Chapter 13. The lumbar spine
SUMMARY
This chapter outlines the relevant anatomy to enable discussion of evidence for the causes of back pain and differential diagnosis. The clinical examination procedure will be outlined and interpreted, and the models used in orthopaedic medicine will be identified to act as a guide to treatment using this approach.
ANATOMY
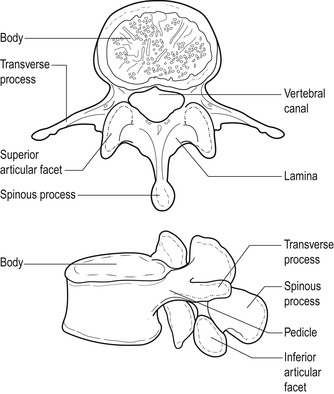
There are five lumbar vertebrae, each with a large vertebral body designed for weight-bearing (Fig. 13.1). Each vertebral body consists of a shell of cortical bone surrounding a cancellous cavity of supporting struts and cross-beams called trabeculae. This provides a lightweight box with the strength to support longitudinally applied loads. The intervening intervertebral disc provides a mechanism for shock absorption, distribution of forces and movement (Jensen 1980).
 |
| Figure 13.1 Typical lumbar vertebra. From Anatomy and Human Movement by N Palastanga, D Field and R Soames. Reprinted by permission of Elsevier Ltd. |
The stabilizing function of the lumbar spine is achieved by the various bony processes that make up the posterior elements of the lumbar vertebrae, i.e. the pedicles and laminae, and the articular, spinous and transverse processes. The position and direction of the articular processes that form the synovial zygapophyseal joints prevent forward sliding and rotation of the vertebral bodies, while the spinous and transverse processes act as leverage and provide attachment for muscles.
The vertebral foramen is surrounded by the vertebral body in front and the posterior elements behind. It is triangular in the lumbar spine and is larger than that in the thoracic spine but smaller than that in the cervical spine. Together the vertebral foramina form the vertebral canal which contains the termination of the spinal cord opposite the L1–L2 disc, and the cauda equina. The vertebral canal can vary in shape and this may be relevant to pathology.
The lumbar lordosis, the posterior postural concavity, compensates for the inclination of the sacrum and maintains the upright posture. The wedge-shaped lumbosacral disc and vertebral body of L5 contribute to the lordosis as well as the antigravity effect of the constant activity in the erector spinae muscles that prevent the trunk from falling forwards (Oliver & Middleditch 2006).
The intervertebral disc
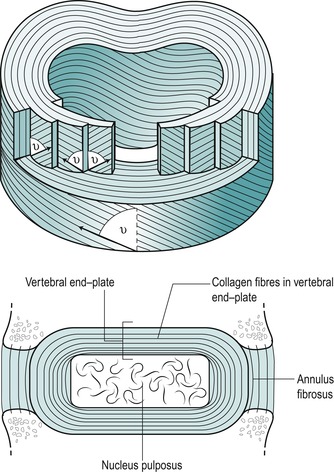
The intervertebral disc has special biomechanical requirements. It is strong to sustain weight and transmit loads while being able to deform to adjust to movement. The intervertebral disc has three parts: a central nucleus pulposus surrounded by a peripheral annulus fibrosus which blends above and below into vertebral end-plates.
The nucleus pulposus accommodates to movement and transmits compressive loads from one vertebral body to another. Its normal consistency has been likened to that of toothpaste. It is composed of irregularly arranged collagen fibres and cartilage cells scattered within amorphous ground substance. The collagen fibres are composed of type II collagen, suited to accept pressure and compression (see Ch. 2). The nucleus in particular has great water-binding capacity through its proteoglycan content. The fluid nature of the nucleus allows it to deform under pressure while the vertebral end-plates prevent its superior and inferior deformation. In this way the intervertebral disc supports and transmits loads.
Although it has long been recognized for its fluid properties, the nucleus also behaves as a viscoelastic solid under dynamic conditions. Iatridis et al (1996) investigated the viscoelastic properties of the healthy nucleus pulposus, showing it to be sensitive to different loading rates. The higher loading rates produced failure of the end-plate and vertebral body, while slower loading rates produced progressive failure of the annulus and disc herniation.
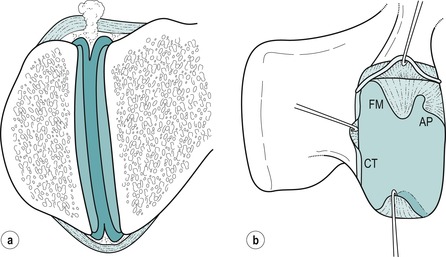
The annulus fibrosus consists of a geometrically organized arrangement of collagen and elastic fibres bound together by a proteoglycan gel, allowing it to support weight without buckling. Types I and II collagen exist in the annulus fibrosus, but the majority of fibres are type I, suited to withstand tensile forces. The fibres are arranged in concentric lamellae around the central nucleus. These tightly packed lamellae are arranged circumferentially at the periphery and can sustain high compressive loads. Adams et al (2002) suggest an analogy to the stiffness of a telephone directory rolled into a cylinder and stood on its end. In each lamella, the collagen fibres lie parallel to each other, inclined at an angle of approximately 65–70° to the vertical (Fig. 13.2). The direction of fibres alternates in adjacent lamellae (Bogduk 2005). Marchand & Ahmed (1990) noted a number of irregularities within the laminate structure of the annulus, particularly at the posterolateral corners, where a number of incomplete layers were seen. Increased stresses applied to the annulus in this region could produce fissuring and provide the nuclear material with an escape route.
 |
| Figure 13.2 Laminate structure of the disc. Reprinted from Clinical Anatomy of the Lumbar Spine and Sacrum. N Bogduk © 1998, by permission of Elsevier. |
The annulus fibrosus acts like a ligament, restraining excessive movement to stabilize the intervertebral joint while allowing flexibility to permit normal movement. The alternating oblique annular fibres resist horizontal and vertical forces, allowing the annulus to oppose movement in all directions (Bogduk 1991).
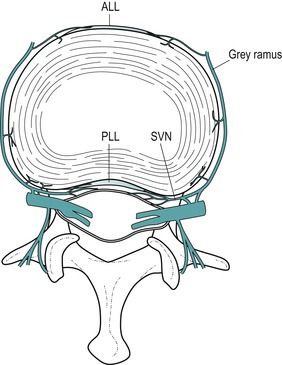
The outer half of the annulus at least is known to have a nerve supply (Cavanaugh et al 1995, Coppes et al 1997). The main source of the supply is believed to be the sinuvertebral nerve and branches of the sympathetic trunks and its grey rami communicantes (Adams et al 2002) (Fig. 13.3). The sinuvertebral nerve supplies the disc at one level and the disc above (Bogduk 2005).
 |
| Figure 13.3 The nerve supply of a lumbar intervertebral disc depicted in a transverse view of the lumbar spine. Branches of the grey rami communicantes and the sinuvertebral nerves (SNV) are shown entering the disc and the anterior and posterior longitudinal ligaments (ALL, PLL). Branches from the sinuvertebral nerves also supply the anterior aspect of the dural sac and dural sleeve. Reprinted from Clinical Anatomy of the Lumbar Spine and Sacrum. N Bogduk © 1998, by permission of Elsevier. |
The vertebral end-plates are thin layers of cartilage, approximately 1 mm thick, covering the superior and inferior surfaces of the discs. They form a permeable barrier for diffusion, mainly between the nucleus and the cancellous bone of the vertebral bodies. They fail relatively easily under excessive compressive loading.
