The Posterior Approach to Revision Total Hip Arthroplasty
David W. Manning
Samer Attar
Case Presentation
A 44-year-old woman was referred for evaluation of a painful right hip 2½ years after staged bilateral hip replacements. The left hip was performed first and is without complaint. The right hip, performed 2 months later, has always been painful in the groin and buttock. Her pain is worse with activity, and has increased over time. In addition to pain, she complains of a limb length inequality with the right limb being longer. The limb length complaint is so severe that she wears only one shoe when she is at home.
Her physical examination shows a well-healed mini posterior-lateral incision, a full range of motion to the hip in the supine position, and normal neurologic and vascular examinations. During side-lying abduction, her muscle strength is graded as five out of five. She walks with an antalgic and vaulting gait on the right. On forward bending it is noticed that the patient has a subtle scoliosis that is well balanced at the shoulders but the right-sided iliac crest and posterior spine are elevated. Using blocks it is measured that the apparent limb length inequality is 0.5 in with the right leg being longer.
Radiographs of the pelvis and hips show bilateral uncemented arthroplasties with fine radiolucencies about the right acetabular implant in all three Delee–Charnley zones (Fig. 101.1) (1). The limb length inequality measured on the AP pelvis is less than the clinically apparent limb length inequality. She has a normal C-reactive protein and erythrocyte sedimentation rate. The diagnosis of aseptic loosening of the right acetabular component and clinically significant limb length inequality was made and a revision planned via the modified posterior-lateral approach (Table 101.1).
Overview and Indications
The modified posterior-lateral approach to the hip is a combination of the original descriptions of Langenbeck in 1873 and Kocher in 1887 (2,3,4,5). The original works were intended to describe posterior exposure to the hip and surrounding tissues for the treatment of tuberculosis, sepsis, tumor, and trauma. The advantages were reported to include ease of surgical approach and the maintenance of the gluteus medius and minimus insertions to the greater trochanter. It was not until 1954 when Marcy and Fletcher reported using the posterior-lateral approach for inserting a femoral head prosthesis that the approach began being used for arthroplasty purposes. The approach has been subsequently modified by several authors including Judet and Harris, but the key features originally described in the late 1800s are what make the surgical approach utilitarian. Thus, the modified posterior-lateral approach is most commonly referred to as the Kocher–Langenbeck approach. Indeed, it is the ease of surgical approach and the maintenance of abductor insertion as originally described, along with the extensile nature
of the approach, which make the modified posterior-lateral approach to the hip a workhorse in revision hip arthroplasty surgery (2,3).
of the approach, which make the modified posterior-lateral approach to the hip a workhorse in revision hip arthroplasty surgery (2,3).
Table 101.1 Surgical Approaches in Revision Hip Arthroplasty | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The modified posterior-lateral approach to the hip attains excellent exposure to the entire posterior column of the pelvis, the posterior two-thirds of the iliac wing, the posterior wall, and weight-bearing dome of the acetabulum, and the entire femur (2,3). As such, the approach is frequently used in revision arthroplasty surgery of the acetabulum, femur, or both. The exposure allows for complex pelvic work such as posterior column plating, structural acetabular bone grafting, metallic acetabular augment placement, acetabular cage reconstruction, cup-cage constructs, and even custom triflange and saddle prosthese reconstruction of the hemipelvis (6,7). In fact, much of this complicated pelvic work can be performed through the modified posterior-lateral approach while maintaining the abductor insertion on the greater trochanter and without removing a well-fixed femoral implant. Additional exposure to the pelvis can be created by employing a greater trochanteric osteotomy and reflecting the muscle, tendon, and trochanteric bone flap proximally and anteriorly (2,3). With respect to the femur, the approach affords excellent top-down exposure for removal of loose femoral implants, simple cement mantles, and proximally ingrown femoral implants. The distal extension of the femoral limb of the exposure is simply a lateral approach to the femur and can be used in cases necessitating extended trochanteric osteotomy, femoral window creation, as well as the management of periprosthetic femoral fracture, proximal femoral replacement, proximal femoral allograft prosthetic composite reconstruction, and even total femur replacement.
The applied anatomy of the proximal limb of the modified posterior approach to the hip can be thought of in three layers. The superficial anatomy of the approach includes the gluteus maximus and the iliotibial band (ITB). The skin incision is typically oriented over the lateral aspect of the femur and curving proximally over the greater trochanter and along the anterior border of the gluteus maximus near its apposition to the tensor fascia muscle (Fig. 101.2). The ITB is incised in line with the skin incision and carried proximally through the superficial fascia of the gluteus maximus, allowing the muscle to split in line with its fibers close to the boundary with the tensor fascia muscle (Fig. 101.3). Because the gluteus maximus muscle receives its innervation from the inferior gluteal neurovascular bundle posteriorly on its deep surface, little muscle is at risk for denervation.
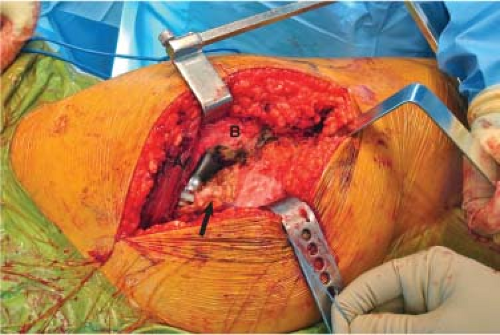
The gateway to the hip through the posterior-lateral approach is the posterior border of the gluteus medius, which is the second layer of the proximal limb of the approach. Simple anterior retraction of the posterior border of the gluteus medius allows for identification of the deep layer, the piriformis,
the remainder of the short external rotators of the hip and the joint capsule. The hip is exposed once the deep layer is dissected from its insertion on the intertrochanteric line of the femur (Fig. 101.4).
the remainder of the short external rotators of the hip and the joint capsule. The hip is exposed once the deep layer is dissected from its insertion on the intertrochanteric line of the femur (Fig. 101.4).
The proximal limb of the approach is extensile to the posterior crest of the pelvis by simply splitting the gluteus maximus proximally and mobilizing the gluteus medius and minimus anteriorly and proximally. The gluteus medius and minimus receive innervation and blood supply from the superior gluteal nerve and vessels, which exit the greater sciatic notch. These structures are tethered at the sciatic notch and are at risk for injury when elevating the medius and minimus muscle bellies to expose the lateral ilium proximal and posterior to the acetabulum. Extensive mobilization of the gluteus medius and minimus necessitates care and may be best performed with a greater trochanteric osteotomy to relieve tension on the superior gluteal nerve and vessels. The sciatic nerve is also at risk during this approach but lies posterior to surgical field and can be palpated to prevent injury (8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree