Figure 5.1
An X-ray showing an avulsion fracture of the right anterior superior iliac spine
Tile and Pennal
A.
Stable fractures.
A1.
Avulsion fractures.
A2.
Undisplaced pelvic ring or iliac wing fractures.
A3.
Transverse fractures of the sacrum and coccyx.
B.
Partially unstable fractures.
B1.
Open book fractures.
B2.
Lateral compression injuries (includes triradiate injury).
B3.
Bilateral type B injuries.
C.
Unstable fractures of the pelvic ring.
C1.
Unilateral fractures.
C1-1.
Fractures of the ilium.
C1-2.
Dislocation or fracture-dislocation of the sacroiliac joint.
C1-3.
Fractures of the sacrum.
C2.
C2. Bilateral fractures, one type B, one type C.
C3.
Bilateral type C fractures (Figs. 5.2, 5.3, and 5.4).


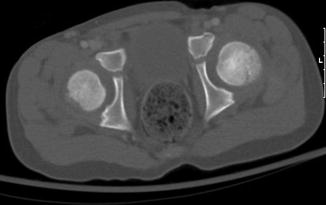


Figure 5.2
Fractures of the left inferior and superior pubic ramus, left sacral alar and widening of the sacral-iliac joints bilaterally

Figure 5.3
X-ray showing an undisplaced fracture of the right inferior sacral alar extending into the sacroiliac joint. There is a displaced fracture of the right inferior pubic ramus and a minimally displaced fracture of the right superior pubic ramus. There is also a minimally displaced fracture involving the left superior pubic rami
Figure 5.4
This is a CT scan of the same patient as Fig. 5.3. It demonstrates the left superior pubic fracture, which extends to involve the left acetabulum

Figure 5.5
An impacted fracture of the left femoral neck
5.4.2 Diagnosis
Avulsion fractures present with localized tenderness and swelling over the fracture site. There is typically a progressive limitation to range of motion. Patients with ischial avulsions experience pain on hip flexion and knee extension, with exaggeration of the pain on hip abduction.
In traumatic pelvic fractures, a full clinical evaluation of a child is necessary with adherence to ATLS protocols. A primary survey and examinations of the chest, abdomen and genitourinary systems should be performed prior to the pelvis. This should include a rectal examination.
When examining the pelvis:
Inspect for lacerations, constusions, haematomas and ecchymosis.
Examine for tenderness, stability and crepitus.
Examine the range of motion of the hip.
Perform a full distal neurological examination.
A painful Trendelenburg sign may suggest an iliac wing fracture (due to abductor muscle contraction).
5.4.3 Imaging
In patients who have sustained a significant trauma, imaging should be preceded by an initial clinical assessment and stabilization of the pelvis where necessary.
In an acute setting, an AP X-ray of the pelvis suffices.
This should be performed as part of the trauma series once the patient is stabilized.
Inlet and outlet view X-rays of the pelvis may be deferred.
A CT scan of the pelvis is indicated if there is:
Doubt with regards to possible injuries.
A plan to perform surgery.
5.4.4 Treatment
The treatment of pelvic and hip fractures depends on the exact injury. The table below summarises the likely mechanism of injury and recommended treatment for the various types of injuries seen.
Fracture | Likely mechanism of injury | Treatment |
|---|---|---|
Avulsion | Ischial tuberosity – Gymnastics ASIS/AIIS – Football Iliac apophysitis – Long distance running | Most do well with conservative management, partial weight bearing for ≥ 2 weeks and extremity positioning Indications for surgery are chronic pain and acute fractures of >1–2 cm |
Unilateral single or double rami fractures | High energy trauma Chronic repetitive stress (stress fractures to single ramus) | Bed rest Gradual weight bearing as pain allows |
Wing of ilium (Duverney fracture) | Direct trauma | Bed rest in a comfortable position, usually with the leg abducted |
Coccyx | Direct trauma | Restriction of activities. Doughnut cushion for 4–6 weeks. |
Fracture near, or subluxation of, pubic symphysis | High energy trauma. Usually associated with posterior structures.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





