The Child at Risk
Most reported cases of child abuse involve children younger than 3 years of age.96 In one report of abused children,30 78% of all fractures reported were in children younger than 3 years of age and 50% of all fractures occurred in children younger than 1 year of age. Infants younger than 1 year are especially at risk for infant homicide, the most severe form of child abuse.76,151 The problem may be more widespread than suspected. In one report,35 covert video recordings of adults attending their children who were hospitalized for suspicious illness documented 14 separate instances of caretaker attempts to cause upper airway obstruction. An infant may present to the emergency room dead or near dead after an apparent “life-threatening event.” In these cases, it is important to be open to all diagnostic possibilities and use a multidisciplinary team approach to the evaluation.201 Possible explanations for these events include SIDS, metabolic disease, cardiac disease, infection, as well as accidental or nonaccidental suffocation. Up to 11% of infants treated in the emergency room for apparent life-threatening events are later confirmed to be victims of child abuse.39 Firstborn children, premature infants, stepchildren, and disabled children are at a greater risk for child abuse, as are twins and children of multiple births.30 Benedict et al.,31 in a longitudinal study of 500 disabled children followed from birth to age 10 years, documented a 4.6% incidence of physical abuse. The most severely disabled children were less likely to be abused, whereas marginally functioning children were at greater risk, with parental frustration considered to be a factor.
The Risk for Child Abuse that Occurs in a Medical Setting
Children who are repeatedly presented by parents for medical assessment of vague illness and have a history of multiple diagnostic or therapeutic procedures for unclear reasons are at risk for having a form of child abuse known as “child abuse that occurs in the medical setting.”251 This term has replaced the previously used “Munchausen Syndrome by Proxy,”193 named after Baron von Munchausen, an eighteenth-century mercenary whose exaggerated tales of adventure were viewed with great suspicion. In child abuse that occurs in a medical setting, children become the victims of this adult behavior when misguided parents fabricate a wide range of illnesses for their children, often subjecting them to needless diagnostic workups and treatment.193 Symptoms of the child’s “illness” are based on an imaginary medical history given by the parent, with signs of the illness either simulated or induced by the parent. For example, a child may be brought into the emergency room by a parent with a complaint of vomiting. This complaint may either be a total fabrication by the parent or the parent may simulate the complaint by producing “vomitus” from some source as proof of illness. In one report, bloodstained material was presented by a caretaker as proof of a child’s “gastrointestinal bleeding,” but DNA testing revealed that the source was actually from the caretaker.276 Conjunctivitis from a caustic agent placed on an infant by a caretaker has been reported.28 Children have been given clozapine and clonidine by caretakers to simulate illness.27 A parent has caused vomiting in a child by the administration of salt191 or ipecac. In other extreme cases, a rodenticide-induced coagulopathy was seen in a 2-year-old child,18 a deliberate self-induced preterm labor was caused by a parent,98 and another repeatedly gave insulin to a 1-year-old child.193 Over half of reported cases of child abuse in the medical setting involve induced symptoms, whereas 25% involve a combination of both simulation and induction of symptoms.39 In less severe cases, the parent’s anxiety can cause them to obtain unnecessary and harmful or potentially harmful medical care, even though the parent believes that he or she is acting in the child’s best interest. Physicians need to be vigilant so as not to be an unwary participant of this form of child maltreatment.
The biologic mother is almost always the perpetrator of child abuse in the medical setting,227 but men can be responsible.192 Caretakers often have a medical background: 35% to 45% are nurses, 5% are medical office workers, 3% are social workers, and 1% are orderlies.227 The perpetrator of the child’s illness denies the knowledge of its etiology; however, the acute signs and symptoms of the child’s illness will resolve if the syndrome is recognized and the child is separated from the parent.227 Follow-up of families with this disorder is crucial. Failure to diagnose this condition places a child at risk for either serious long-term sequelae or death in approximately 9% of cases.
The diagnosis of child abuse in the medical setting remains difficult. Health care workers must have a high degree of suspicion when children present with repetitive illness with no physiologic explanation. Physicians need to recognize that their perseverance in finding an explanation to a child’s illness may contribute to the inflicted harm to the child. When possible, a pediatrician with experience in child abuse should become involved in the evaluation as well as the hospital or community-based multidisciplinary child protection team. A thorough review of all the medical care received by the child and communication among team members is necessary to establish the diagnosis and to recognize patterns of parental behavior that may harm the child. Covert video surveillance (CVS) of caretakers with their children may be a valuable means to substantiate or disprove this diagnosis. Hall et al.102 reported that CVS with audio surveillance allowed diagnosis in 56% of patients monitored and was supportive of the diagnosis in another 22% of children. The approach is expensive, is not covered by third-party payers, and so is infrequently used. Effective treatment generally involves assuring the safety of all children in the family and addressing ongoing dysfunctional family behaviors.
The Risk for Sexual Abuse
Although the orthopedist usually considers child abuse in the context of fractures and other obvious injuries, an increasingly important situation to recognize is sexual abuse. It is estimated that 25% of abused or neglected children have been sexually abused.167 Physically abused children have a one in six chance of being sexually abused, whereas sexually abused children have a one in seven risk of being physically abused.117 Children living with nonbiologic parents or with caretakers who are substance abusers are most at risk. The child usually discloses sexual abuse under three types of circumstances: The child may have just experienced an argument with the abuser and may “accidentally” reveal the existence of the abusive relationship, the child is permanently separated from the abuser, or the abusive adult is shifting attention to a younger sibling.279 Up to 25% to 83% of children with a disability have been reported to be abused.257
OBTAINING THE HISTORY
The history is critical in the diagnosis of child abuse, which is a team effort with the consulting pediatrician, social worker and other personnel from the hospital’s child protective team, child protective services worker, law enforcement, and the appropriate consulting service. The orthopedic surgeon is involved if the child has an injury to the musculoskeletal system. The history is usually taken in the chaotic environment of a busy emergency room, so it is important to find a quiet area for the interview to be conducted calmly and with minimal distractions. The orthopedic surgeon should focus on the facts of the injury, including the child’s ability to get into the injury scenario, details of when, where, and what happened, the child’s position and action before the injury, position after the injury, how the child reacted, and how promptly the caregiver responded appropriately. Such detailed interview skills rarely are taught during residency training. In a survey of pediatric residents, 42% of them had 1 hour or less in training for detection of child abuse, and most orthopedic residents likely have even less.80 In a study comparing the documentation of physical abuse between 1980 and 1995 in a teaching hospital, very little improvement was noted.179 Little progress has been made in how frequently physicians inquire about basic historic information such as the timing of the injury and who were the witnesses.14 The type of hospital that an injured child visits also influences the likelihood that a diagnosis of abuse will be made.269,270 General hospitals were less likely to diagnose a case of abuse compared to children’s hospitals. Use of a structured clinical form can increase the information collected to support the diagnosis of child abuse.24 Having received recent continuing medical education focused on child abuse was the most important factor for a physician to properly recognize and report child abuse.90 Precise documentation in child abuse is vital for reasons beyond medical care. Although most subpoenas for testimony by physicians in child abuse cases do not result in courtroom appearances,212 all documentation in child abuse cases may become evidence in courtroom proceedings. Thus, detailed records are helpful to all in courtroom testimony by physicians.105 The history needed to document child abuse is termed the investigative interview, is a team effort, and should be led by members of the child protective team and the police when potential child abuse is investigated.
The Orthopedic Interview
When involved, the orthopedic surgeon performs a detailed musculoskeletal history and physical examination to characterize the features and mechanism of the obvious injury and to discover evidence of additional undocumented injuries. The interview documents the history (or the lack of history) of the presenting injury and attempts to uncover enough details about the child’s life so that plausible scenarios can be evaluated that might explain the injury. The team should determine how the injured child lives, find out which family members, friends, or other caretakers have access to the child, and how likely it is that they might have contributed to the child’s injuries. A detailed history of injury is obtained individually from each adult family member in a private setting. If the patient and siblings can communicate, they should be interviewed separately from the parents and other members of the family. The location where the injury occurred and which individuals were actually present are documented. The interviewer should follow a systematic review of symptoms: What happened, who was there, when the injury was recognized, and how long before medical treatment was sought. To avoid provoking emotions, any additional soft tissue or skeletal trauma discovered should be brought up at the end of the interview for explanation once the presentation injury has been thoroughly discussed.
Delay in seeking medical care for an injured child is very suggestive of child abuse.81 An infant who has sustained abusive head trauma (AHT) typically will develop immediate neurologic change and will invariably show symptoms within a few hours.37 For a child with head trauma, a caregiver’s story that there was a long period after the injury in which the child had no symptoms is suspicious. When central nervous injury in child abuse is significant or severe, it is immediately symptomatic; thus, the last caretaker who witnessed the reported injury or found the child immediately after the injury is highly suspected of being the perpetrator.23 Inconsistencies are not challenged during the interview. Leading questions are avoided in favor of open-end questions. Medical terms should be explained in plain English, with care taken to avoid medical jargon. More plausible explanations for the injury are not volunteered. Open prompts can enhance the interview.209 If the injury was observed, the caregiver should be able to give a detailed description of the injury mechanism that fits the energy of the fracture and the clinical picture.218,219 The crucial questions to be answered are not only whether the given history of trauma is sufficient to explain the severity of injury, but also what other possible scenarios could explain the injury if the volunteered explanation is not plausible. This requires obtaining a working knowledge of the child’s environment, which team members can obtain by asking specific, detailed questions (Table 9-2).
TABLE 9-2 Child Abuse: Investigative Interview

When interviewing injured children, it is essential to be as gentle as possible, asking how they got hurt rather than who hurt them. Questions asked should be appropriate for the child’s age. The child’s account of what he or she was doing at the time of injury should be compared with the accounts of the adult witnesses. If possible, the siblings of the injured child should be interviewed because they are also at risk for child abuse. Nonvisual cues during the interview should be noted (Table 9-2).
To make the diagnosis of child abuse, the orthopedic surgeon or child abuse team must determine if the history of trauma is adequate to explain the severity of injury.56 This should be based on the experience in the care of fractures with knowledge of their mechanisms of injury and special insight into the types of trauma most likely to cause significant injury. In addition, it is extremely important to have knowledge of the developmental abilities of a child when a caretaker states the child’s injuries are self-inflicted.135 For example, if the parents explain that a 4-month-old infant’s femoral fracture occurred in a fall while the infant was standing alone, this history is inconsistent with the child’s developmental ability.
Details given as the reason for the injury should be carefully considered. Although it is not unusual for a young child to sustain an accidental fall, it is unusual to sustain a serious injury from that fall alone. Infants fall from a bed or a raised surface during a diaper change fairly frequently. In a study of 536 normal infants,165 nearly 50% of them had fallen accidentally from an elevated surface, usually after the first 5 months of life, when the children were able to roll over and were more active. Significant injury in such falls is, however, extremely rare. Combining two studies of 782 children younger than 5 years of age who accidentally fell off an elevated surface, such as bed or sofa, reveals that injuries were limited to three clavicle fractures, six skull fractures, one humeral fracture, and one subdural hematoma.112,163 In another report, a much higher rate of fracture was seen in falls from furniture with 98% having fractures, mostly in the upper extremity, because of the child catapulting during play activity rather than sustaining a simple short-height fall.113 More severe injuries occur in falls from greater heights. Stairway falls usually result in low-energy injuries, but there is increased risk of injury if the child is being carried by the caregiver. In a report of 363 stairway injuries,145 10 were infants who were dropped by their caretakers and four of those sustained skull fractures. In patients 6 months to 1 year of age, 60% were using walkers at the time of the stairway injury. Only 4% of patients had extremity fractures and 1% had skull fractures. Reported short-height falls (<1.5 m) are rarely documented to cause death.55 A review of child mortality in infants and young children in California showed the following causes of death/1 million children/year: Prematurity 165, congenital malformation 316, neoplasms 33, respiratory 38, accidents 121, homicide 22, and short-height falls 0.48 (a total of six cases, all occurring in the home). Although short-height falls are a rare cause of death, there has been no reported case of shortfall death in an institution-type day care setting, where witnesses are typically present. A fatally injured child from a reported short-height fall at home must receive expert postmortem investigation for child abuse.
Additional information about the child and the family may be obtained by a review of past medical records or by contacting the patient’s primary physician and social workers who may have been involved with the family. The physician or social worker should be asked if there has been any previous pattern of injury, illness, ingestion of objects or medications, or noncompliance with health care recommendations; whether the family is receiving counseling or other support from any community groups; and whether the family has any previous involvement with child protective services or law enforcement.80
Documentation Requirements
Careful documentation is critical. Chart notes may later be presented as evidence in court for either custodial hearings or criminal trial.179 Defending inaccurate or partial chart notes in court can be extremely embarrassing as well as placing the child at additional risk. Each account should be recorded in as much detail as possible, using quotation marks for exact quotes and specifying who is giving the history. Particularly with crucial answers, the exact question preceding the response should be documented. In a study of subsequent confessions, the initial history, although not consistently true, did reveal some elements of truth.88 In addition, the general emotional state of the individual providing the account, as well as the individual’s reaction to emotionally charged questions should be documented to assist in later evaluation of the credibility of the account. If the family wishes to change their story after the initial account, no changes should be made to the earlier record, but an addendum should be placed detailing the new account. The completed record should include several specific items such as the timing and mechanism of the injury, who found the child, timing of events, family history of underlying conditions such as osteogenesis imperfecta (OI), radiographs, and documentation of protective services involvement.
PHYSICAL EXAMINATION
After the initial musculoskeletal evaluation for acute fracture assessment, a detailed physical examination should follow, systematically evaluating from head to toes, to detect any signs of additional acute or chronic injury. Acute and subacute fractures may cause local tenderness and swelling, whereas chronic fractures may produce swelling from the presence of callus and clinical deformity from malunion. Radiographs are obtained to confirm clinically suspected fractures. A skeletal survey must be performed in children under 2 years of age when there is reasonable suspicion of abuse12: It should be considered an extension of the physical examination for this age group. A thorough examination should focus on the body areas commonly involved in child abuse including the skin, central nervous system (CNS), abdomen, and genitalia.207 Careful evaluation for signs of previous injury is useful because 50% of verified abuse cases show evidence of prior abuse.100
Soft Tissue Injuries
In addition to examination of the soft tissue around the acute fracture site for swelling and bruising, the patient’s entire body should be systematically evaluated to detect acute and chronic soft tissue trauma. Deliberate soft tissue injuries are present in 81% to 92% of abused patients,96,190,159 making them the most common abuse-related physical examination finding. The types of skin lesions commonly encountered include bruises, welts, abrasions, lacerations, scars, and burns.
The number and location of bruises relate to the child’s development. Seventeen percent of mobile infants, 53% of toddlers, and most school children have bruises.185 Young infants have a much lower prevalence of accidental bruising (seen in 1%) compared to mobile toddlers.185 Accidental bruises in babies are also typically noted over bony prominences.49 The toddler may have multiple accidental bruises over bony prominences such as the chin, brow, knees, and shins.4,230,255 Bruises on the back of the head, neck,4 arms, legs, buttocks, abdomen, cheeks, or genitalia may be suspicious for abuse, although accidental bruises can also occur in all these locations.8 Accidental bruising of the face is much less common and should be carefully evaluated.185 In the dentistry literature, in a series of 266 children suspected of being abused, Jessee and Rieger134 reported that bruises were the most common soft tissue injury, with the most common facial. In nonabused children, only 7% had accidental soft tissue injuries of the face and head, with the peak incidence of 17% seen in toddlers; whereas, soft tissue injuries were present on the lower extremities and buttocks in 31% of children and on the upper extremities in 9%.225 In a study of 1,467 patients seen for reasons other than trauma at a medical center over a 1-year period, 76.6% had at least one skin lesion of recent onset, 17% had at least five, 4% had at least 10, and fewer than 1% had more than 15 recent lesions.169 In children less than 9 months of age, skin lesions were uncommon and were concentrated on the head and face, whereas in children over 9 months of age, the skin lesions were mostly on the lower extremities.169 Although any number of bruises may be present in any child, the location and configuration of the bruises and the mobility of the child, taken together with the rest of the medical and social history determines the suspicion for abuse (Fig. 9-1 and Table 9-3).
TABLE 9-3 Evaluating Bruising in a Child—Implications for Practice


FIGURE 9-1 Schematic illustrates distribution of abusive versus accidental bruising. (Redrawn from original courtesy of Samir Abedin, MD.)