Properties of the intervertebral disc
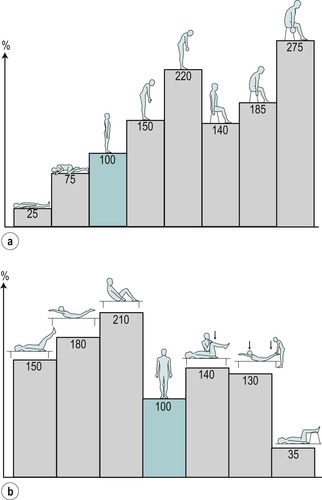
The intervertebral disc at rest possesses an intrinsic pressure due to the compressive effect of the elastic ligamentum flavum (Oliver & Middleditch 2006). This preloaded or prestressed state provides it with an intrinsic stability to resist applied forces such as body weight (Jensen 1980). The resting pressure is affected by posture and loading, being lowest in the lying position and highest in the sitting position, with a further increase if external loading is applied (Nachemson 1966). In the sitting position the spine usually rests in a degree of flexion and the activity in psoas major contributes a compressive effect on the disc as it stabilizes the spine.
The terms ‘somatic’ and ‘radicular’ are discussed within Chapter 1. Clinically, somatic back pain and radicular pain are affected by movements and posture, as well as being increased by straining, coughing or laughing. An increase in intradiscal pressure of about 50% was noted when straining was performed in standing, due to the increase in loading produced by muscle activity (Nachemson & Elfstrom 1970). The chart originating from the investigations of Nachemson (1966) has been reproduced in several publications as a useful guide to the variation in intradiscal pressure with different postures and activities (Fig. 13.4).
 |
| Figure 13.4 Discal pressures. Relative change in pressure (or load) in the third lumbar disc: (a) in various positions; (b) in muscle-strengthening exercises. From A Nachemson 1976 The lumbar spine: an orthopaedic challenge. Spine 1:59–71, with permission. |
Movement of the spine involves simultaneous tension, compression and shear at different locations of the disc affecting intradiscal pressure and fluid flow. Flexion, extension and side flexion produce tension resulting in stretching of the annulus on one side, and compression on the other side through body weight (Jensen 1980). Flexion includes a component of forward translation that is stabilized by the zygapophyseal joints, while extension is limited by bony impaction of the inferior articular processes against the lamina of the vertebra below. Axial rotation produces torsion in the intervertebral discs, with tension in half of the annular fibres that are inclined towards the direction of the rotation, and impaction of the zygapophyseal joints. Side flexion is a composite movement which includes side flexion and rotation (Bogduk 2005).
As a viscoelastic material, the intervertebral disc is subjected to the phenomena of creep, hysteresis and set (Twomey & Taylor 1982, Oliver & Twomey 1995, Bogduk 2005), as discussed in Chapter 2. The creep behaviour of flexion and extension is similar, with the amount of creep increasing with load and progressing with time. Creep also increases with age when hysteresis recovery is slower. Flexion creep, in particular, has implications for occupations that require a constant flexed posture, e.g. manual workers. It may also be responsible for fatigue in the disc, making it vulnerable to a sudden applied force – the ‘straw that breaks the camel’s back’.
Nutrition of the intervertebral disc
The lumbar discs have a relatively poor blood supply since no arteries enter the disc and it is the largest avascular tissue in the human body (Adams et al 2002, Paesold et al 2007). Nutrition of the intervertebral disc occurs through two routes: the blood vessels situated around the peripheral annulus and those in the central portion of the vertebral end-plate. The outer annulus may be supplied with nutrients from blood vessels in the adjacent longitudinal ligaments but the supply to the nucleus pulposus cells is almost completely dependent on diffusion via the end-plate capillary network (Paesold et al 2007). The mechanisms involved are diffusion and fluid flow and are interrelated. Both are affected by posture and motion (Adams & Hutton 1986).
The water content of the disc varies and represents a balance between two opposing osmotic and hydrostatic pressures, i.e. a swelling pressure (imbibition) which hydrates the disc and a mechanical pressure (posture, movement, loading and creep) which dehydrates the disc. Diurnal decrease in the total length of the spine is offset by its recovery in the supine position overnight (Parke & Schiff 1971, Porter 1995). Flexion postures cause a larger fluid outflow from the disc than erect or lordotic postures, with this outflow being further reduced when the spine is unloaded by lying down. Alternating between rest and activity will enhance fluid flow (Adams & Hutton 1983, 1986). Factors that influence the nutrition of the disc are increased loading, vibration or spinal deformity. Factors that compromise the vascular supply include smoking, vascular disease and diabetes (Buckwalter 1995).
Zygapophyseal joints (facet joints)
The zygapophyseal joints are synovial joints that provide stability of the spine, control of movement and protection of the intervertebral discs (Fig. 13.5) (Taylor & Twomey 1994). The articular facets are covered with articular cartilage and the joints are surrounded by a fibrous capsule and lined with synovium. The superior articular facets face posteromedially and grasp onto the inferior articular facets of the vertebra above, which face anterolaterally. The resultant plane of the joint facilitates flexion and extension movements, but prevents rotation. It also restricts translation in healthy joints, helping to protect the lumbar disc from the shearing forces responsible for fissuring (Bogduk 1991, Taylor & Twomey 1994).
 |
| Figure 13.5 Intra-articular structures of the lumbar zygapophyseal joints. (a) Coronal section of a left zygapophyseal joint showing fibroadipose meniscoids projecting into the joint cavity from the capsule over the superior and inferior poles of the joint. (b) Lateral view of a right zygapophyseal joint, in which the superior articular process has been removed to show intra-articular structures projecting into the joint cavity across the surface of the inferior articular facet. The superior capsule is retracted to reveal the base of a fibroadipose meniscoid (FM) and an adipose tissue pad (AP). Another fibroadipose meniscoid at the lower pole of the joint is lifted from the surface of the articular cartilage. A connective tissue (CT) rim has been retracted along the posterior margin of the joint. Reprinted from Clinical Anatomy of the Lumbar Spine and Sacrum. N Bogduk © 1998, by permission of Elsevier. |
The fibrous capsule consists of an outer layer of regularly arranged connective tissue and an inner layer of yellow elastic fibres. Anteriorly the capsule is replaced by the ligamentum flavum, while some of the deep fibres of multifidus give the capsule reinforcement medially (Yamashita et al 1996). The superior and inferior aspects of the capsules are loose and contain intra-articular structures consisting of fat and meniscoid structures (Bogduk 2005). Fine nerve fibres thought to conduct nociceptive and proprioceptive sensations have been found (Yamashita et al 1996).
The zygapophyseal joints cannot be discounted as a cause of back pain since, as synovial joints, they may be subjected to trauma or arthritis. Degenerative changes usually coexist in the intervertebral joint of the same segment.
Authors have looked at the pattern of pain referral of the zygapophyseal joints in an attempt to establish a recognized syndrome and pain referral patterns (Mooney & Robertson 1976, Bogduk 1994). Schwarzer et al (1994a) acknowledged this joint as a possible source of pain, but questioned the existence of a facet syndrome. Some authors suggest that the zygapophyseal joint is responsible for the acute locked back, as the intra-articular structures become trapped between the articular surfaces (Twomey & Taylor 1994, Bogduk 2005), while Kuslich et al (1991) demonstrated that stimulation of the zygapophyseal joint capsule very rarely generates leg pain. In a study of the relative contributions of the disc and zygapophyseal joint in chronic low back pain, pain was noted to arise more commonly from the disc than the zygapophyseal joint (Schwarzer et al 1994b).
Laslett & van Wijmen (1999) suggest that the symptomatic zygapophyseal joint presents with pain that settles well on lying down and four of the following criteria: age greater than 65; pain not increased by coughing; no pain on flexion in standing; pain not increased in rising from flexion; pain not increased by extension/rotation; or pain not increased by extension in standing.
The authors of this text accept the lack of evidence to attribute the cause of low back pain to one specific structure and that will also apply to the symptomatic zygapophyseal model presented above. Orthopaedic medicine treatments have traditionally been based on the discal model but it may be more clinically relevant to apply treatments selected on the basis of a particular set of signs and symptoms rather than to attempt to be too pedantic with regard to pathology (see below). It must be acknowledged that a lesion in any structure within a spinal segment will influence neighbouring structures and similarly treatment cannot be directed to one anatomical structure in isolation.
Ligaments
Anterior and posterior longitudinal ligaments are well developed in the lumbar region where both stabilize the vertebral bodies and control movement (Fig. 13.6). The anterior longitudinal ligament is widest in the lumbar spine where it covers most of the anterior and lateral surfaces of the vertebral bodies and intervertebral discs. The posterior longitudinal ligament is relatively weaker and has a denticulate arrangement that permits the passage of vascular structures. Superficial fibres bridge several vertebrae while deeper fibres pass over two joints and have lateral extensions intimately related to the intervertebral disc (Parke & Schiff 1971). The strong central portion of the posterior longitudinal ligament provides resistance to central disc displacement, deflecting it laterally where the lateral extensions are deficient and offer a space for posterolateral displacement.
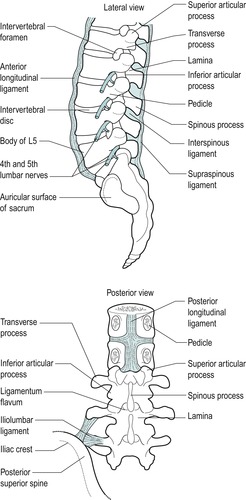 |
| Figure 13.6 The ligaments of the lumbar spine. |
The ligamentum flavum consists of predominantly yellow elastic fibres and connects adjacent laminae. It controls lumbar flexion by ‘braking’ the separation of the laminae and assisting the return to the upright posture. The elastic fibres also restore the ligament to its normal length after stretching, to prevent buckling into the spinal canal and compression of the spinal cord or cauda equina. Such pathology may arise in the degenerate ligament and contribute to stenosis.
The iliolumbar ligament provides stability for the lumbo-sacral junction (Yamamoto et al 1990), attaching the L5 transverse process to the pelvis. Sometimes a band also passes from the transverse process of L4. This anchorage of L5 to the pelvis may restrict the amount of accommodation possible for disc herniation. Disc herniation at the L5, S1 level may produce severe pain with the patient fixed in flexion, whereas herniation above this level, usually L4–L5, may be accommodated more readily by a lateral shift that will reduce pain.
LUMBAR SPINAL NERVES
The termination of the spinal cord lies approximately level with the L1–L2 disc, and the lumbar and sacral nerve roots descend vertically in the cauda equina, surrounded by the dural sac, to exit via their appropriate lumbar or sacral intervertebral foramina.
Dorsal (sensory) and ventral (mainly motor) nerve roots join to form the relatively short spinal nerve that is situated in the intervertebral foramen, together with the dorsal root ganglion. The dorsal root ganglion is the collected cell bodies of all sensory nerve fibres related to that segment. The cell bodies of the motor axons are located in the anterior horns of the grey matter in the spinal cord. In the intervertebral foramen the spinal nerve is surrounded by the dural nerve root sleeve, which eventually blends with the epineurium of the nerve. Immediately after leaving the intervertebral foramen the spinal nerve divides into dorsal and ventral rami.
Spinal nerves do not possess the same protective connective tissue sheaths as peripheral nerves and are therefore said to be vulnerable to direct mechanical injury (Rydevik & Olmarker 1992).
There are five pairs of lumbar nerves, five pairs of sacral nerves and one pair of coccygeal nerves. Their dorsal and ventral nerve roots pass in the cauda equina in an infero-lateral direction to reach their appropriate level, before joining to emerge through the intervertebral foramina as the spinal nerves. Until the coccygeal level is reached there are several nerve roots passing vertically in the cauda equina (Fig. 13.7).
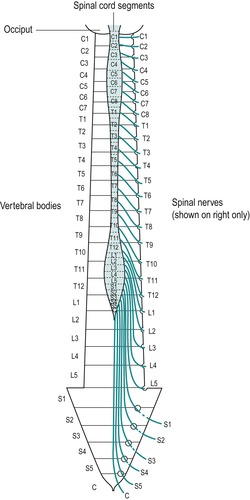 |
| Figure 13.7 The cauda equina and emerging nerve roots. From Functional Anatomy of the Spine by J Oliver and A Middleditch. Reprinted by permission of Elsevier. |
The clinical implications of this should be recognized as it is possible for a lumbar disc herniation to encroach on more than one nerve root. It also explains how a lumbar disc herniation could compress the S4 nerve root to affect bladder function.
DEGENERATIVE CHANGES IN THE LUMBAR SPINE
There is a suggestion that the intervertebral discs degenerate first and the subsequent reduction in the ability of the disc to distribute loads equally in all directions causes secondary degenerative changes in the zygapophyseal joints and ligaments (Acaroglu et al 1995, Prescher 1998). The degenerative process has been noted to be most predominant in the L4, L5 and L5, S1 levels but affects all levels of the lumbar spine, resulting in an overall reduction in spinal mobility (Prescher 1998) (Fig. 13.8).
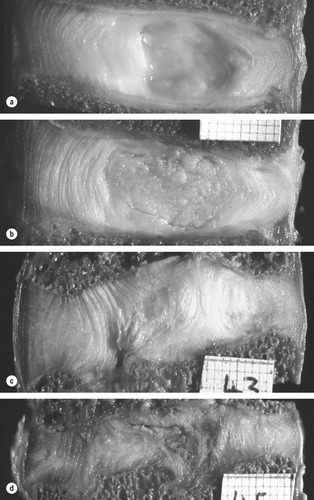 |
| Figure 13.8 Lumbar intervertebral discs sectioned in the mid-sagittal plane, anterior on left. These discs, which were not subjected to any post-mortem loading, represent the first four stages of disc degeneration. (a) Grade 1 disc, typical of ages 15–40 years. (Male 35 years.) (b) Grade 2 disc, typical of ages 35–70 years. The nucleus appears fibrous, and there is some brown pigmentation typical of ageing. However, the disc’s structure is intact and not ‘degenerated’. (Male, 47 years, L2–3.) (c) Grade 3 disc, showing moderate degenerative changes. Note the annulus bulging into the nucleus, damage to the inferior end-plate, and the lack of pigmentation in some regions of the disc. (Male, 31 years, L2–3.) (d) Grade 4 disc, showing severe degeneration. Note the brown pigmentation, the disruption to both end-plates, and internal collapse of the annulus, with corresponding reduction in disc height. (Male, 31 years, L4–5.) From The Biomechanics of Back Pain by M Adams, N Bogduk, K Burton and P Dolan. Reprinted by permission of Elsevier Ltd. |
The most marked ageing or degenerative changes occur in the nucleus of the intervertebral disc. There is a reduction in the water and proteoglycan content and a change in the number and nature of the collagen fibres, with the typical type II fibres of the nucleus changing to resemble the type I fibres of the annulus (Umehara et al 1996, Bogduk 2005, Paesold et al 2007). The gel-like appearance is lost as fibrocartilaginous tissue replaces the central portion of the disc and there is a resulting reduction in disc hydrostatic properties and flexibility (Paesold et al 2007). The water content of the nucleus reduces from 90% at birth to approximately 65–71% by the age of 75 and reduces the preloaded state of the disc (Jensen 1980, Taylor & Twomey 1994, Bogduk 2005). A strong familial predisposition for disc degeneration has been demonstrated through twin studies (Paesold 2007). In section the ageing nucleus pulposus develops the appearance of a dry, crumbling mass, changing in colour from the normal glassy greyish-blue towards yellow and brown – an observation that is sometimes referred to as ‘brown degeneration’ (Prescher 1998).
In losing some of its fluid properties, the nucleus is less able to exert a radial pressure on the annulus. Therefore, a greater portion of vertical load is supported by the annulus and the greater stresses contribute to circumferential tears and radial fissures. The lumbar discs become stiffer and less resilient and overall there is reduced mobility in the lumbar spine.
Cell proliferation has been observed in the degenerating nucleus, with lacunae formation (small spaces) containing multi-cell clusters, approximately half of which show signs of necrosis and others of apoptosis (programmed cell death). The outcome is cell loss from the disc (Paesold et al 2007).
Neovascularization of the inner portions of the disc has also been described, possibly accompanied by the growth of nerve fibres (Paesold et al 2007). This is an interesting development from the traditional understanding that the disc does not have its own blood supply and that only the outer third is innervated. Nerve growth factor has been identified exclusively in painful discs when compared to non-painful discs and is a possible mechanism of pain production. Direct treatment to inhibit its action could therefore be a possibility in the treatment of back pain. The need for further research is clear to be able to examine the interplay between neovascularization and neoinnervation, either or both of which could be of relevance regarding pain production and sensation in degenerate discs.
Degeneration affects the structure of the annulus, with a decrease in the number of lamellae. Individual lamellae become thicker and there is fraying, splitting and breakdown of the laminate structure with less evidence of a transitional zone between annulus and nucleus (Marchand & Ahmed 1990, Bernick et al 1991, Holm 1993, Acaroglu et al 1995). This degenerative process causes a change in the tensile properties of the annulus that affect its mechanical properties, as well as rendering it vulnerable to failure at lower stresses (Acaroglu et al 1995).
Three types of annular defect are noted (Osti & Cullum 1994):
• Rim lesions – discrete defects between the outer annulus and the vertebral body
• Circumferential tears – more common in the lateral and posterior layers
• Radial fissures – commonly seen in degenerating discs, extending from the nucleus.
Prescher (1998) explores the results of degeneration of the intervertebral disc material, suggesting that ‘dislocation’ of the annulus and/or the nucleus can occur, which may help in rationalizing the disc as a possible cause of spinal pain. The ‘dislocation’ may present as a ‘disc protrusion’ – a bulging of the disc in a posterior, lateral or anterior direction, which mainly involves nuclear material pushing outwards and stretching or ‘bulging’ the annular fibres. Since annular fibres contain nociceptive nerve endings, stimulation of these may produce primary discal symptoms.
If annular fibres tear, the pressurized nuclear tissue pushes outward through the defect, resulting in ‘disc prolapse’ where it may be responsible for compression or irritation of other pain-sensitive structures, resulting in secondary discal symptoms. The prolapsed tissue may be directed posteriorly, posterolaterally and anteriorly. If it detaches completely, it is referred to as ‘sequestrated’, when it may be directed further, either cranially or caudally. Posterolateral disc prolapse may encroach into the intervertebral canal and may compromise the emerging spinal nerve root, since the intervertebral disc is located at the same level as the emerging spinal nerve in the lumbar spine.
Bone density in the vertebral bodies reduces with age, causing weakening of the trabecular system, a loss of the horizontal trabeculae and a gradual collapse of the vertebral end-plate (Taylor & Twomey 1994, Prescher 1998). This results in the intervertebral disc bowing into the concavity of the weakened end-plate, with consequences for the nutrition of the disc via this route. A loss of overall height with ageing may not be due to a loss in disc height therefore, but to a loss in vertebral body height due to the collapse of the vertebral end-plate and subsequent migration of the discal material into the vertebral body (Taylor & Twomey 1994, Bogduk 2005). However, Prescher (1998) suggests that a pronounced decrease in disc height may result in adjacent spinous processes coming into contact with one another (‘kissing spines’) causing grinding, sclerotic changes and even pseudoarthroses.
Prescher (1998) also discusses degeneration, i.e. spondyloarthrosis of the zygapophyseal joints, suggesting that this particularly affects lumbar joints in patients over 30. Loss of disc height would appear to be the trigger, causing caudal migration of the inferior articular processes and a posterior displacement (or retrolisthesis) of the vertebral body. Advanced spondyloarthrosis may result in anterior displacement of the vertebral bodies, particularly L4, which occurs with the pars interarticularis intact. This phenomenon was noticed by Junghanns (cited in Prescher 1998) and was termed a pseudospondylolisthesis, occurring more frequently in females. This is a separate entity to a spondylolisthesis which affects L5 predominantly and occurs more commonly in males.
Lumbar lesions
Any structures in the lumbar region that receive a nerve supply can be a primary source of somatic pain. Congenital or acquired disorders of a single component of the motion segment cannot exist without affecting the functions of other components of the same segment and the functions of other segmental levels of the spine (Parke & Schiff 1971). However, Schwarzer et al (1994b) consider zygapophyseal joint pain to be uncommon, with discogenic pain a singular, independent disorder.
The zygapophyseal joints, as synovial joints, can be affected by arthritis and the presence of intra-articular structures makes derangement of the joint a possibility. The intervertebral disc is known to degenerate and since the outer annulus receives a nerve supply it can be a primary source of pain. Herniations of discal material are well recognized and are a secondary cause of pain, affecting other pain-sensitive structures.
Traction exerted on the dura and noxious stimulation of the back muscles, ligaments and lumbar zygapophyseal joints have both provoked a pain response (Bogduk 1994). Compression of normal nerves does not provoke a pain response while stimulation of swollen, stretched or compressed nerve roots has been shown to produce leg pain, with the dorsal root ganglion tending to be more tender than other parts of the nerve (Kuslich et al 1991). In the same study, stimulation of the outer annulus fibrosus and the posterior longitudinal ligament produced back pain while there was tenderness on stimulation of the capsule of the zygapophyseal joint, also associated with localized back pain. Pain may be produced in any pain-sensitive structure through chemical, mechanical or ischaemic mechanisms, although it seems more than likely that all factors coexist in disc pathology or herniation.
Chemical pain is the result of irritation of the noci-ceptive nerve endings by the products of inflammation, generally following tissue damage. The products of inflammation can either sensitize nerve endings so that they respond to a lower threshold of stimulus, or activate silent nociceptors (see p. 372) to provoke a response.
Mechanical pain occurs through stretching, compression or distortion of connective tissue structures stimulating the intervening nociceptors. Mechanical stress ultimately produces vascular changes and ischaemia, which activates nociceptors.
While acknowledging the existence of all pain-sensitive structures within the spinal joints, the discal model is central to the concepts of treatment in orthopaedic medicine. With evidence from scans more readily available, the disc would seem to be a major contributor to spinal pain, but the mechanisms of internal derangement, disc herniation and the recovery from disc pathology, often spontaneously, remain unknown. More recent work has concentrated on the chemical effects of displaced nuclear material, while the exact mechanism of pain produced by mechanical compression is unclear.
Primary disc pain
The outer part of the annulus fibrosus receives a nerve supply, some of which is thought to be nociceptive. Pressure exerted on the outer annulus and injection of contrast medium into the disc have each provoked a pain response (Bogduk 1994). Roberts et al (1995) found sensory nerve endings in the form of mechanoreceptors in intervertebral discs and the posterior longitudinal ligament. Golgi tendon organs were the most frequently seen. These may directly elicit pain or modulate muscle activity, perhaps in the form of muscle spasm that is often associated with lumbar lesions. Coppes et al (1997) established a more extensive disc innervation in severely degenerative human lumbar discs, when compared with normal discs, that invaded deeper than the outer third of the annulus. The nociceptive properties of some of the nerves were suggestive of substance P immunoreactivity.
As with all connective tissue structures, the elastic property of the collagen fibres in the annulus, enhanced by ‘crimp’, allows it to tolerate tensile forces. When placed under excessive mechanical tension the annulus deforms and may directly squeeze or distort pain-sensitive nerve endings, producing pain of mechanical origin. Once forces exceed normal limits microtrauma occurs, producing pain of chemical origin. The most vulnerable position for the annulus is when it is placed under rotational strains in flexion, ultimately resulting in circumferential splits (Bogduk 2005). Shear and tensile forces initiate damage at the peripheral portion of the disc but not at the centre, since fibre strain is always minimal at the centre and maximal at the periphery (Brinckmann 1986).
With consideration for the chemical contribution to low back pain, substance P causes the release of inflammatory mediators that affect the local environment and may sensitize nociceptors, resulting in chronic pain (Zimmermann 1992, Beaman et al 1993, Palmgren et al 1996). Substance P immunoreactive nerve fibres have been identified in the zygapophyseal joint capsule and synovial folds, the supraspinous ligament, posterior longitudinal ligament and the annulus fibrosus. Some fine unmyelinated and small myelinated fibres in the annulus are thought to serve as a type of pain fibre – termed silent nociceptor – that is not excited by mechanical stress, but responds to algesic chemicals produced at times of tissue damage or inflammation (Cavanaugh 1995).
There is no evidence as yet to support a nerve supply to the nucleus pulposus and pathological processes are thought to occur internally within the nucleus without provoking a pain response.
Secondary disc pain
Mixter & Barr (1934) suggested that a displaced fragment of the intervertebral disc into the vertebral canal causes mechanical compression of the lumbar nerve roots and sensory root ganglia. However, the mechanism by which back or leg pain is produced by this mechanical compression is still not fully understood. Kuslich et al (1991) demonstrated that stimulation of a normal nerve root did not produce a pain response, while stimulation of an already swollen, stretched or compressed nerve root produced leg pain. However, no suggestion was made for how much, or for how long, mechanical stress should be applied to a previously undamaged nerve root before changes occur to make it sensitive.
The extruded disc material in disc prolapse may consist of nuclear material, sometimes with end-plate material and occasionally elements of the annulus (Bogduk 1991, Brock et al 1992). However, normal disc material does not usually rupture and the nucleus is thought to undergo some process of deterioration or degradation, in order for it to be displaced (Bogduk 1991). Hormonal, nutritional or viral factors, or simply an acceleration of the degenerative process, have been proposed as possible reasons for the degradation of the nucleus.
Bogduk (2005) offers a plausible explanation of mechanical trauma together with an autoimmune reaction within the nucleus. Proteins in the nucleus may act as an antigen which, when exposed to the circulation for the first time, triggers an autoimmune response. Intrinsically, this can occur via contact with the circulatory plexus associated with the vertebral end-plate through microfracture due to compressive loading. The provoked autoimmune inflammatory response causes degradation of the nucleus which continues once the microfractures heal. Degrading the nuclear material in this way renders it capable of herniation. Changes must also occur within the annulus since herniation of nuclear material can only occur through a radial fissure in a weakened annular wall (Brinckmann 1986).
The posterolateral corners of the annulus are irregular, thin and potentially weak (Umehara et al 1996). Radial fissures and circumferential splits commonly develop here, providing an escape route for the degraded nuclear material, when a force is applied sufficient to expel it. Flexed postures, especially combined with rotation, trigger backwards herniation of the nuclear material through a weakened annular wall (Bogduk 2005).
As well as being a primary source of pain, the prolapsed disc can have a secondary effect on any pain-sensitive structure lying within the vertebral canal or intervertebral foramen. This effect can be mechanical through compression and distortion, chemical through the inflammatory process and ischaemic through the pressure of oedema.
Once discal material enters the vertebral canal it may again be treated as foreign and stimulate an extrinsic autoimmune inflammatory response as it comes into contact with the circulation in the vertebral canal. The resulting chemical mediators affect adjacent pain-sensitive structures. If the prolapsed fragment is small, it will be dealt with by the macrophage system; if large, the inflammatory process continues until the fragment is eventually organized into scar tissue (Hirabayashi et al 1990).
Both mechanical and inflammatory mechanisms can produce ischaemia. The inflammatory mediators produced are thought to have a role in somatic pain (McCarron et al 1987, Bogduk 1994) and in radicular pain (Doita et al 1996, Kang et al 1996, Takahashi et al 1996, Greening 2004). Peng et al (2007) use the term ‘chemical radiculo-pathy’ to describe the irritation of nerve roots by inflammatory mediators travelling into the epidural space following disruption of the annulus.
The quality of pain seems to be instrumental in distinguishing somatic and radicular pain. Somatic referred pain is produced when any sensitive structure is stimulated and is deep, aching and hard to localize. Radicular pain is produced when a nerve root is compressed or irritated and was described by Smyth & Wright, cited in Bogduk (2005), as shooting, lancinating pain felt in a relatively narrow band, approximately 4 cm wide, into the limb (see Ch. 1).
Compression of undamaged nerves produces numbness, paraesthesia and muscle weakness. Under some circumstances, which are not well understood, compression alters nerve root conduction and compromises nutritional support, causing the nerves to become pain-sensitive through inflammation, ischaemia or both (Garfin et al 1995). Studies suggest that the products of the auto-immune inflammatory process stimulated by the displaced discal material may increase the sensitivity of the nerve root to bradykinin and be involved in the pathophysiology of radiculopathy (Saal 1995, Kang et al 1996, Takahashi et al 1996).
The mechanical effects of compression of a nerve root may be direct or more probably indirect through ischaemia. A sequence of events may be induced involving impairment of nutrition and increased microvascular permeability, leading to intraneural oedema, blockage of axonal transport and altered function (Rydevik & Olmarker 1992). For referred leg pain to be radicular in origin, arising from compression of a nerve root, it must be accompanied by other signs of compression – paraesthesia and muscle weakness. If these are absent, pain referred to the limb must be somatic in origin (Bogduk 2005).
However, in clinical practice, signs and symptoms of somatic and radicular pain coexist since, for a disc protrusion to compress a nerve root, it must first compress and stimulate nerve endings in its dural nerve root sleeve. Thus the dural nerve root sleeve produces somatic referred pain, either mechanical or chemical in origin, while the nerve root may produce radicular pain and other signs and symptoms of nerve compression.
In studies on peripheral nerves, a critical level of pressure is significant for structural and functional changes to occur and longer periods of compression would seem to be responsible for more damage (Jancalek & Dubovy 2007). Prolonged compression may produce changes in axonal transport impairing the transport of proteins from the nerve cell body to the distal parts of the body and resulting in compression-induced effects in the distal axonal segment (double crush syndrome).
The trauma evoked by compression may alter the permeability of the intraneural vessels, resulting in oedema. The oedema usually persists after removal of the compression and therefore may adversely affect the nerve root for longer. The presence of intraneural oedema is thus related to intraneural fibrosis and adhesion formation.
Unfortunately, at the time of writing, there do not appear to have been many experimental studies on spinal nerves, but they are known to be more susceptible to compression than peripheral nerves since they do not have the same protective connective tissue sheaths. The critical pressure levels for compression to induce impairment of nerve nutrition or function are not known, or the length of time that compression needs to be applied before changes occur and they become pain-sensitive.
Huang et al (2007) describe that traction injuries to the dorsal nerve root can avulse the sensory axons, e.g. cauda equina which cannot regenerate through axonal regrowth from the dorsal root ganglion into the spinal cord. There is a divide between the central nervous system (CNS) and the peripheral nervous system (PNS), the transition zone. Regeneration cannot occur backwards from the PNS to the CNS and, since the nerve roots themselves are components of the PNS, this has considerable significance if disruption of the S4 nerve root is suspected.
Differential diagnosis at the lumbar spine
The mechanism by which the lumbar intervertebral disc produces pain is probably complicated, with several factors contributing to the diagnosis. It is important to understand the anatomy and the possible mechanisms for pain production, as discussed above.
Patients with non-mechanical causes of back pain can present with signs and symptoms that mimic those of disc pathology. It is important to recognize those features that allow them to be identified as ‘red flags’ (indicators of serious spinal pathology), since manual techniques are either contraindicated or not appropriate, and the patient needs to be referred to the appropriate specialist.
Mechanical lumbar lesions
A recap of the terminology used to describe disc herniation is provided below to add clarity to the following discussion. In contrast to the cervical spine, where the degenerate disc tends to displace as a central bar-like protrusion of the annulus, the degenerate lumbar disc involves degradation and herniation of nuclear material through a weakened annular wall. This herniation may occur as a protrusion into the weakened annulus where it may produce primary disc pain, or as a prolapse where nuclear material moves into the vertebral canal. Here it can have a secondary effect on any pain-sensitive structure by mechanisms involving compression, inflammation and ischaemia.
A central prolapse affects central structures, in particular the posterior longitudinal ligament and the dura mater. Pain arising from compression of the dura mater is multisegmental in nature (see Ch. 1). A posterolateral prolapse affects unilateral structures, mainly the dural nerve root sleeve and nerve root, which tend to produce segmental pain.
A disc herniation, either protrusion or prolapse, produces a pattern of signs and symptoms that are progressive, with a history of increasing, worsening episodes. Often the precipitating factor is trivial. The dural nerve root sleeve and nerve root are vulnerable in the lumbar spine to posterolateral prolapse, with pain and other associated symptoms referred into the leg. A classification of clinical models has been established to aid diagnosis and to establish treatment programmes. These are outlined in the treatment section later in this chapter, since they relate directly to treatment selection.
Disc protrusion
• Degenerate disc material bulges into the weakened laminate structure of the annulus, where it can produce primary disc pain since the outer annulus receives a nerve supply.
Disc prolapse
• Discal material passes through a radial or circumferential fissure in the annulus which provides it with an escape route into the vertebral canal where it has a secondary effect on the pain-sensitive structures in the vertebral canal. The sequela of this is sequestration of the disc.
Other causes of back pain, leg pain and associated signs and symptoms
Non-mechanical lesions, including serious pathology, have features that do not ‘fit’. Since they represent contraindications to manual orthopaedic medicine treatments, they must be recognized and the patients referred appropriately.
Arthritis, in any form, presents with the capsular pattern which is demonstrated by the lumbar spine as a whole.
• Degenerative osteoarthrosis affects the intervertebral joint and the zygapophyseal joint. The consequences of degeneration and degradation of the intervertebral disc lead to increased possibility of disc herniation. Disruption of the intervertebral joint affects the zygapophyseal joint, causing the joint surfaces to bear increased weight.
• Osteophytes may form at the peripheral margins of the disc, possibly in association with rim lesions of the annulus, as well as at the zygapophyseal joints. Overall the degenerative changes may lead to spinal stenosis.
• Spinal stenosis is a term that has become synonymous with neurogenic or spinal claudication. It should be used to define any symptomatic condition in which limited space in the vertebral canal is a significant factor (Porter 1992). Lateral stenosis affects the nerve root; central stenosis affects the spinal cord or cauda equina and may coexist with lateral stenosis.
Some patients have a developmental abnormality where the spinal canal has a trefoil shape in cross-section (Vernon-Roberts 1992) and spinal stenosis is particularly prevalent in this group. Narrowing can also occur as a result of degenerative changes through ageing, injury, disease, or as a result of surgery (Lee et al 1995). Irrespective of cause, a small vertebral canal can have clinical significance for back pain (Porter & Oakshot 1994).
Degenerative spinal stenosis can be associated with osteophyte formation at the vertebral body or zygapophyseal joints, with reactive proliferation of capsular and soft tissues, and fibrous scarring around the nerve roots. The vertebral canal can be compromised by thickening of the ligamentum flavum which shows a 50% increase in thickness with ageing over a normal lifespan (Twomey & Taylor 1994). Degenerative spondylolisthesis may also narrow the canal (Osborne 1974, Rauschning 1993).
A disc prolapse may significantly reduce the size of both the vertebral and intervertebral foramina and Porter et al (1978) noted that the risk of developing disabling symptoms from disc prolapse is inversely related to the size of the spinal canal. The anterior margin of the canal can be indented to compress the cauda equina by a lax posterior longitudinal ligament overlying degenerate prolapsed discs. Cyriax (1982) termed this the ‘mushroom phenomenon’.
