Fig. 3.1
A 9-year-old child sustained a lower leg and femur fracture on the right side; both fractures were aligned and the original leg length was achieved. Despite a short healing time and no remodeling it came to an over growth of 3 cm over the next 5 years
In addition, healing time varies with age. Consequently, the period of immobilisation differs. Below the age of 10 years, 3–4 weeks of wearing a cast is sufficient in almost all cases. However, above 10 years, 5–6 weeks of immobilisation is often necessary.
In addition to that the above, fractures-types are age-related. This phenomenon is because of the typical physical properties of the bone, periost, and cartilage at that age.
Development and Growth
The immature bone is not only more capable of reaction and adaptation, but also more vulnerable than the mature bone. A fracture in an immature bone can cause growth to speed up or slow down, superimposing the problems of deformity on the complications of the fracture itself.
On the other hand, children’s fractures heal very rapidly and, depending on the age of the child and direction of the deformity one can remodel by correcting the most angular malunion. The most important area of injury in the immature skeleton is the growth plate or physis.
Regulation of Epiphyseal Growth
The physis is the primary center for growth in most bones and may be divided into two zones according to their function: the zone of growth and the zone of matrix formation. The zone of growth is involved with both longitudinal and circumferential growth of bone. The physis is capable of responding to different stimuli, either compression or tension.
Any kind of stimulation of the circulation leads inevitably to a stimulation of the growth zone, and therefore, of the growth. It was believed earlier that fractures would heal with shortening so that the bone has the same length at the end of the treatment. This shortening was inaccurate as it was not possible to calculate it correctly. On the other hand an anatomical reduction and osteosynthesis in most cases leads to a lengthening (Fig. 3.1). We know today that the stimulation of growth is a result of the healing time and remodeling time. We achieve the best results if we have a biological treatment and fixation, which anatomically adapts the bone fragments, has a short healing time, and no remodeling needs. This biological principle is put into effect with the ESIN technique as the best one.
Growth and Remodeling of the Metaphyseal and Diaphyseal Bone
The metaphysis is the site of the most rapid changes in bone structures as the deeper physeal zones mature and the physis produces primary trabecular bone.
The circumferential growth of the diaphysis is a function of appositional bone formation by the periostium, together with osteoclastic resorption by the endosteum so as to enlarge the medullary cavity. As growth continues, the bone is capable of reducing, or even correcting, angular deformity by selective resorption and apposition, possibly driven by forces of compression and tension (Table 3.1).
Table 3.1
Place of correction, factors and possibilities of the growing skeleton
Displacement/deformity | |||
Side to side | Axial (frontal–/sagittal plane) | Shortening/lengthening | Rotational failures |
Periosteal–endostal | epiphyseal | ||
Direct correction | Indirect correction | ||
Healing Time based on Patient Age
In addition, healing time varies with age. Consequently, the period of immobilisation differs. Below an age of 10 years, 3–4 weeks of wearing a cast is sufficient in nearly all cases. However, above 10 years, 5–6 weeks of immobilisation are often indispensable. But we must also consider the weight of the child.
Further, fracture-types are age-related. This phenomenon is because of the typical physical properties of the bone, periost, and cartilage in children.
The factors mentioned above determine the degree of tolerable dislocation and the choice of treatment. With rising age the option of conservative treatment declines and that of osteosynthesis increases.
In childhood especially, K-wires with an additional cast, cannulated screws, intramedullary elastic nails, and adapted external fixators are suitable implants. Plate osteosynthesis is exclusively used in adolescents, as also in adults. Solid intramedullary nails should be avoided in children (Table 3.2).
Table 3.2
Guidelines for fracture immobilization in childhood (weeks)
<5 years | 5–10 years | >10 years | |
|---|---|---|---|
Clavicle | 1 | 2 | 2–3 |
Humerus | |||
Proximal stable | 1 | 2–4 | 3–4 |
Proximal unstable | 1 | 2–4 | 3–4 |
Humerus shaft | 2–3 | 3–4 | 4–6 |
Supracondylar | 2–3 | 3–4 | 4–5 |
Radial condyle | 3 | 3–4 | 4 |
Ulnar condyle/Y fracture | 2–3 | 3–4 | 3–4 |
Ulnar epicondyle (+ dislocation of the elbow) | 2–3 | 2–3 | 4 |
Radius proximal | 1–2 | 2–3 | 3–4 |
Olecranon | 2 | 2–3 | 3–4 |
Forearm shaft incl. Greenstick fracture | 3 | 4 | 4–6 |
Radius (+ radius + ulna) distal | 2–3 | 3–4 | 4–5 |
Salter Harris I radius distal | 2 | 2–3 | 3–4 |
Carpus | 4–6 | 5–8 | |
Metacarpal proximal and distal | 2–3 | 3–4 | |
Metacarpal shaft | 3–4 | 4–6 | |
Fingers proximal and distal | 1–2 | 2–3 | 3–4 |
Fingers shaft | 2–3 | 3–4 | 4–6 |
Femur | |||
Neck of the femur | 4–6 | 6–8 | |
Subtrochanteric fractures | 2–4 | 4–5 | 5–6 |
Shaft | 2–3 | 4–5 | 4–6 |
Distal | 2–3 | 3–4 | 4–5 |
Tibia and lower leg | |||
Tibial spine fracture | 3–4 | 4–6 | |
Proximal metaphysis | 2–3 | 3–4 | 4–5 |
Shaft | 2–3 | 3–5 | 4–6 |
Distal and malleolar | 2–3 | 3–4 | 4–5 |
Hindfoot and calcaneus | 4–6 | 5–10 | |
Midfoot and toes distal | 2–3 | 3–4 | 4 |
Toes | 1–2 | 2–3 | 3–4 |
Fibulo—talar ligaments/osseous avulsion | 3–4 | 4–6 |
Table 3.3
Overview of the influence of these three factors (localization/displacement/stability) regarding therapeutic options
Stability | Bone/segment | Therapy |
|---|---|---|
Sufficiently stable for safe reduction and initial retention | Diaphyseal/metaphyseal | Immobilization with plaster of Paris, e.g. in combination with cast wedging |
Transverse fracture with tolerance limits depending the age | Fiber-glass cast | |
Or | Standardized produced splints | |
Oblique or spiral fractures only of one bone of the lower leg or forearm | ||
Articular | ||
Non or minimal (<2 mm) displaced articular fractures | ||
Unstable fractures (not reducible and not to stabilize with non-operative treatment) | Diaphyseal/metaphyseal | Reduction under anaesthesia is indicated |
All fully displaced fractures | Conservative (plaster cast) or operative stabilization is necessary | |
Articular | ||
Articular fractures with a gap over 2 mm |
Patient’s Body Weight
In childhood, absolute stability of the fracture is not necessary, neither following surgical treatment nor after conservative treatment. The reasons for this have been discussed in the previous section. In most cases, relative stability is sufficient for immobilisation and progressive weight bearing. However with increasing age, biomechanical limits are noticed. The key influence is not age itself, but the tendency toward increased body weight and size that can be observed. Frequently, 12–14 year old children are as tall and have the same body weight as adults, which is often associated with overweight, today. Little attention has been paid to this observable fact in the current literature on pediatric traumatology. Nevertheless, therapy planning has to integrate these aspects as the clinical impact is of major concern. Therefore, in older children who are also heavier, therapy should be provided as provided to adults after fracture- treatment, particularly in shaft-fractures (Fig. 3.2).


