available commercially. The most options are available in alternating or low-air-loss mattresses. These devices are used routinely in many clinical settings and are considered both reliable and effective, although a recent Cochrane Report found that the relative merits of these hi-tech devices have not been clearly shown .
Dynamic wheelchair cushions may provide a means for reducing or varying interface pressures while seated. These devices work on the same principles as alternating pressure mattresses systems. In the past, alternating pressure cushions has not been as well embraced as a standard of care as mattresses. Early systems had many problems with reliability and were often too heavy for use in a manual wheelchair. Burns and Betz reported that mean ischial region pressures were significantly lower with a dynamic wheelchair cushion during the low ischial pressure phase when compared with a gel cushion and tilted seating posture. However, there was little difference between the dynamic cushion and a dry flotation cushion with tilted posture. Furthermore, the high ischial pressure phase produced higher mean regional pressures than either the gel or dry flotation cushion when seated upright in a tilt-in-space wheelchair.
Technological developments, including smaller, light-weight pumps and customization, have allowed some of these issues to be addressed. The USA Tech-Guide, produced by the United Spinal Association, currently lists more than 15 different powered alternating cushions from nine different manufacturers . The majority of these cushions provide a regular pressure relief cycle of alternating rows or groups of cells inflating and deflating together. Pressure variation operates on a fixed cycle, typically of 4 to 5 minutes in duration. Some systems offer the capability to adjust “patient comfort level”, ie, a subjective evaluation of acceptable inflation levels. Some cushions, such as the Ease Seating Systems (EASE Seating Systems, Paradise, California) can be tailored to individual requirements by adjusting cell layout. However, there is limited biofeedback or ability to vary factors such as cycle duration. Further research is needed to validate the efficacy and ease of use of dynamic wheelchair cushions before they can be universally accepted as a cost-effective approach to pressure ulcer prevention.
Individuals who are able to perform pressure relief maneuvers often find it difficult to adhere to a regular 20-minute regime, particularly when they have an active lifestyle and may have altered sensory function. For these individuals, a pressure relief reminder device may be highly beneficial and more economically viable than a dynamic wheelchair cushion. The design of such a device has been explored in preliminary feasibility studies in which the primary challenge was the design of an appropriate pressure sensor . CleveMed (Cleveland, Ohio) has developed a patented biofeedback system, the Pressore Alert, which provides auditory or vibratory feedback to wheelchair users when pressure relief is necessary . The device is programmable and can be set up to provide stimuli at appropriate time intervals, depending on the risk status and activity level of the individual.
Conceptual
Advances in early detection of pressure ulcers
Basic research studies are expanding knowledge of pressure ulcer etiology. For example, many clinicians have experienced the pressure ulcer that seems to “appear from nowhere”; one day the skin is mildly indurated but intact and the next there is a large open wound with extensive tissue breakdown and necrosis. There has been a growing clinical consensus that not all pressure ulcers are caused by high pressures at the skin interface and that deep tissue breakdown may be a significant factor in pressure ulcer development . Several researchers have used finite element modeling and in vitro models to investigate the distribution of forces throughout the soft tissues. The research group at the Laboratory for Tissue Biomechanics and Engineering, Eindhoven University of Technology, The Netherlands has used a number of tissue muscle models to study the effects of applied strain and compressive forces on both the cellular level and on tissue constructs . These studies found that the highest forces were experienced close to the bone interface. More recently, the group found the same force distributions in an animal model . Furthermore, they found that short-term applied shear forces were much more causative of tissue damages than reversible ischemia. Animal model studies by Linder-Ganz and Geffen also concluded that internal muscle stress is required to establish new criteria for pressure sore prevention.
These findings present a challenge to the clinician whose goal is the prevention of pressure ulcer development. At this time, there are limited techniques to monitor deep tissue viability. Any procedure to monitor tissue health to prevent pressure ulcer development would require regular assessment, ideally daily and at least weekly. Furthermore, at-risk individuals should be able to carry out the procedure with minimal disruption to their activities of daily living. Advanced imaging techniques, such as magnetic resonance imaging (MRI), have been used in research studies . However, MRI evaluations clearly cannot meet the goals of a pressure ulcer prevention monitoring procedure. Daily, or even weekly, MRIs would be impractical and prohibitively expensive both for the health care system and the patient; indeed, in this scenario the cost of prevention may be greater than the cost of treatment.