Spinal stenosis can produce neurogenic or spinal claudication which was recognized by Verbiest, in 1954, as due to structural narrowing of the vertebral canal compressing the cauda equina and producing claudication symptoms (Porter 1992). Men over the age of 50 with a lifestyle that has involved heavy manual work may be affected. The entire cauda equina can be compressed centrally causing bilateral symptoms, or the emerging nerve root can be affected (Osborne 1974). The patient complains of discomfort, pain, paraesthesia and heaviness in one or both legs while standing or walking. There may be night cramps and restless legs. A long history of back pain may be present and the patient may have undergone back surgery at some time. The symptoms are usually of several months’ duration. There is usually a threshold distance when the symptoms develop and a tolerance when they have to stop; the tolerance distance is about twice the threshold (Porter 1992). These symptoms are similar to those of the ischaemic pain associated with intermittent claudication of peripheral vascular disease and with the age group affected; the two conditions can coexist, making diagnosis difficult.
With neurogenic claudication, stooping or bending forwards relieves the symptoms and allows the patient to continue. Flexion increases the space in the canal and tightens the ligaments, straightening out the buckling that tends to occur with degeneration. The patient can usually walk uphill, which involves a flexed posture, easier than walking downhill, which involves an extended posture.
On examination, the patient often stands with a stooped posture, with flexed hips and knees and a flattened lumbar spine with loss of the lordosis. This posture becomes more evident on walking. The capsular pattern is present with marked loss of spinal extension. Extension may produce the pain as it decreases the calibre of the spinal canal while, conversely, flexion relieves the pain (Osborne 1974). Dynamic variations in flexion and extension are related to changes in the buckling of the ligamentum flavum and the herniation of the intervertebral discs (Rauschning 1993). The rest of the examination may be unremarkable and back pain itself may not be a feature. Neurological signs are often absent.
Management may involve spinal decompressive surgery or advice on how to live with the condition. Symptoms do not usually resolve, but they do not always get worse.
Kotil & Bilge (2007) report on two cases of haematoma in the ligamentum flavum as a rare cause of low back and leg pain in elderly patients. The signs were consistent with L5 root compression. A cautious approach is required for leg pain in the elderly, especially as a first presentation. Full consideration should be given to the entire clinical presentation and further investigation is wise if there is any suspicion that the cause is non-mechanical.
• Rheumatoid arthritis can affect the spinal joints and this has been covered in Chapter 8. Ankylosing spondylitis is discussed in Chapter 14.
Structural abnormalities can be completely asymptomatic or may produce pain, inflammation and neurological signs, or coexist with disc herniation.
• Spondylolysis is a defect in the pars interarticularis (the neural arch between the lamina and the pedicle) of L5 and sometimes L4.
• Spondylolisthesis is an anterior shift of one vertebral body on another, usually involving slippage of L5 on S1. It may be congenital, acquired through degeneration, trauma, or as a sequela to spondylolysis. It is commonly associated with over-training in such sports as gymnastics, involving hyperextension, and the rotational stresses involved in fast bowling (Bush 1994). If symptomatic, the main symptom is back pain that may be referred to the buttocks. The pain is aggravated by exercise and standing and is eased by sitting. Inspection may reveal excessive skin folds above the defect and a step defect may be felt on palpation (Norris 2004). On examination, extension is limited and painful and passive overpressure of the affected vertebra produces the pain.
Diagnosis is confirmed by oblique X-rays that show the typical ‘Scottie dog’ view. If the ‘Scottie dog’ is wearing a collar, there is a defect in the pars interarticularis and the patient has spondylolysis. If the head of the ‘Scottie dog’ is separated from the neck, the patient has spondylolisthesis.
X-ray assesses the degree of spondylolisthesis which is measured by the distance the slipped upper vertebra moves forward on its lower counterpart. Slippage is divided into four degrees, progressing from a first-degree slip, which is a forward displacement of one quarter of the anteroposterior diameter of the vertebral body, to a fourth-degree slip with a full anteroposterior diameter displacement (Corrigan & Maitland 1983).
A particular feature of serious non-mechanical conditions is an unwell patient with possible weight loss. Neoplasm of the lumbar spine, although relatively uncommon, should be considered as a possible cause of low back and leg pain. Metastases may be secondary to carcinoma of the bronchus, breast, ovary, prostate, thyroid or kidney. Metastatic invasion may involve bone or may be intradural. Primary bone tumours occasionally affect the posterior elements of the vertebrae and multiple myeloma can produce backache due to vertebral involvement.
• Neoplasm involving the lumbar spine may be clinically silent or may produce pain in isolation or cause associated neurological deficit (Findlay 1992). The pain may be due to compression or distortion of pain-sensitive structures and/or to destructive changes in the bone. Neurological deficit is usually of a lower motor neuron type and it may begin either at the same time as the pain or prior to it.
The pain of neoplastic disease has characteristic features. It is usually deep-seated, boring, relatively constant, steadily worsening and often persistent at night. If there is collapse of the vertebral body, the pain will be associated with movement and activity due to the spinal instability (Findlay 1992). Aside from night pain, symptoms of weakness, fatigue and weight loss should be considered to be serious in a patient complaining of back pain.
The signs and symptoms of a tumour can mimic a disc lesion. Palma et al (1994) reported three cases of neurinoma of the cauda equina initially misdiagnosed as a disc lesion. Pain which worsens during recumbency and improves in sitting and walking, together with bilateral, multiple root involvement, is more indicative of an expanding lesion in the cauda equina than sciatica. Unusual cases of a primary extraosseous Ewing sarcoma in a 15-year-old girl with a history of chronic back and leg ache (Allam & Sze 1994) and primary Hodgkin’s disease of the bone presenting clinically with an extradural tumour (Moridaira et al 1994) exist in the literature.
• Infection may cause osteomyelitis or discitis and epidural abscess is possible. Pyogenic organisms, e.g. Staphylococcus aureus, Myobacterium tuberculosis or, rarely, Brucella, may be responsible (Kumar & Clark 2002). The clinical presentation of spinal infection varies from a complaint of back pain only, to being very ill, emaciated and febrile and with a raised erythrocyte sedimentation rate. On examination tenderness is elicited on percussion of the affected vertebra and widespread muscle spasm may be present. X-ray may show loss of bony contour, cavitation and collapse and possibly an associated paravertebral abscess (Kemp & Worland 1974).
• Aortic aneurysms are commonly abdominal (Kumar & Clark 2002). When they rupture they may present with epigastric pain that radiates through to the back. The patient is shocked and a pulsatile mass is felt. This situation is a medical emergency. Galessiere et al (1994) presented three cases of chronic, contained rupture of aortic aneurysms associated with vertebral erosion. The patients presented with a history of chronic backache.
Non-organic back pain should be considered at the lumbar spine, although true psychogenic back pain is rare. Anxiety tends to be associated with acute back pain while depression is associated with chronic back pain; both are indicators of the patient’s distress. Back pain may begin as a physical problem and, as such, is generally addressed by mechanical or physical treatments. If low back pain becomes chronic, psychosocial factors may be more obvious than physical signs, and illness behaviour becomes a relevant component. Illness behaviour is a normal phenomenon and a physical problem exists with varying degrees of illness behaviour (Waddell 1998). As clinicians, the physical and psychosocial factors that coexist in chronic pain must therefore be understood in order to provide total care. The interested reader is referred to the work of Waddell (1998) which includes the biopsychosocial model and describes non-organic or behavioural signs, the so-called ‘yellow flags’, as indicators of pychological distress and risk of long-term disability.