Fig. 3.2
A 13-year-old boy, overweight with unstable fracture of the lower leg. Osteosynthesis with ESIN, insufficient stability because of fracture type and the weight despite additional stability by an interlocking screw; so called “miss–a–nail” technique
Fracture Pattern
Fracture morphology has a decisive influence on therapy, independent of the age or physical development of the child. The stability of the fracture is of primary interest. Then the completeness of the fracture is evaluated.
The recognition of a so-called “bowing-fracture” is of particular importance. This type of injury is subject to laws of its own. Bowing fractures show progressive angulation and possess only little potential for remodelling. In particular, at the forearm, where this fracture is frequent in young children, there is a good chance of ending up with bad functional results after conservative therapy (Fig. 3.3). The current treatment of choice is ESIN (elastic stable intramedullary nailing). The inserted nail equalizes the angulation of the bone with its own opposite curvature, which was applied to the nail before insertion. Further angulation is thereby prevented.
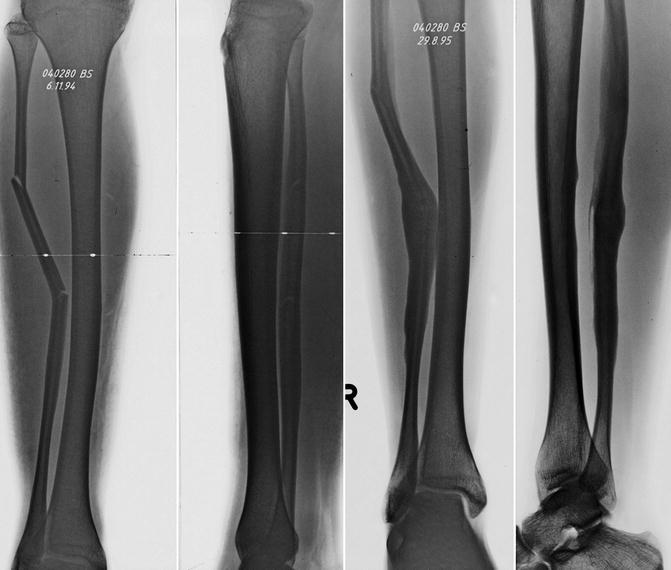
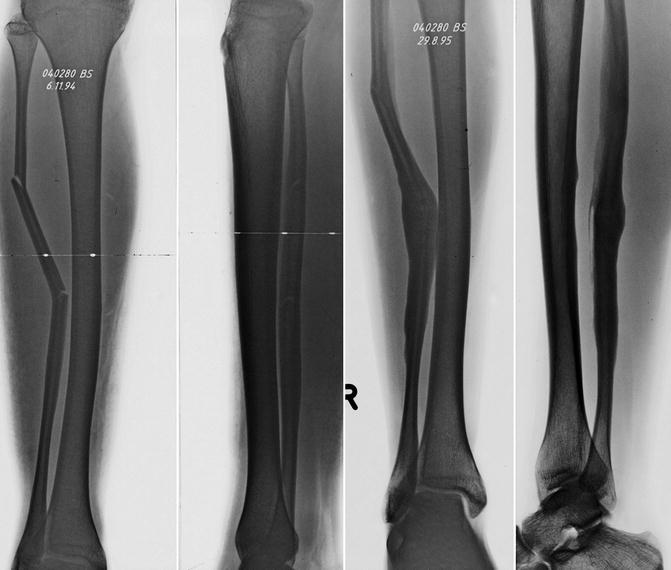
Fig. 3.3
Direct lower leg trauma in a 15-year-old boy with “bowing” fracture of the tibia. The x-rays show a malunion 8 months after this “bowing fracture” of the tibia (still remaining bowing)
Nonetheless, for the most part, stable fractures are treated conservatively with a cast independent of the patients age. Healing of the bone occurs quickly and without problems. Immobilization between 3 and 5 weeks is nearly always sufficient. An exception is the fracture of the femoral shaft which is treated with ESIN or external fixator in most centres.
In the case of unstable fractures one should always be prepared for an operation. Even if the initial reposition of an unstable, dislocated fracture is successful, secondary dislocation may require a change from conservative to surgical therapy (Table 3.3).
Repetitive reductions or manipulations in the treatment are to be avoided. Considering the type of the fracture, the following rules should be taken into consideration:
If general anaesthesia for reduction of a fracture in childhood is indicated, we aim at a definite, stable, and safe fixation; i.e. potentially unstable fractures will be reduced in the operation theatre with the option of an eventual operative treatment.
Independent of the age of the child, totally unstable fractures are operated primarily.
If general anaesthesia is required, the first treatment has to be the definite treatment; no second anaesthesia.
Because the fracture type has a direct influence on the therapy, it is important to classify the fractures correctly (Table 3.4). One of the most recognized fracture classifications is the AO/OTA today (Pediatric Comprehensive Fracture Classification of Long Bones; PCCF). See chapter appendix (below) and Table 3.5.
Table 3.4
Overview of the influence of localization and the involvement of the physis regarding therapeutic options
Fracture localization | Stability | Morphology | |
|---|---|---|---|
Shaft fracture | Diaphyseal fracture | Stable fracture | Not displaced fractures without shortening |
Unstable fracture | Displaced fractures with shortening or the tendency for shortening or angulation | ||
Greenstick fracture | Bowing fractures with complete fracture of one cortex and incomplete facture of the opposite cortex | ||
Metaphyseal fracture | Buckle fracture | Compression of the metaphyseal cortex of one side | |
Bowing fracture | Greenstick fracture in the metaphysic | ||
Supracondylar fracture | Ligament avulsion | ||
Ligament avulsion | |||
Articular fracture | Epiphyseal fracture | Aitken I | See below |
Salter I, II | See below in the puberty, partial closed physis bony or cartilage avulsion “normally” in combination with joint dislocation | ||
Aitken II + III | |||
Salter III + IV | |||
Fractures of Tillaux or two planes fractures | |||
Lig. Avulsion | |||
Flake fracture |
Table 3.5
The Salter-Harris classification in comparison to the Aiken classification
Salter | Aitken | |
|---|---|---|
I | (a) Epiphysiolysis | I |
II | (b) Epiphysiolysis with metaphyseal wedge | |
III | (c) Epiphyseal fracture | II |
IV | (d) Epiphyseal fracture with metaphyseal wedge | III |
V | (e) Epiphyseal compression (only seen “post festum”) |
Table 3.6
Overview of the sign/treatment and outcome of clavicle fractures
Morphology | Fractures of the mid-shaft are most common and range from greenstick to complete fractures |
|---|---|
Signs | Pain, swelling, painful movement of the arm |
Diagnosis | Clinically and radiologically |
Correction potential | Good |
Complications | Nerve problems, non-union, cosmetics |
Nonoperative therapy | In principle non-surgical – sternal brace or “figure-of-eight” bandage pulling the shoulder backwards (pain management) |
Operative treatment | Only fully displaced, comminuted fractures in adults (author’s preferred method is ESIN) |
Immobilization | 2–3 weeks |
X-ray control | After 3 weeks |
Follow-up | Only clinically |
On the other hand we have to take into account different factors of the fractures as well as the localization/displacement and stability for a correct therapeutic decision.
Bone and Segment
In addition, localization influences the choice of the treatment. The management is different if the lower or the upper extremity is involved. In childhood, even more important is the localisation of the fractured segment: diaphysis/metaphysis or epiphysis.
Although in diaphyseal fractures, stability has a decisive influence on therapy, in epiphyseal and some metaphyseal fractures, the extent of displacement of the fragments is crucial.
Epiphyseal fractures are special in two ways. On the one hand it’s an injury of the growth plate with a possible impairment of the growth; on the other hand these are always injuries of the joint with all the difficulties of this type of injury. In principle, articular incongruency has to be redressed, and interfragmentary gaps up to 2 mm can be accepted. This proceeding has not been established by scientific evidence, but justified following observations and evidence.
In these fractures, the suitable implants are cannulated screws and K-wires of all sizes. In some articular fractures, as for example the two-plane fracture of the tibia, screw fixation allows a closed procedure.
The potential for remodelling of a facture is strongly influenced by the segment involved. Knowledge of the prevailing potential for remodelling is an indispensable requirement for treating pediatric fractures (Fig. 3.4).


Fig. 3.4
Sometimes the “expected/normal” healing does not following the natural laws. Simple metaphyseal, nearly not angulated radial fracture fixed in a plaster cast. Six months later well healed but increasing angulation and deformation is growing proximal. Because of wrist pain the child came back 3 years later. A severe dorsal tilt of the wrist (35°) and “bayonet” malunion is clearly seen on the normal x-ray and CT scan
Metaphyseal fractures of the proximal humerus and the distal forearm have to be emphasized. As the corresponding epiphyseal plates are responsible for a major part of the length growth of these bones, remodeling has the highest capacity at this place. For this reason, fractures involving the proximal humerus or distal forearm are treated conservatively for the most part, even in older children.
Independent of the localisation of the fracture, side-to-side (so called bayonet displacement) is corrected better than axial deviation.
Adequate, correct diagnostic: Skeleton standard x-rays and special radiological examinations (Ultrasound/CT/MRI)
Even in an emergency the correct AP and lateral (at least +/− perpendicular each-other) x-rays should always be taken.
General notes to the fracture types:
Not every fracture is visible on the x-ray in childhood
An x-ray is always indicated if the patient history/local signs or injury is unclear.
If the decision for an x-ray has been made, then it should also provide the desired information; in other words we need good quality.
It is absolutely necessary to take x-rays in two planes (perpendicular to each other). Moreover the proximal and distal joint of the broken segment should be visible on the x-ray.
The x-ray of the opposite extremity is unnecessary as no new knowledge will be obtained.
Remember, you can see only what you know.
The evaluation and correct assessment of an x- ray is the prerequisite for correct diagnosis. The diagnosis, therefore, represents the base of the therapy decision. The phenotype of the childlike skeleton changes from year to year, sometimes from month to month. Therefore, the exact age-related development of the child’s skeleton is important. Growth plates are very often missing—interpreted as a fracture. This often leads to non-indicated treatment. The most frequent and typical example of this is the misinterpretation of the three-dimensional form of the proximal physis of the humerus. The following table gives a summary overview of the age dependent skeleton development of the most frequent miss-interpreted skeletal regions.