The idea of nanotechnology was first introduced in the late 1950s by the renowned physicist, Richard Feynman . Briefly, the concept is that of devices and materials being developed on the molecular scale, ie, of the order of 10 −9 of a meter or 1 nanometer (nm). The associated field of microelectromechanical systems (MEMS) addresses the development of devices and materials with size from 10 −6 of a meter (1 μm) to 10 −3 of a meter (1 mm). Development in these fields has accelerated since the discovery of unique materials such as carbon nanotubes (buckytubes) and buckminsterfullerene (buckyballs). MEMS technology is moving out of the basic research laboratories and into mainstream application, such as automotive sensors and computer printers. In the medical field, BIOMEMS applications being developed include disposable blood pressure sensors and drug delivery systems.
Advances in the field of nanotechnology introduce the possibility of developing microscopically small devices. Nano devices, or nano-device arrays, could be implanted in the deep tissues of the high-risk individual with minimal disruption to the existing environment. These systems could provide real-time, in situ monitoring of biomechanical variables such as applied normal and shear forces, together with biochemical measures, such as temperature, pH, or lactate.
Other researchers have been investigating the role of biochemical indicators as precursors of pressure ulcer development. Bader and his group investigated early changes in the sweat metabolism of at-risk individuals during prolonged loading . In their studies, a method for collection of sweat samples at discrete intervals was developed. Advances in the field of biosensors introduce the possibility of wearable devices for continuous monitoring. This approach is already being explored by the BIOTEX Project of the Sixth Framework Program of the European Commission . The project goals include the development of a sensing patch on a textile substrate. The development of a smart textile for use in wheelchair or mattress covers would seem to be a highly attainable goal within the next 5 to 10 years.
Treatment of pressure ulcers
Current state-of-the-art methods
Novel treatment modalities: negative pressure wound therapy
Negative pressure wound therapy (NPWT) is based on the theory that the negative pressure generated drains wounds of exudates and enhances wound healing through a number of mechanisms . More specifically, NPWT is proposed to decrease bacterial load and edema while concurrently promoting and improving local circulation and increasing granulation. The technique is also known as “subatmospheric pressure therapy,” “vacuum sealing,” “vacuum pack therapy,” and “sealing aspirative therapy.”
NWPT devices consist of a suction pump with foam and occlusive dressing to create negative pressure on the wounds that they are treating. The most common known NPWT device is probably “Vacuum Assisted Closure” (V.A.C.®), which was trademarked by Kinetics Concepts, Inc., San Antonio, TX (KCI) in 1997.
Although there are currently no official guidelines on the use of NPWT, the manufacturers have provided clinical guidelines for the use of the V.A.C.® device , and there have been recent consensus reports by Sibbald and colleagues and Gupta . The primary recommendations of these reports are that NPWT is indicated under the following clinical criteria:
- •
Anatomic surfaces that allow a tight seal.
- •
Adequately prepared wounds, eg, debrided, free of eschar and necrotic materials.
- •
Wound drainage.
- •
Patient compliance.
NPWT is contraindicated when wounds are dry, there is uncontrolled pain, there is untreated infection or malnutrition, or there is poor hemostasis.
Although there is no official guideline on NPWT device settings, the consensus reports recommended a negative pressure of 75 to 125 mm Hg. The precise pressure setting is dependent on the wound condition and the level of coexisting pain; it is recommended that a lower pressure be used if pain is an issue. Negative pressure should be applied continuously for the first 48 hours followed by intermittent negative pressure thereafter (5 minutes on, 2 minutes off). Effective NPWT will produce a response within 2 to 4 weeks. Discontinuation is recommended if there is less than 30% wound size reduction after 4 weeks.
Despite its popularity, none of the major clinical reviews and guidelines has found sufficient scientific evidence to support the use of NPWT for wound healing. Over the period from 2000 to 2006, meta-analyses of clinical studies of NPWT have been performed by the Agency for Healthcare Research & Quality (AHRQ) , the Cochrane review , the Ministry of Health and Long-term Care of Ontario , the McGill University Health Center , and the PVA Consortium Clinical Practice Guideline panel . There were several common reasons that these reports did not support the scientific basis of NPWT. It was universally found that there were too few randomized, controlled trials for NWPT. In addition, both small sample size and poor study design limited the validity of theses studies. Further research is needed to determine the utility of NPWT as a treatment modality for some nonhealing pressure ulcers. Currently, judicious use of NPWT should only be considered when performed under the auspices of the consensus reports discussed above.
Novel treatment modalities: pulsatile lavage therapy
Hydrotherapy is one of the two modalities recommended by the Agency for Health Care Policy and Research (AHCPR) for pressure ulcer management . It is particularly helpful for cleansing and debridement of stage III and IV wounds. Conventionally, hydrotherapy for pressure ulcer management has been performed through the use of a whirlpool. However, the whirlpool has been found to have some clinical and practical limitations. Specifically;
- •
Cross-contamination between patients may occur, with multiple cases of pseudomonas infections being reported in the literature .