Although the configuration of abusive bruises may resemble the implement used to inflict the injury, the soft tissue injuries of abuse are weapon specific in fewer than 10% of patients.190 The weapons used to abuse children often include belt buckles, staplers, ropes, switches, coat hangers, ironing cords, and the open or closed human hand.136,258 Bruises inflicted by an open hand may appear on the face or a flat area of skin and grasp marks may appear as ovoid lesions when the fingertips are deeply embedded in the extremities or the shoulders of the child during extreme shaking.123 The injury pattern and the severity of the bruising depend on the amount of force used, how directly the instrument made contact, and the specific type of implement used to strike the child.123
Other types of skin lesions may be noted. Welts are more complex skin lesions in which swelling accompanies bruising from injury through lashing or whipping. Lacerations, scars, and burns are seen in older abused children, whereas bruises are seen in all ages.190 Like bruises, the laceration configuration can resemble the weapon used to inflict the injury on the child. Although minor lacerations around the eye are fairly common, multiple scars from either lacerations or burns are suspicious.222,265 Displaced fractures may have associated bruising, with or without abuse. Deep bruising after abuse can be so extensive that rhabdomyolysis can occur, detectable by urine dipstick.216
The age of a bruise can be roughly estimated by a change in color over the 2 to 4 weeks following injury, with fading of the lesions beginning at the periphery. Acute contusions are blue or reddish purple, gradually changing to green, then to yellow, with final resolution as a brownish stain as hemoglobin is finally broken down.278 Langlois and Gresham171 noted that a yellowish bruise must be older than 18 hours; a red, purple, blue, or black coloration of the bruise may be present from 1 hour after injury to resolution; red is always present in bruises regardless of the age; and bruises of identical age and etiology on the same person may be of different appearances and may change at different rates. A deep contusion may take some time to rise to the skin surface because of intervening fascial planes and thus delay its appearance. Although the color of a bruise may roughly aid in determining the length of time it has been present, dating bruises based on appearance should be done with caution.232,250
Natural skin lesions should not be mistaken for bruises. Mongolian spots, more common in black or Asian infants, are deep-blue pigmented areas that are present on the lower back at birth, usually just proximal to the buttocks.17 They do not change in color and gradually resolve as the child matures.123 Cultural differences should be considered when unusual skin lesions are noted. Vietnamese children may be subjected to the folklore medical practice known as cao gio, which places scratches and bruises on the back of the trunk and may be mistaken for child abuse.45 Other conditions can mimic inflicted bruising: Eczema, coagulation disorders, vasculitis, impetigo, Ehlers–Danlos syndrome, vascular malformations, dye stains, and others.259 In cases where bruising or bleeding is the only finding of abuse, a family history for bleeding diathesis, using established protocols for hematologic evaluation for an underlying bleeding disorder and involvement of a hematologist, is advised before child maltreatment is diagnosed.172,262
Burns
Burns are found in approximately 20% of abused patients96 and are most likely to occur in patients younger than 3 years of age.190 Burn evaluation should include configuration, approximate percentage of body surface area, location, distribution, uniformity, length of time the child was in contact with the burning agent, temperature of the burning agent, and presence or absence of splash marks when hot liquids are involved.123
Scalds are the most frequent type of abusive burns and are caused either by a spill or an immersion.164 Accidental spill burns are generally located on the trunk and proximal upper extremities (Fig. 9-2). Most accidental pour or spill burns occur on the front of the child, but accidental burns can also occur on the back as well. In accidental flowing liquid burns, the injury usually has an arrowhead configuration in which the burn becomes shallower and more narrow as it moves downward, and there may be splash marks surrounding the lesion.123 The pattern in accidental burns may also be indicative of flowing water.224 Abuse should be suspected when deep second- or third-degree burns are well demarcated with circumferential definition. The typical child abused by scalding burns is an undernourished 2-year-old child with 15% to 20% of the body involved, usually the buttocks, and has a 10% to 15% mortality rate from secondary sepsis.224
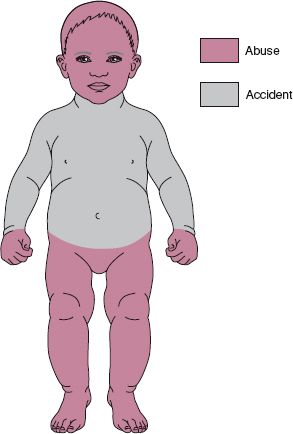
FIGURE 9-2 Schematic illustrates location of accidental versus abusive burns. Note the buttock and lower extremity distribution of nonaccidental immersion burns compared to thoracic distribution accidental burns. (Redrawn from original courtesy of Samir Abedin, MD.)
In accidental hot water immersion, an indistinct stocking or glove configuration may be seen with varying burn depths and indistinct margins. In deliberate immersion burns such as occurs when a child’s buttocks are immersed in hot water, the burn demarcation has uniform depth and a well-demarcated water line.123 The gluteal crease of the buttocks may be spared, giving a doughnut-like appearance to the burn. In accidental hot water immersion, the child is uniformly scalded about the lower extremities as the legs are quickly extended by the child to climb out of the water, but in deliberate, abusive immersion the child is lowered into the water and instinctively flexes the hips and knees, thus sparing the popliteal area.96
Burns can be inflicted by many objects commonly found in the household. Intentional burns by cigarettes are circular, deeply excavated, and sometimes repetitive, usually about 8 mm in diameter.123 Impetigo may resemble scalds or cigarette burns, but is more superficial. Severe eczema may mimic burns suspicious for child abuse.110 Contact with heated objects may cause burns of unique shape that allow identification of their etiology. Children accidentally grasping curling irons sustain burns of the palms, whereas burns on the dorsum of the hands are more suspicious for abuse.135 Hair dryers can be used to inflict burns on children, and full-thickness skin burns can result from the heated air or from contact with the grill up to 2 minutes after it has been turned off.220 Abuse burns have also been inflicted by stun guns.94 These devices deliver a high-voltage impulse of up to 100,000 V at 3 to 4 mA, incapacitating the individual and leaving hypopigmented burn scars on the skin 0.5 cm apart. Circular scars above the wrists may be because of rope burns when children are restrained for beatings.135 Full-thickness skin burns have been reported in small children who were placed in microwave ovens.7 Certain folklore practices may cause lesions simulating abusive burns. Round burns on the abdomen, buttock, or between the thumb and forefinger of Southeast Asian children may be because of a variant on the Chinese medical practice of moxibustion. Folk medical practitioners’ burn balls of the moxa herb on the surface of the skin for therapeutic purposes, and both cigarettes and yarn have been similarly used in refugee camps. The knowledge of these practices may help to avoid inappropriate accusations of child abuse.86
The orthopedic surgeon must examine and carefully document all soft tissue injuries that are present before treating acute fractures. Casts applied in the treatment of fractures, especially a spica cast, may obscure potentially incriminating skin lesions and will preclude other members of the child advocacy team from being able to identify or document them. Photographs taken to document skin lesions must be done before cast placement.
Abusive Head Trauma
Several terms have been used to describe head trauma related to abuse, including the older term shaken baby syndrome (SBS) and the preferred newer terms AHT,37 inflicted traumatic brain injury (ITBI), inflicted head trauma (IHT), or nonaccidental head trauma.201 These terms have been used to describe a form of physical NAT in infants with a triad of subdural hemorrhage, retinal hemorrhage, and encephalopathy occurring with an inconsistent or inappropriate history, commonly associated with other inflicted injuries.106 The American Academy Committee on Child Abuse and Neglect recommends the term “abusive head trauma” to be used in the medical record. Pediatric AHT is defined as “an injury to the skull or intracranial contents of an infant or young child, less than 5 years of age, because of an inflicted blunt impact and/or violent shaking.61,214 Recent excellent review articles discuss fatal AHT95 and the diagnosis of pediatric head trauma in general.125,126 The rate of hospitalization for AHT (36 per 100,000) is similar to that of fractures from NAT (25 to 32 per 100,000).175
A child under the age of 3 years who suffers head trauma from abuse is more likely to have sustained a noncontact injury mechanism (acceleration–deceleration or shaking) resulting in deeper brain injury, cardiorespiratory compromise with diffuse cerebral hypoxia–ischemia, and a worse outcome at 6 months than a child who is accidentally injured.126 Head injuries can be from indirect noncontact forces such as in shaking or from direct contact from a blow to the head such as occurs when the child is thrown against an object. Indirect trauma is felt to be responsible for the most severe injuries, although the actual injury may be from both mechanisms. Symptoms typically occur early rather than later, although secondary or delayed brain injury may occur with edema and the brain’s neurotoxic injury response.
In physical abuse, the most common cause of death is head trauma.223 In Kleinman’s154 classic postmortem study of 31 infants with an average age of 3 months, head trauma was the cause of death in 18. For children less than 2 years of age dying from a traumatic brain injury, 80% of the deaths are from abuse, with the highest incidence at 6 months.93 For a child with AHT, the mortality rate is approximately 20%, and survivors have a higher rate of permanent and significant disability than is seen with accidental trauma.140
When an infant presents with altered mental status, AHT should be suspected (Table 9-4). Jenny et al.132 reported that 31.2% of cases of AHT were misdiagnosed on initial presentation to the emergency room, with a delay averaging 7 days until a correct diagnosis was made. Although early diagnosis of an infant with AHT is essential, primary prevention is the most important new development to occur nationally. There is correlation between peak incidence of infant crying and peak incidence of AHT that occurs 4 to 6 weeks later, suggesting that repeat and prior injuries occur.25 Dias et al.,77 utilizing an early postnatal hospital-based program for new parents to learn about shaking impact syndrome and how to appropriately deal with an inconsolable infant, found a 47% decrease in SBS, whereas intervention programs after abuse was recognized having much less success.182
TABLE 9-4 Criteria for Categorizing the Etiology of Head Injuries

As a general principle, a typical short fall in the home is highly unlikely to cause generalized CNS injury or subdural or retinal hemorrhage, although isolated skull fracture or epidural hemorrhage may be seen. The young infant who is not developmentally mobile enough to cause a fall from a height, having a relatively large head, immature brain, and weak neck muscles, is very vulnerable to the whiplash effects of inflicted violent shaking (Fig. 9-3). In 25% to 54% of confirmed cases of AHT, the abuser described an indirect mechanism by shaking the infant without the head contacting a surface, with resulting immediate onset of symptoms.36,247 Indirect trauma is responsible for the most severe injuries. There is sudden angular acceleration and deceleration with associated rotation of the head and neck in relation to the thorax, producing inertial shear strain deformation and disruption leading to diffuse injury.23 Whereas accidental trauma causes subdural hemorrhage from the translational forces of an impact, IHT from rotational and shearing forces may result in more diffuse subdural or intrahemispheric hemorrhage.120

FIGURE 9-3 Illustration of acceleration–deceleration injury sustained by a shaken infant. Shaken infants suffer whiplash injuries due in part to their disproportionately large heads in relation to their bodies. This mechanism is believed responsible for the common association of subdural hematomas, retinal hemorrhages, and posterior rib fractures. (Artwork courtesy of Gholamreza Zinati, MD.)
The eye of a young infant has a soft sclera: The globe can more easily deform during shaking. This causes vitreoretinal traction leading to direct hemorrhage in the retina and in the optic nerve sheath.282 Fundoscopic examination confirms and documents retinal optic nerve as well as orbital hemorrhage.46 Retinal hemorrhages of abuse classically are multilayered, more anterior, closer to the ora serrata, and are numerous and bilateral. Retinoschisis is a splitting of the layers of the macula forming a cystic cavity caused by shearing and pulling forces of the strong vitreous attachments to the retinal surface and is classic for AHT.229 Unilateral retinal hemorrhages may occur in 10% to 16% of cases, so unilateral does not rule out SBS.16 Although retinal hemorrhages resulting from normal vaginal birth are present in 34% of newborns, these resolve by 16 days of age.121
Previous clinical studies on SBS do not typically address injury to the cervical spine, so it is not known how frequently the spine also is injured with this mechanism.21 In very young infants (2 to 3 months of age), forces may be directed to the upper cervical spine leading to spinal cord injury without obvious radiographic abnormality (SCIWORA), cervicomedullary junction cord injury, apnea, and cardiorespiratory arrest.97,126 Direct head injuries may also occur when the child’s head is slammed onto a soft surface such as a mattress.83 On impact, deceleration forces approaching 400 Gs may occur, tearing the bridging vessels between the skull and the brain and producing intracranial hemorrhage and cerebral edema. Skull fractures are rare unless the child is thrown onto a hard object.
A complete neurologic examination is required for any child suspected of being abused. This should include assessment of the child’s mental status, motor function, sensation, reflexes, and gait, if possible. Any abnormal findings warrant further investigation. Also included should be a dilated fundoscopic examination by an ophthalmologist looking for retinal hemorrhages. For the child with acute neurologic findings suspicious for AHT, a noncontrast computed tomography (CT) scan is done to evaluate for conditions that may benefit from prompt medical and neurosurgical treatment, such as intracranial hemorrhage—acute parenchymal, subarachnoid, subdural, or epidural (Fig. 9-4). If the head CT scan includes upper cervical spine-associated injuries, pre-existing bony conditions such as Klippel–Feil syndrome or occipital cervical assimilation may be detected.119 Anteroposterior (AP) and lateral skull and spinal radiographs are always included as part of the routine skeletal survey for the child less than 2 years of age and should be performed for any aged child with suspected AHT (Table 9-5). CT scans alone may occasionally miss in-plane axial skull fractures. However, these fractures are usually easily seen on the accompanying skeletal survey. Although fine-cut three-dimensional CT skull reconstructions may reveal subtle skull fractures, they may increase delivered radiation by up to 30% over standard head CT. New CT scanners and reformatting algorithms allow for 3D images of the calvarium at no extra radiation dose. Magnetic resonance imaging (MRI) is best used to fully assess various intracranial pathology and has become the imaging modality of choice for evaluating asymptomatic, nonacute parenchymal brain lesions and for fully documenting the abuse. MRI is also effective for diagnosis of related conditions in the cervical spine, including ligamentous injury and intraspinal injuries such as SCIWORA.
TABLE 9-5 Complete Skeletal Survey Table


FIGURE 9-4 Interhemispheric subdural hematoma in an 8-month-old female presenting with seizures caused by nonaccidental trauma. Axial CT image shows high attenuation blood along the left aspect of the posterior falx (arrow).
Even in abused children without neurologic findings or retinal hemorrhages, occult head injury should always be suspected. At risk children with obvious neurologic findings should be urgently screened with head CT for acute pathology. At risk children without obvious neurologic findings are best imaged initially with MR brain imaging (ACR guidelines).12 MRI is sensitive for diagnosing small parenchymal hemorrhages83 and offers the highest sensitivity and specificity for the diagnosis of subacute and chronic head injuries.12 Diffusion- and susceptibility-weighted imaging sequences are extremely sensitive for detecting subtle hypoxic–ischemic brain injury and parenchymal hemorrhage213,256 and are routinely included in imaging protocols when available. MR venography may be used if venous sinus thrombosis is suspected. MR spectroscopy may detect lactate levels, an indicator of prognosis.87
Infants with acute head injuries may have fever, bulging fontanelles, and macrocephaly. Paresis may be present, and reflexes may be increased. Older infants and children may have subdural hemorrhages and musculoskeletal injuries.97 Classic infant AHT with multilayered retinal hemorrhages and acute subdural hematomas has been noted in an autopsy series of four older children between 2.5 and 7 years of age.229 Cerebral edema may be lethal,60 so emergency neurosurgical consultation may be needed. Barnes and Krasnokutsky23 reviewed the radiographic evaluation of a young child with a suspected nonaccidental head injury, including mimicking of conditions, such as accidental injury from short falls, acute CNS infections, coagulopathies, venous thrombosis, metabolic abnormalities, and neoplasms. The diagnosis of these mimics may require more extensive workup before a diagnosis of AHT is confirmed (Table 9-6).242 Oehmichen et al.204 have presented very practical principles for diagnosing AHT (Table 9-7).
TABLE 9-6 Differential Diagnosis of Subdural Hemorrhage in Infants and Children

TABLE 9-7 Principles of Diagnosing Inflicted Traumatic Brain Injury in Children

Disability after AHT is frequent and ranges from mild to severe. Common late sequelae after AHT include developmental delays, sensory and motor deficits, feeding difficulties, recurrent seizures, attention deficits, and intellectual, educational, and behavioral dysfunctions.126 In a long-term outcome study, 69% of children had an abnormality and 40% had severe dysfunction.22 Approximately 50% had visual impairment and another 50% had behavior disorder.22 Some children seemed normal until 5 years after the inflicted injury, then showed learning disorders, so long-term follow-up is essential. Repeat abuse when AHT is not recognized and the child is returned to the home is too common.97
Abdominal Injuries
After AHT, trauma to the abdomen is the second most common reason for death from abuse.39 In a review of the National Pediatric Trauma Registry, 16% of all blunt abdominal trauma in children 0 to 4 years of age was attributable to child abuse.268 The pediatric thorax and pelvis are very compliant. The abdominal muscles are pliable with little subcutaneous and omental fat, so there is less protection to the internal abdominal, chest, and pelvic organs. Whereas shaken infants sustain head trauma, toddlers receive abdominal injuries as they are more often punched and beaten. Inflicted abdominal trauma may be because of beatings with the hand, fist, or when the child is thrown into a fixed object. The compliant pediatric abdominal wall does not absorb much of the injury energy, so abdominal bruising is present in only 12% to 15% of major intra-abdominal injury cases.123 Children with inflicted injuries are more likely to be of a younger age, malnourished, have a pancreatic or hollow viscous injury, have an associated traumatic brain injury, and have higher mortality compared to victims of accidental abdominal injury.268
Children with abdominal injury from child abuse may have a wide range of symptoms depending on the organ involved and the severity of the injury. Fever, vomiting, anemia, abdominal distention, localized involuntary spasm, and bowel sounds may be absent.207 The liver is the most commonly injured solid organ. With a damaged liver, right shoulder pain from hemidiaphragm irritation (Kehr sign) may be associated with abdominal pain and fatal hypovolemic shock.266 Liver function tests may reveal occult liver injury. In one study,64 elevated aspartate aminotransferase, alanine aminotransferase, and lactic dehydrogenase enzyme levels were useful markers for occult liver lacerations in abused children who had false-negative abdominal examinations. Blows to the abdomen often injure the pancreas as it is violently compressed against the spine. Blunt pancreatic injury caused by NAI commonly presents with contusion, transaction, or laceration, all of which are associated with pancreatitis and elevated blood amylase. A pancreatic pseudocyst may form, causing obstructive symptoms several weeks after initial injury.123 Splenic and renal injuries, rare in child abuse, have a 45% risk of mortality from hemorrhagic or septic shock if care is delayed.67
Hollow organ injuries to the upper or lower gastrointestinal tract or bladder are infrequent in accidents but common in child abuse, particularly in the younger child (mean age 2.5 years).173 Hollow organ abuse injuries, as is true for most abdominal injuries caused by NAI, presented for medical attention late, with an inconsistent or vague history. In a young child with unexplained hollow organ injury, abuse should be suspected and investigated.
Child abuse is the leading cause of duodenal injury in children less than 4 years of age.267 Intramural duodenal hematoma may cause obstruction and bilious vomiting.123 CT, ultrasound imaging, and/or upper gastrointestinal radiography may be diagnostic (Fig. 9-5). More severe trauma may cause duodenal avulsion or transection with nausea, vomiting, and clinical acute abdomen.181 Frequently, the radiologist first suggests the possibility of NAT by finding a duodenal hematoma with no history by the caregiver of trauma. Blunt trauma to the abdomen may also cause intestinal perforation, usually involving the small intestine, and the physical examination may suggest peritonitis. Previously, plain radiographs were used to search for free air in suspected hollow organ injuries; however, only 19% of radiographs were diagnostic.41 Today, CT with intravenous contrast enhancement is used for the trauma evaluation. CT imaging better reveals free fluid, focal bowel wall thickening, inflammation, or ileus. Associated spine injuries, such as Chance flexion–distraction lumbar spine fracture, should be evaluated.

FIGURE 9-5 Duodenal hematoma and pancreatic transection in a 4-year-old male presenting with bilious vomiting caused by nonaccidental abdominal trauma. A: Fluoroscopic upper gastrointestinal image reveals a large, well-defined defect within the third portion of the duodenum (arrows). Axial contrast-enhanced CT images at the level of the duodenum (B) and pancreas (C) show a large hyper attenuated retroperitoneal duodenal hematoma (arrows) and a linear low attenuation defect (arrowhead) in the pancreatic head. Also noted is peripancreatic fluid.
The Academy of Pediatrics Section on Radiology12 recommends CT scans with nonionic intravenous contrast to define injury to abdominal organs. Contrast should not be used if there is a history of iodine allergy or renal failure. The use of oral contrast is debatable with CT scans and may place the patient at risk of aspiration. Ultrasound and upper gastrointestinal series are most often used to evaluate duodenal hematoma. When abdominal injury is suspected in an abused child, the hematocrit and hemoglobin levels are checked, the child is typed and crossmatched for blood, and two large intravenous lines are placed in anticipation for surgical treatment. General surgery consultation is obtained. The overall mortality rate associated with visceral injury in child abuse is 40% to 50%.64 In fatal cases with liver injury, hepatic glycogen staining may be helpful in establishing time of death for legal reasons.261 Occult abdominal trauma is easily missed, so a high index of suspicion with serial abdominal examination and liberal use of abdominal CT should be used in the suspected abused child.120
Genital Injuries
Sexual abuse should always be considered when evaluating a physically abused child. Specific guidelines for the evaluation for sexual abuse were revised and published in 2005.2 Children who have been sexually abused can have symptoms of bed wetting, fecal incontinence, painful defecation, pelvic pain, abdominal pain, vaginal itching and bleeding, sexually transmitted diseases, and pregnancy in postmenarche adolescents. Sexually transmitted diseases found in abused children include gonorrhea, syphilis, chlamydia, trichomoniasis, and lymphogranuloma venereum. Although the percentage of sexually assaulted children with obvious physical trauma to the genitalia is low, failure to document such findings is a serious matter. Sexual abuse is always a criminal offense and must be reported to legal authorities. The physical signs of sexual abuse, including genital trauma, sexually transmitted diseases, or presence of sperm, are present in only 3% to 16% of verified sexual assaults,29,241 but even this minority of patients will be undiagnosed if sexual abuse is not considered when a child presents with musculoskeletal injury resulting from abuse.