On x-ray, children’s joints seem much larger than they really are (Fig. 3.5). The reason for this is the thick cartilage around the epiphysis.
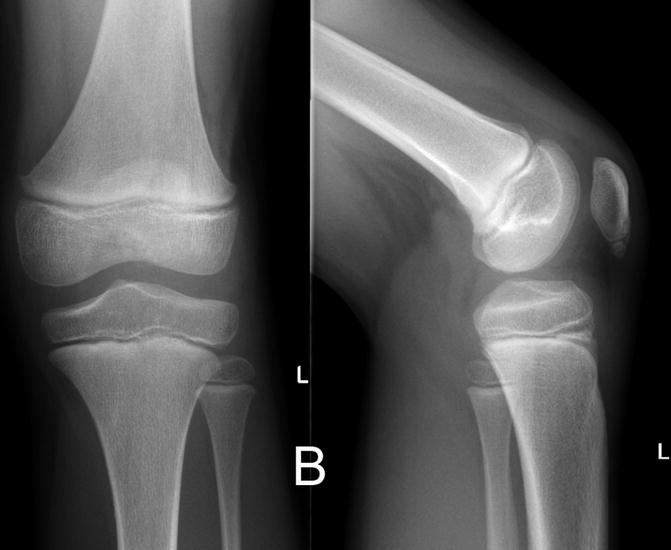
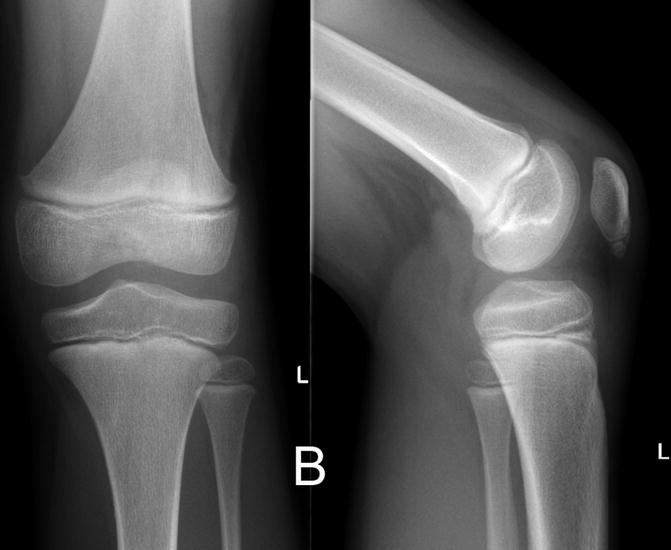
Fig. 3.5
X-ray shows typical radiological situation of knee joint in a 6-year-old girl
Treatment Options: Non-operative Versus Operative
To decide between conservative and surgical therapy, the four previously discussed criteria are to be taken into consideration. Experience shows that quite often all aspects of a fracture are not considered in the decision for the therapy.
The choice of operative or conservative therapy has to be based on the main goal of the treatment. Despite the fact that the treatment should be definite, an initial cast-immobilisation of a potentially stable fracture is legitimate if general anaesthesia is avoided. Radiological follow-up after 5–7 days is imperative. If progressive displacement is observed, definitive treatment is still possible, in most cases, by surgery. Outcome is not influenced negatively by a brief delay to definitive surgery.
For example, in lateral condyle fractures of the humerus, the arm is primarily immobilized if the interfragmentary gap is equal or below 2 mm. After 5–6 days, a radiological control without cast is performed. If the position of the fragments remains unchanged, cast immobilisation is continued. In the case of displacement above the tolerable limit, the radial condyle is fixed operatively (Fig. 3.6).


Fig. 3.6
Lateral condyle fracture of the humerus with displacement below 2 mm treated by cast immobilization (a). According to our recommendation after 5 days a cast free x-ray was made and shows a secondary displacement more than 2 mm (unstable situation). This is the indication for operative fixation (b). Correct K-wire fixation one parallel to the joint, one in the lateral column (c)
Modality of Surgical Treatment
In addition to the theoretical knowledge required for the treatment of pediatric fractures, certain technical prerequisites are necessary, especially with regard to surgical therapy.
In childhood, implants should be adapted to body size. As stability does not have to be as high as in adults and as additional cast-immobilisation is well tolerated, very small implants can be used, especially in epiphyseal and metaphyseal fractures. K-wires and cannulated screws are particularly suitable.
For surgical therapy of shaft fractures, the various implants should be disposable, and alternatively, the surgeon should be experienced in several techniques.
An adequate surgical setting enables changes in therapy during the operation. The following essential guidelines are commonly accepted for the surgical management of shaft fractures.
The therapy of choice for transverse, oblique, and short spiral fractures between the age of 4(/5)—14(/15) years is ESIN.
Extremely unstable fractures of the lower limbs are preferably treated with external fixators. According to the experience of the surgeon, ESIN may be suitable or a combination of both ESIN and external fixators (Fig. 3.7).

Fig. 3.7
A 14-year-old boy with cerebral palsy, previous hip and proximal femur osteotomies, osteoporotic bone sustained in a subtrochanteric transverse fracture: for alignment a closed reduction and fixation with two thin elastic nails was performed; to prevent any axial deviation and to manage the child immediately in the wheel-chair a medium external fixator was applied; removal of Ex Fix is planned when callus formation is visible
Today, osteosynthesis with plates in childhood get more and more rarity value and we see this type of fixation as a “special indication”. The main indication to use plates is older teenager and overweight children.
Personal Experience
A factor not to be underestimated is experience in the treatment of fractures in children. A retrospective analysis at our clinic of all femoral fractures treated with ESIN has shown that 75 % of all problems and complications have been caused by surgeons who had treated less than four fractures with this technique. This also points to the fact that the importance of the learning curve should not be underestimated. This also applies to smaller clinics, especially those that seldom treat children or see only few, individual special fractures per annum.
Unfortunately, this statement does not only apply to operative therapy but also applies to handling the plaster cast and to conservative therapy. Being able to make an adequate plaster cast is still a part of the high art of conservative therapy.
The analysis of the malunions and complications to be treated in the cases assigned to this clinic within the last 5 years, shows that 90 % of these cases came from hospitals which that only sporadically treat children.
Consequently, treatment of pediatric fractures should only be carried out by experienced pediatric surgeons who:
Are competent
Treat pediatric fractures regularly
Dispose of adequate equipment
Are trained in the use of the implants
Practicability of Postoperative Management
It is in the nature of children to be always moving. It represents a basic need in childhood. Infants hardly support being tied up. Respecting this condition, a worldwide change in therapy planning has taken place.
Children do not like bed rest for 2 to 3 days or weeks, or restriction using the upper extremity as for writing in school or everyday activities. Therefore such treatments (as plaster cast) should be things of the past for children. Absence from school is a major strain for children today. Apart from this, taking care of ill or disabled children is a difficult charge for young and working parents and the society (Fig. 3.8).


Fig. 3.8
Two girls, a 10-year old and a 11-year-old, with femoral fractures. Right: treatment with a modern scotch-cast/ spica-cast; Left: treatment was performed with ESIN and mobilisation on crutches on the second postoperative day
Altogether, if possible, therapy planning should take these factors into consideration. During the initial setting up of the treatment with the parents, the postoperative and post-hospital care, follow up consultations, and the effort necessary for each therapy should be mentioned.
Cost Effectiveness
Financial factors increasingly influence medical treatment, including pediatric traumatology. A trend towards surgical treatment approaches reflects this tendency in pediatric bone trauma. Today, an operative treatment with ESIN for a femur fracture for a 12-year-old child (including out-patient nail removal) at this clinic is around 1/3 of the cost of a conservative therapy by means of extension and spica cast.
The Choice of the Method of Treatment According to the Type and Location of the Fracture and the Age of the Child
Conservative Immobilization Techniques
Plaster Immobilization
As mentioned earlier, plaster treatment is at the base of the fracture treatment in children. It is therefore indispensable that for a doctor who treats children has the skills of modern plaster technology.
Plaster Splint
Indications
Fractures
Distortions
Pain after bone bruises
Technique
The extremity should be covered with a cotton tube.
It should be wrapped with thin half elastic cushion cotton.
It should be wrapped with a paper bandage (not necessary if fibrecast is used.)
Plaster gauzes should be placed longitudinally along both sides of the extremity with a 3-cm plaster-free gap between them
After oedema regression, the cast can be closed circularly.
Circular Plaster Cast
Indications
Functional treatment
Secondary post-plaster splint (after oedema regression)
Technique
Same steps as above
The extremity is enclosed in a circular plaster.
Drying time for plaster ~1.5 h; for Scotch cast ~30 min.
A primarily applied circular plaster should be opened longitudinally, especially when the tissue is swollen after fresh injuries.
When swelling subsides, the plaster can be closed again.
Plaster Cast Windows
Indications
Open wounds
Pins
K-wires
Technique
The earliest that windows can be made in the plaster is after drying.
The window in the plaster must always be covered with the piece that was taken out in order to prevent oedema in this region.
The window in the plaster must not impair the stability.
Plaster Cast Wedging
Indication
Remaining angulation of an undisplaced fracture, after fracture stabilization without reduction
Secondary angulation following plaster cast stabilization of an undisplaced fracture
Technique
The earliest the wedging of the plaster can be made is after one week after swelling and pain have completely subsided.
The cut for the wedge must be at the deepest point of the concavity of the deformity.
The more peripheral the fracture, the more proximal should be the point for the wedge.
The child should not have any pain during this procedure.
Principles of Therapy (Non-operative and Operative)
One takes into account all considerations before choosing from the following options for the therapy so:
Fixation without any manipulation
Skin (skeletal should be avoided) traction
Closed reduction and non-invasive fixation
K-wire fixation
Lag-screw fixation
Reduction and fixation by “external fixator”
Intramedullary elastic stable nail fixation (ESIN)
Intramedullary rigid fixation
Plate osteosynthesis
Fixation Without Manipulation or Fracture Reduction
Indications
Fractures without any dislocation, angulation (in principle, stable) or distortions
Stable fractures, which are within the age-related range, acceptably angulated
Traction
Indications
Nowadays, less acceptable for children over 5–6 years (acceptable up to 3 years depending on the child’s weight)
Used as an overhead skin traction (skeletal traction should be avoided)
More used for lower extremity (femur fracture) (Fig. 3.9)

Fig. 3.9
Over-head traction for femur fractures in children between 2 and 4 years. Left: preparation of the equipment and the bed; Right: the child is fixed on the frame and applies the traction using the boy’s weight. Within 2 days the parents learn the technique and the child can be treated at home for 3 weeks.
Advantage: can be applied without anaesthesia (only sedation)
Fixation of the extension on the overhead arch so that the child’s buttocks are raised (there should be space for a flat hand to move freely under the buttockswithout touching them)
Possible for out-patient treatment
Closed Reduction and Non-invasive Fixation
Indications
Carry out every fracture reduction under anaesthesia (plexus block, general anaesthesia).
Extend the fingers, hang a weight at the humerus and maintain the upper extremity with 90° flexion at the elbow for 20–30 min
Reduce the fracture using a reduction manoeuvre that mimics the movement that led to the fracture in the first place
Apply the plaster in the hanging position
Immobilize the fracture with a dorso-volar plaster splint
Prepare and use help to fix the lower leg
For plaster cast application ensure the following crucial point : one person is holds the leg, another prepares the plaster cast or fibre cast, and a third makes the cast.
Osteosynthesis with K-Wires
Indications
Closed or open reduced metaphyseal fractures
Fractures of the hand and foot
Contraindication
Diaphyseal fractures.