- •
The pressure jets may not be directed specifically at the pressure ulcers, thus the exact pressure applied to the wounds is not known.
- •
The cleansing and sterilization procedure may be rather cumbersome.
- •
Skin infections are potentially hazards for caregivers who are in contact with the contaminated water.
Other important issues are specific to individuals with spinal cord injury:
- •
It is very labor intensive to transfer the spinal cord–injured individuals with limited mobility into and out of the whirlpool.
- •
The sensory impairment in these individuals may result in burn injury if the water temperature is too high.
- •
Submersion into the whirlpool may affect body temperature control, especially for those with a higher level injury.
Therefore, despite the effectiveness of whirlpool therapy, it may not be ideal for use for individuals with spinal cord injury.
Pulsatile lavage therapy is a different form of hydrotherapy that encompasses all of the advantages of whirlpool therapy but without the potential adverse effects. A portable device is used that delivers pulsed jet streams of water at a known, preset pressure, which is compliant with the pressure range (4 to 15 psi) recommended for wound cleansing . The device is for single-patient use only and is applied over the pressure ulcer, with the jet streams of water aiming directly into the wound bed through a soft, fan-spray tip. Some models also have concurrent suction that takes the soiled fluid back into a sealed collection canister, thus eliminating any significant spillage around the treatment area. The potential for cross-contamination between patients is eliminated because the device is for single-patient use and is used by a caregiver in the patient’s room. In addition, there is no risk of any skin infection for the caregiver, provided that appropriate protective garments are being worn. However, the use of pulsatile lavage for multiple patients in the same location, without limiting the equipment for single-patient use, may lead to adverse outcomes with cross-contamination . Because the treatment is localized to the wound area and uses a room temperature fluid, there is no risk for burn injury or any temperature dysregulation. Furthermore, pulsatile lavage therapy is less labor intensive than whirlpool hydrotherapy because it does not involve any transfer, and there is no cleansing of equipment afterward.
These factors also make pulsatile lavage appropriate for pressure ulcer debridement for home use . Therefore, pulsatile lavage appears to be a preferred alternative to whirlpool therapy in the management of pressure ulcers. The clinical efficacy of pulsatile lavage in the treatment of pressure ulcers is currently under investigation.
Advances in pressure ulcer assessment: the use of telehealth for pressure ulcer management
The outpatient evaluation and monitoring of pressure ulcers in persons with spinal cord injury can be rather challenging at times because of the limited availability of appropriate transportation and poor pressure relief surface options while the individuals travel to see the evaluating clinician. The process of traveling to a clinical appointment could ironically pose more harm to the pressure ulcers to be evaluated. This process can present a dilemma to the clinician, who needs to balance the benefits of a pressure ulcer evaluation against the potential adverse effects of travel.
With the advances in technology, telehealth is becoming increasingly common and can provide us with the means to evaluate and monitor patients with pressure ulcers , while eliminating the need for long-distance travel. Telehealth is defined as long-distance communication between the patient and the health care provider via electronic means, such as video and audio. Studies have found that telehealth can provide accurate evaluation of wounds . Telehealth can be used for pressure ulcer management and may be applied as home-based telehealth or clinic-to-clinic telehealth. In each case, the data delivery may be done immediately (“real-time”) or be obtained and then delivered at a later time (“store-and-forward”). Both real-time and store-and-forward telehealth programs have been found to be accurate, although there is trade-off between cost and efficiency; the real-time system is more expensive to set up but clinically more efficient, whereas the store-and-forward system is less expensive to set up but less efficient .
Home-based telehealth can be used for the management of pressure ulcers by the transmission of digital images from the patient’s home to the clinician’s office, either through the use of a real-time video camera or through store-and-forward digital photography . High-definition wound images can be sent over a regular telephone line, the internet , or even a wireless telephone . For spinal cord–injured individuals, this may require the assistance of the caregivers to capture images and transmit them from home. In such cases, training of the caregiver will be necessary. Depending on the system and equipment used, there may or may not be direct interaction between the patients at home and the clinician in the clinic. The resolution of the images depends on the transmission speed of the equipment as well as the quality of the imaging device. There are currently no established standards for home-based devices and appropriate transmission speeds for the reliable evaluation of pressure ulcers using telehealth.