The orthopedic surgeon should be aware of the proper procedure for handling suspected sexual abuse, but is not expected to manage this evaluation. When sexual abuse is suspected, consultation with an experienced medical team will assure competent assessment of the child’s physical, emotional, and behavioral needs, manage reporting and legal requirements, and interact with appropriate professionals to provide comprehensive treatment and follow-up.2 The child’s genitalia should always be examined and documented in a chaperoned setting by an appropriate physician consultant such as a pediatrician or a gynecologist. If the sexual assault occurred within 72 hours of evaluation, then a rape kit must be used by the evaluating physician or nurse examiner to provide medical evidence of the attack.167 However, detecting semen on examination for forensic evidence decreases markedly after 24 hours.211
Patterns of injury that suggest, but are not specific for, sexually motivated assault include bruises, scratches, and burns around the lower trunk, genitalia, thighs, buttocks, and upper legs, including the knees. Pinch or grip marks may be found where the child was held. Attempted or achieved penetration may involve the mouth, vagina, or anus.117 Sexually abused boys may have poor rectal sphincter tone, perianal scarring, or urethral discharge. Female genital examination findings that are consistent with sexual abuse include chafing, abrasion, or bruising of the inner thighs or genitalia, distortion of the hymen, decreased or absent hymen, scarring of the external genitalia, and enlargement of the hymenal opening.11 The size of the transverse hymenal orifice does not correlate as a marker of child abuse.127 The examination of the female genitalia can be normal even when there has been penetration, because hymen tissue is elastic and there can be rapid healing. In a study of 36 adolescent pregnant girls evaluated for sexual abuse, only 2 of 36 had genital changes diagnostic of penetrating trauma, suggesting that injuries either may not occur or may heal completely.141 There is also a wide variability of appearance of normal female genitalia,48,60 but posterior hymen disruption is rare and should raise suspicion for abuse.33
FRACTURES IN CHILD ABUSE
Overview
After skin lesions, fractures are the second most common physical presentation of abuse. Fractures, documented on plain radiographs or CT, are present in 11% to 55% of abused children and are most common in children younger than 3 years of age.4,73,100 The child abuse literature shows varying incidence of abuse-related fractures, depending on the age of the study population, institution, study entry criteria, selection bias, and time period when the study was published.174 The younger the child with a fracture, especially under 18 months of age, the more likely abuse is the cause.62,65,143 Fractures resulting from abuse should be suspected in young children if a caretaker brings the child for evaluation but reports no history of accidental trauma, especially if the caretaker reports a change in the child such as extremity swelling or decreased movement of the limb. Particularly concerning is a bone that fractures under tension with torsion, rather than the physiologic loading of compression of normal childhood activity or falls. Pierce et al.219 recommend that the clinician determine if the observed injury of a long bone and the stated mechanism are consistent (Table 9-8).
TABLE 9-8 Considerations When Evaluating a Child with a Long-Bone Fracture

Kleinman ranked the specificity of skeletal fractures for abuse (Table 9-9) based on the location and type of fracture. He emphasized that both moderate and low specificity radiographic findings become more specific when there is an inadequate or inconsistent explanation for the injury. The location and the type of fracture can aid in distinguishing between an accident and child abuse, but is only one piece of information.
TABLE 9-9 Specificity of Skeletal Trauma for Abuse

All types of fractures have been reported in the child abuse literature, and it is often the presence of multiple fractures that indicates NAT (Fig. 9-6). In one of the largest series, King et al.147 reported 429 fractures in 189 abused children. Fifty percent of these patients had a single fracture, and 17% had more than three fractures. Approximately 60% of fractures were found in roughly equal numbers in the humerus, femur, and tibia. Fractures also occurred in the radius, skull, spine, ribs, ulna, and fibula, in order of decreasing frequency. Another study207 found a similar incidence of fractures of the humerus, femur, and tibia in abused children, with skull fractures seen in 14%. In contrast, Akbarnia et al.3 found that rib fractures in abused patients were twice as prevalent as fractures of any one long bone; the next most frequently fractured bone was the humerus, followed by the femur and the tibia. Nearly a third of these patients had skull fractures. Loder and Bookout181 reported the tibia to be the bone most commonly fractured in their series of abused children, followed by the humerus, the femur, the radius, and the ulna. In a classic study of 31 postmortem infants, the fracture pattern was very different from clinical studies in living children.154 Highly detailed skeletal, specimen, and histopathologic analysis revealed 165 total fractures, most commonly in ribs, distal femur, the ends of the tibia, and skull (Fig. 9-7). The fact that 29 of the 31 infants had evidence of a healing fracture provides sobering evidence of the need to aggressively diagnose NAT before an infant is killed.


FIGURE 9-6 Multiple fractures in a 3-month-old female victim of inflicted injury. A: Frontal radiograph of the humerus shows proximal metaphyseal irregularity consistent with a corner fracture (arrow) and an oblique diaphyseal fracture with extensive periosteal reaction and healing (arrowhead). B: Axial CT image reveals a depressed left calvarial fracture (arrow). C: Lateral thoracolumbar radiograph suggests a T12 compression fracture (arrow), which is confirmed on nuclear bone scintigraphy (D) as a region of increased uptake (arrow). Bone scan also confirms left parietal (arrowhead) and humeral (curved arrow) fractures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