Technique
Whenever possible, the K-wires should be placed percutaneously so that they can be removed without anaesthesia.
The crossing points of the K-wires should be proximal to the fracture line.
If the epiphysis must be crossed, repeated attempts to fix it should be avoided.
In cases such as this, thin K-wires should be used instead.
K-wires should penetrate the opposite cortex.
Daily care of the pins reduces the risk of infection.
Normally K-wires can be removed after 3 – 4 weeks.
Lag Screw Fixation
Indications
Articular and peri-articular fractures, Salter–Harris II fractures, mainly in the distal tibia and femur, femoral neck fractures
Technique
Use mainly self-drilling and taping cannulated screws (dimensions 3.0/3.5/4.0/4.5/6.5 mm); if these types of screws are not approved in a region, use a normal cannulated cortex screw.
Position the extremity on the intensifier to facilitate the correct view.
Rotate the extremity so that the fracture line is visible in a proper a.p. view.
Put the guide wire on the fragment parallel to the table of the intensifier.
Drill the guide wire into the bone to the contralateral cortex.
Measure the length.
Put the correct-sized cannulated screw over the guide wire.
Tighten the screws until the fracture is closed.
Closed Reduction and External Fixation
Indications
Comminuted fractures in older children (femur, tibia, forearm)
Polytrauma
Long spiral fractures, e.g. spiral wedge of the femur in older children
Technique
The technique used is normally closed reduction with or without extension table
The types to be used are the Monotube system, tubular system, circular frame, TSF
The Schanz screws should be placed under imaging intensifier (take care of the bone size.)
In Monotube systems, the distances between the entry points are predefined.
In “frame systems”, one entry point should be near the fracture, the other further away from it.
All clamps must be open for reduction.
After sufficient reduction, all clamps have to be closed and secured.
Daily care of the pins reduces infection risk.
Note: Due to good healing and associated short healing time, the child is the ideal patient to be treated with an external fixator. To make post-operative management easier and to prevent complications, it is recommended that good patient information is always available.
Intramedullary Elastic Stable Nail Fixation (ESIN)
Indications
Transverse, oblique, short and long spiral, diaphyseal fractures of the long bones in children from (3) 4–14 (15) depending on the child’s weight
Metaphyseal fracture up to 2–3 cm from the growth plate distal and proximal femur, subcapital humerus fracture, supracondylar fractures of the humerus
Radial neck fractures
Nowadays a more complex fracture can be treated with elastic nails when so called Endcaps are used.
There is a special indication for finger and clavicle fractures.
ESIN is a minimally invasive, minimally traumatic, and sufficiently stable for movement and partial weight bearing, biologically and child friendly osteosynthesis using special elastic nails.
Technique
Operation technique: see section on femoral fractures.
Intramedullary Rigid Fixation with Adolescence Lateral Femoral Nail (ALFN)
Indications
Femur shaft fractures in children over 13–14 years when ESIN is not stable enough, especially with over-weight Technique
Supine or lateral position
Preparation of the lateral aspect of the greater trochanter
Opening of the proximal femur according to the OP-technique
Indirect or direct (open) reduction of the fracture
Insertion of the nail over the nail guide wire
Rotation check on the not fractured side before operation; in critical cases, draping both legs to compare rotation during operation
Proximal and distal locking of the nail
Note: Obese children, even if they have a body-weight of 100 kg do not have weight-related bone/medullary canal diameters.
Plate Osteosynthesis
Indications
Comminuted fractures of the diaphysis (femur, tibia, humerus, radius and ulna) mainly in older children
Complex metaphyseal fractures
Technique
Usage of plates is reserved to exceptions and special cases.
When an osteosynthesis with a plate is indicated, the application of new types of plates such as LC-DCP and LCP plates is recommended. If possible, these types of plates can be applied using a minimally invasive technique (MIPO).
Joint Aspiration
Knee Joint Arthrocentesis
Indications
Posttraumatic haemarthros (best time after 24 h)
Signs or suspicion of infection
Technique/Procedure
Apply local anaesthesia or anaesthetic cream well before the puncture.
Puncture in the lateral/proximal recess.
Hip Joint Arthrocentesis
Indication
Posttraumatic haemarthros as soon as possible to decompress the joint (lower limit 4–6 mm distance in the anterior recess in hip ultrasound.)
Signs or suspicion of infection
Technique/Procedure
From lateral approach, or
From anterior approach (be careful of artery and nerve) or
Ludloff approach (author’s preferred approach)
Special Injuries
Spinal Injuries
General Considerations
Spinal injuries in childhood are not as rare as one assumes.
The most common injuries are simple fractures after anterior crush injuries or compression fractures of the vertebral body.
In injuries involving the atlas and axis, rotatory subluxation or dislocation is one of the most common lesions in children, rather than fractures of the atlanto-axial articulation.
Injuries of the thoracic and lumbar spine are more common in childhood than in adulthood. The majority of these fractures result from traffic accidents. Child abuse should also be considered.
Obstetric fractures involve mostly the cervical spine (with high mortality.)
End-plate fractures in younger children are followed by scoliosis.
Fractures of vertebral bodies have good remodelling capacity, depending on the child’s age.
Diagnosis can be difficult owing to congenital malformations (congenital non-union, hemi vertebra, congenital vertebral fusions) or the following diseases (post-traumatic malformations or Scheuermann’s disease).
The normal spine in children differs considerably from that in adults, especially in the cervical region.
Classification
Stable spine fractures with compression of the vertebral body or “end-plate” injuries
Unstable fractures with involvement of the vertebral arch and the pedicles
Ligament avulsion
Fractures involving end-plates with growth disturbance
Fractures not involving end-plates
Diagnostic Studies
Diagnosis includes accurate evaluation of the level and extent of injuries to both chondro-osseous and nervous system tissues.
Radiographic evaluation must be carried out paying due attention to potentially severe unstable injuries and must include prior adequate immobilization of the spine.
Osseous injuries can be seen on an adequate a.p. and lateral view.