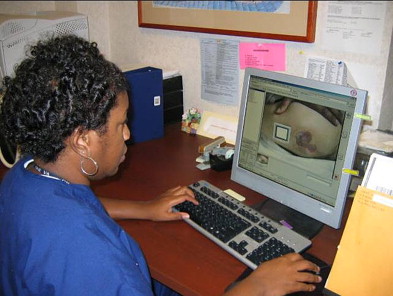
Clinic-to-clinic telehealth can provide subspecialty evaluation of pressure ulcers from one clinic to another . The patients at the referral site are able to directly interact with the consultant through the real-time video. In addition to providing direct evaluation of pressure ulcers, clinic-to-clinic telehealth can also provide the means by which long-distance evaluation of other factors that affect pressure ulcer healing, including interface pressure measurement by pressure mapping, and seating or wheelchair evaluation. Our clinic at the Louis Stokes Cleveland DVA Medical Center has designed a dual screen system with one screen showing the posture of the patients at the referral site, while the other screen provides live data of pressure mapping from the referral site ( Fig. 2 ). The clinic personnel at both the referral and consulting sites require training for the operation of the equipment, and a high-speed internet line is essential to provide high-resolution images and video. Using the clinic-to-clinic telehealth system, comprehensive pressure ulcer evaluations can now be done with the patients attending the local primary care clinic that would otherwise not have the special expertise for pressure ulcer management. Just as with home-based telehealth, there are currently no standards for devices and communication protocols to be used for clinic-to-clinic telehealth.

Using both home-based and clinic-to-clinic telehealth systems, pressure ulcers can be effectively and comprehensively managed over long distances. Participating patients no longer have to travel long distances for subspecialty care, thus improving the access to care for spinal cord–injured individuals and avoiding any high costs associated with long distance travel. In addition, telehealth can provide educational training and help standardize care across a large geographical area united by a single telehealth network. It also enables the clinicians to provide teleconsultations to more patients than without the use of telehealth . Currently, telehealth is not the standard of care in most geographical areas; however, it is expected to gain popularity as the technology becomes more affordable and available. The future growth of telehealth will be critically dependent on the resolution of important issues such as data security duration transmission and medicolegal concerns .
Advances in pressure ulcer assessment: the use of digital measurement techniques
Accurate wound measurement is of utmost importance in the monitoring and outcome evaluation of pressure ulcers in both clinical care and research. Over the last decade, wound evaluation tools have been developed that combine subjective assessment with wound size measurement . A recent survey found that the majority of the surveyed clinicians felt that improvement is possible in the objective measurement of wound size . Conventionally, linear measurements of length, width, and depth have been used widely in clinical care. However, this may not provide the most reliable evaluation, especially for pressure ulcers that are large, deep, and irregular in size and shape. Linear measures also tend to overestimate the surface area . Furthermore, the linear measurements may have low interrater reliability. Assessment of wound healing over time incorporating repeated clinical evaluation together with reliable objective quantification of wound dimensions is essential to evaluate both current standards of care and new therapies. Therefore, alternative wound measurement methods that provide high accuracy and good interrater reliability would be very desirable. Digital wound measurement devices can potentially have these qualities that would be helpful in both the clinical and research settings.
Chronic wounds of varying etiologies can be highly variable in appearance and size. The ideal wound measurement technique would be able to accurately define the size of any wound, no matter what its depth, surface area, location, or the extent of undermining or tunneling. Critical geometric variables that could fully describe the wound “space” include maximum linear dimensions (length, width, and depth), aspect ratio, and circumference. In addition to providing an index of wound size, quantitative techniques must be reliable, repeatable, sensitive, and valid. The technology used must be robust and safe for both patients and clinical staff, cause no pain to the patient, and produce minimal additional disruption to ongoing care.
Two digital imaging techniques that have recently been introduced for clinical use may provide increased accuracy in determining linear wound dimensions and surface area. The Visitrak (Smith & Nephew, Largo, Florida) system represents a planimetry approach and requires wound contact for measurement. The VeV MD (Verge Videometer Measurement Documentation) system (Vistamedical, Manitoba, Canada) is a digital image analysis technique with photogrammetry that requires no contact for wound surface area measurement.
Visitrak is a tracing measurement technique that uses a transparent tracing film and a calculation tablet. The transparent, thin, flexible plastic sheet is placed over the wound area, and the outline is traced manually by the clinician using a permanent marker. The transparent film is then retraced on the Visitrak tablet. The Visitrak software then calculates the maximum length, width, and surface area of the traced wound automatically. Good inter- and intrarater reliability has been shown with this technique .
The VeV MD system is a noncontact technique based on the use of digital image analysis. It requires a digital photo of the wound with a standard target plate of known size to be placed next to the wound. After the images have been uploaded onto the computer, the outline of the wound’s digitalized image is then traced manually by the clinician on the computer monitor. This area subsequently is compared with the adjacent standard target plate by the program’s software, automatically calculating the surface area of the wound ( Fig. 3 ). This measurement software has been used for the evaluation wound size in research studies .