Oblique views may be necessary.
CT scan or MRI may be indicated.
Management
A number of unique problems can be encountered in the treatment of infants, children, and adolescents with spine injuries.
In any closed, nonoperative treatment regime, the spinal deformity must be reduced and adequately stabilized and protected from re-displacement during the healing process.
Treatment Guidelines
For stable/non-displaced fractures, simple bed rest is indicated, because most children with stable (compression) fractures are asymptomatic within a few days or weeks. External support may be necessary. Stable/displaced and unstable fractures require surgical stabilization with dorsal fusion.
Prognosis
The prognosis for undisplaced stable fractures is good, depending on the type of injury and the number of involved levels (growth plate/end-plates, wedge compression).
The prognosis for displaced fractures depends on the accompanying neurological problems (Fig. 3.10).


Fig. 3.10
Typical compression fracture in an older child (14 years). CT scan shows the dorsal wall fragment in the spinal canal; fortunately in childhood in 95 % cases there are no neurological problems. Stabilization is mandatory, in this case with an internal fixator system
Clavicle and Pectoral Girdle
Considerations
Fractures of the clavicle are very frequent and occur most frequently in children during the first 12 years.
Fracture in the first 2 years may be a “sign” of non-accidental injury.
Fractures of the scapula in childhood are extremely rare and are mostly a result of a strong direct trauma because the scapula is well protected by muscles and is very mobile.
Table 3.6 gives an overview of the sign/treatment and outcome of clavicle fractures.
Glenohumeral Joint Dislocation
Subluxation and dislocation of the shoulder (Table 3.7) are rare in infants or young children.
Table 3.7
Overview of Gleno-Humeral joint dislocation
Morphology
Fractures of the mid-shaft are most common and range from greenstick to complete fractures
Signs
Pain, swelling, painful movement of the arm
Diagnosis
Clinically and radiologically
Correction potential
Good
Complications
Nerve problems, non-union, cosmetics
Nonoperative therapy
In principle non-surgical – sternal brace or “figure-of-eight” bandage pulling the shoulder backwards
Operative treatment
Only fully displaced, comminuted fractures in adults (author’s preferred method is ESIN)
Immobilization
2–3 weeks
X-ray control
After 3 weeks
Follow-up
Only clinically
The capsule of the shoulder joint has some intrinsic laxity that allows some displacement during stress.
“Dislocation” of the shoulder has also been described as a birth injury. However, great care should be taken before making such a diagnosis as the proximal humerus is most likely to be fractured through to the epiphysis.
Prognosis
For clavicle fractures, the prognosis is very good
Prognosis for the dislocation of the gleno-humeral joint depends on the time lapsed since the incident and the type of injury.
Humeral Fractures
General considerations:
80 % of humeral fractures occur on the distal segment.
Proximal and diaphyseal fractures are rare.
It is mostly direct trauma or so called “wring-injuries” or in Baby’s obstetric injury.
Don’t forget the possibility of a non-accidental injury.
Most of them are transverse or oblique fractures; an exception is wring-injury (spiral wedge fracture).
Fractures of the Proximal Humerus
Proximal humeral fractures and their management are detailed in Table 3.8.
Table 3.8
Morphology/diagnosis and treatment of proximal humerus fractures
Morphology | About 60 % are subcapital fractures; 38 % are Salter–Harris II fractures; pure epiphysiolysis are rare |
Signs | Deformation, pain |
Diagnosis | X-ray; interpretation is often difficult in undisplaced fractures, displacement of the epiphyseal line is interpreted as a fracture |
Note the three ossification centers | |
Correction potential | Great potential, angulation in the sagittal and frontal plane is tolerated up to 60° in children <12 years old and up to 30° >12 years |
Complications | Practically unknown; in neonates premature close of the growth plate is possible |
Nonoperative therapy | Stable, undisplaced fracture, any age Stable fracture with angulation |
<60°: <10 years | |
<30°: >10 years | |
Or | |
Stable fracture with tolerable displacement, any age | |
Immobilization for 3–4 weeks in a Desault or Gilchrist dressing | |
Or | |
Reduction, definitive treatment with stable fixation is recommended | |
Operative treatment | Children >10–12 years of age |
Unstable fracture if a reduction under anesthesia is necessary | |
Major displacement after nonoperative treatment | |
Author’s preferred method: ESIN | |
No additional immobilization is needed | |
Nail removal after 3–4 months | |
Immobilization | 3 weeks (see above) |
X-ray control | Nonoperative therapy: days 3–4 and weeks 3–4 |
Operative treatment: postoperatively and week 4 | |
Follow-up | Week 3 or 4 radiological and clinical |
Operative Treatment
Author’s preferred method
ESIN from a monolateral, radial approach in an ascending technique
Alternative: percutaneous (2.5-mm threaded) K-wire fixation
Open reduction, a rare exception (Fig. 3.11)

Fig. 3.11
A case example of the successful management of a displaced proximal humerus fracture in a skeletally immature patient. After a closed reduction maneuver, the fracture is stabilized by two retrograde elastic titanium nails inserted through a unilateral radial approach in ascending technique. Adequate reduction is ascertained by the “ice-cream on a cone” principle under fluoroscopy in antero-posterior and lateral planes
Humerus Shaft (Diaphyseal) Fractures
See Table 3.9 for an overview of diaphyseal fractures.
Table 3.9
Overview of the morphology, diagnosis and treatment of diaphyseal humerus fracture
Morphology | Rare fractures |
Signs | Deformity, pain |
Diagnosis | X-ray (two images taken at 90° to one another) |
Correction potential | There is a great potential in all planes |
Complications | Damage to the radial nerve (long spiral fractures of the distal third) |
Non operative therapy | Stable undisplaced fracture, any age |
Stable fracture with angulation <30° | |
Or | |
Stable fracture with tolerable displacement, any age | |
Immobilization for 3–4 weeks in a Desault or Gilchrist dressing | |
Or | |
If anesthesia is needed for reduction, definitive treatment with stable fixation is recommended | |
Operative treatment | Children >10–12 years of age |
Radial nerve irritation is not an indication for surgical intervention | |
Unstable fracture if a reduction under anesthesia is necessary | |
Major displacement after nonoperative treatment | |
Author’s preferred method: ESIN | |
No additional immobilization is needed | |
Nail removal after 3–4 months | |
Immobilization | 3–4 weeks |
X-ray control | Nonoperative therapy: days 3–4 and weeks 3–4 |
Operative treatment: postoperatively and week 4 | |
Follow-up | Week 3 or 4 radiologically and clinically |
It is mostly direct trauma or so called “wring-injuries” or in baby’s obstetric injury
Non accidental injury is also possible.
One must be aware of radial nerve lesions.
Rotational failures are not of such a high importance as on the lower extremity.
Prognosis
Very good, independent of age (Fig. 3.12).

Fig. 3.12
One of today’s most popular fixation modalities for humerus shaft fractures. Nowadays, displaced and unstable fractures (10 %) are preferably treated with elastic nails (ESIN). The major indications in our hand are children with head injury (advantage for rehabilitation)
Supracondylar Humerus Fractures
General Considerations (Table 3.10; Fig. 3.13):
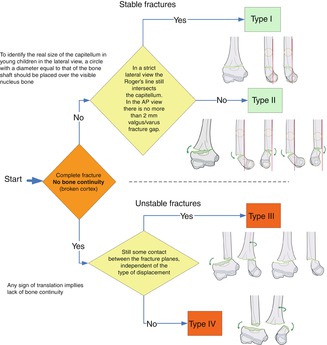
Table 3.10
Overview of the morphology, diagnosis and treatment of the supracondylar humerus fracture
Morphology | See Fig. 3.13 |
|---|---|
Signs | Swelling, pain, visible deformation |
Diagnosis | X-ray in two planes |
Classification: | Incomplete fracture; no displacement (Type I) |
According AO pediatric | Incomplete fracture with more 2 mm gap (Type II) |
Long bone classification | Complete fracture with bone contact (Type III) |
Complete fracture no bone contact (Type IV) | |
Correction potential | Practically does not exist at this place |
Complications | Radial (medial) nerve injury (deep branch) |
Premature closure of the growth plate after repeated drilling | |
Varus deformity as a consequence of a rotational failure | |
Nonoperative therapy | Classification: type I and II |
Blount loop | |
Dorso-volar plaster splint in 90° position | |
Operative treatment | Classification: type III and IV |
Closed reduction (in 90–95 % is possible) | |
Percutaneous K-wire fixation (ascending crossed bilateral, parallel radial, ascending or descending monolateral radial) | |
Small external radial fixator (method preferred by author) | |
ESIN | |
Immobilization | Operative and nonoperative treatment; 3–4 weeks of plaster fixation |
Removal of the percutaneous K-wires at this time | |
X-ray control | Nonoperative treatment: after a few days and at week 3–4, depending of the child’s age |
Operative treatment: after 3–4 weeks | |
Follow-up | 2–3 months after injury functional, clinical examination |
No physiotherapy |
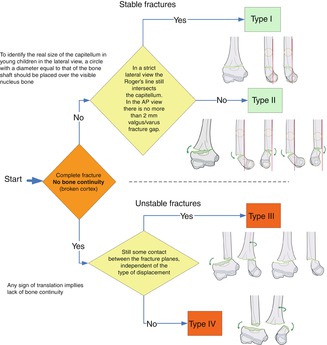
Fig. 3.13
Classification regarding the direction of displacement of the distal fragment according the AO Pediatric Comprehensive Classification for long bone Fractures (PCCF)
These constitute 80 % of all fractures of the humerus.
They can happen from the first year of life up to adolescence.
One must be aware of radial and medial nerve injury.
The absence of the radial pulse is not an absolute indication for a revision of the cubital artery.
We have to distinguish between pulseless pink and pulseless white hand.
A compartment syndrome is the result of too tight a plaster cast; a huge swelling in addition to a tight plaster cast or the swelling of the soft tissue and muscles following the direct trauma.
Prognosis
If reduction and stabilization is adequate and sufficient, a perfect or at least a good functional and cosmetic result can be expected.
Most nerve injuries are temporary; revision is indicated if within 4–5 months there is no visible recovery.
If a cubital artery repair was performed after 4–6 h after injury, a prophylactic fasciotomy is mandatory (Fig. 3.14).
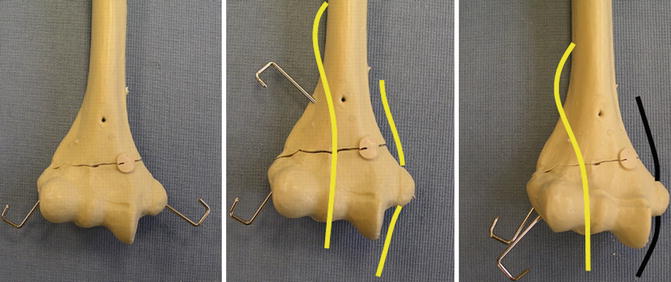
Fig. 3.14
Different treatment/fixation modalities for supracondylar fractures; the most popular and used K-wire fixation, crossed bilateral, crossed only from radial and divergent from radial
Note:
1.
Poor quality reduction leads to poor/insufficient stabilization.
2.
Insufficient/poor stabilization frequently leads to poor functional and cosmetic (cubitusvarus) results.
Fractures Around the Elbow Region
General considerations:
Mostly children between 3 and 10 years old sustain these fractures.
One must be aware of non-accidental injury.
Good knowledge of the child’s anatomy of the distal humerus and the proximal forearm is imperative (Tables 3.11 and 3.12).
Table 3.11
Classification regarding the joint
Articular
Fractures of the lateral condyle
Transcondylar fractures of the humerus
Extra-articular
Supracondylar fracture of the humerus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access