COMMENTARY ON THE EXAMINATION
Observation
A general observation of the patient’s face, posture and gait will alert the examiner to the seriousness of the condition. Patients in acute pain will generally look tired. They may have adopted an antalgic posture of flexion or lumbar scoliosis which is generally indicative of an acute locked back, possibly due to a disc lesion. A lumbar lateral shift is pathognomic of a disc lesion (Porter 1995). Patients may not be able to sit during the examination due to discomfort from this particular posture. Their gait may be uneasy with steps taken cautiously, obviously wary of provoking twinges of pain by sudden movements or pain on weight-bearing. A dropped foot may be evident on walking and will lead you to consider involvement of the L4 nerve root affecting the tibialis anterior muscle and interfering with function.
The Box on page 379 lists the ‘red flags’ for the possible presence of serious pathology that should be listened for and identified throughout the subjective and objective examination. In isolation, many of the flags may have limited significance but it is for the clinician to consider the general profile of the patient and to decide whether contraindications to treatment exist and/or whether onward referral is indicated.
History (subjective examination)
The history is particularly important at the spinal joints. Vroomen et al (1999) published a systematic review of the diagnostic value of the history and examination of patients with suspected sciatica, establishing that very little attention has been paid to the history of such events. Pain distribution was the only sensitive sign of the level of disc herniation, with straight leg raising seemingly a sensitive sign and crossed straight leg raise a strong indicator of nerve root compression. Disagreement exists in the literature with regard to the value of decreased muscle strength, sensory loss and altered reflexes as signs of nerve root involvement and it is unclear whether the physical examination adds much to the diagnostic value of the history.
There is a close relationship between signs and symptoms from the lumbar spine, sacroiliac joint and hip joint. The history will help with the differential diagnosis but conditions at each of these areas can coexist. Major pathology can affect the spine, such as malignancy, infection, spondyloarthropathy or fracture, but these represent a small percentage of the problems compared with mechanical lesions of the lower back (Swezey 1993). X-ray findings can be misleading, particularly when showing the degenerative changes of osteoarthrosis which may or may not be painful. Similarly, spondylolysis progressing to spondylolisthesis occurs in approximately 5% of adults but is symptomatic in only half of them (Swezey 1993).
The age, occupation, sports, hobbies and lifestyle of the patient may give an indication of provoking mechanisms. Often the incident precipitating the episode of back pain may be relatively minor, though factors predisposing to the event may have been continuing for some time. While cure will be the initial aim of treatment for this presenting incident, ultimately the management of the condition and prevention of recurrence will become the patient’s responsibility. Patients will require advice and guidance on management of their back condition to prevent chronicity.
Many occupations involve a flexion lifestyle, e.g. sedentary office work and brick-laying apply postural stress to the intervertebral joint. These patients require advice about changing postures to minimize the stress inflicted by work. Directives on the manual handling of loads are in existence and patients should receive advice about this in their place of work. The vibration of motor vehicle driving may have an influence, as well as the sitting posture involved, which is known to increase intradiscal pressure (Osti & Cullum 1994).
Assessment of patients with chronic low back pain presents a particular challenge to the clinician. Emotional, environmental and industrial factors may influence pain perception, while monotony or dissatisfaction at work or home is relevant (Osti & Cullum 1994). Distinction will need to be made between the true physical symptoms of the presenting condition and those relating to psychosocial factors that influence the way the patient reacts to the pain (see above). Enquiry should be made about the possibilities of secondary gain factors relating to disability, or the presence of psychological or social stresses that might predispose the patient to chronic pain disorders (Swezey 1993). Standard questions on quality of sleep, tiredness levels, concentration, appetite, etc. may establish whether the patient is depressed.
The site of the pain will give an indication of its origin (see Ch. 1). Lumbar pain is generally localized to the back and buttocks or felt in the limb in a segmental pattern. Sacroiliac pain may be unilateral, felt in the buttock, or more commonly in the groin, and occasionally referred into the leg. The hip joint may produce an area of pain in the buttock consistent with the L3 segment, pain in the groin, or pain referred down the anteromedial aspect of the thigh and leg to the medial aspect of the ankle. Dural pain is multisegmental and will be central or bilateral. Pressure on the dural nerve root sleeve will be referred segmentally to the relevant dermatome. Pressure on the nerve root will refer pain to the relevant limb with accompanying symptoms of paraesthesia at the distal end of the dermatome.
Vucetic et al (1995) considered the difficulty that patients have in giving a precise verbal description of pain. They support the use of a pain drawing, which may take a few minutes to obtain, but the result can be grasped at a glance. Waddell (1992) warns that how a patient draws pain is influenced by emotional distress and that non-anatomical, widespread and magnified drawings tell of the patient’s distress rather than the physical characteristics of the pain.
The spread of pain will not only give an indication of its origin, but also the severity or irritability of the lesion. Generally, the more peripherally the pain is referred, the greater the source of irritation. A mechanical lesion due to a displaced lumbar disc produces central or unilateral back or buttock pain. If the pain shifts into the leg, it generally ceases or is reduced in the back. Pain of non-musculoskeletal origin does not follow this pattern and serious lesions produce an increasing spreading pain, with pain in the back remaining as severe as that felt peripherally.
The onset and duration of the pain can assist the choice of treatment (see below). In very general terms, a sudden onset of pain may respond to manipulation, while a gradual onset of pain may respond better to traction. The whole clinical picture will need to be reasoned through in order to make a decision about treatment, which may contradict these rules of thumb.
The nature and mode of onset are important. The patient may remember the exact time and mode of onset which may have involved a flexed and rotated posture. If lifting was involved in the precipitating episode, it may only have been a trivial weight. If the patient reports a gradual onset of pain, it is worth questioning further for details of previous activity. A minor traumatic incident some time before the onset of back pain or the maintenance of a sustained flexion posture may have been sufficient to provoke the symptoms.
The gradual onset of degenerative osteoarthrosis is common in the zygapophyseal joints and hip joints, while a subluxation of the sacroiliac joint can occur with a sudden onset. Serious pathology develops insidiously.
If trauma is involved, the exact nature of the trauma should be ascertained and any possible fracture eliminated. Direct trauma may produce soft tissue contusions, while fracture may involve the spinous process, transverse process, pars interarticularis, vertebral body or vertebral end-plate. Compression fractures of the vertebral body are common in horse riders and those falling from a height, and involve the vulnerable cancellous bone of the vertebral body (Hartley 1995). Hyperflexion injuries may cause ligamentous lesions or involve the capsule of the zygapophyseal joint, while hyperextension injuries compress the zygapophyseal joints. Both forces can injure the intervertebral disc.
The symptoms and behaviour need to be considered. The behaviour of the pain will give an indication of the irritability of the patient’s condition and provide clues to differential diagnosis. Serious pathologies of the spine, including fractures, tumours or infections are relatively rare, accounting for less than 1% of all medical cases seen for spinal assessment. Despite this, the clinician must remain alert to clinical indicators that need more extensive investigation than the basic clinical examination (Sizer et al 2007).
The pattern of all previous episodes of back pain should be ascertained, as in disc lesions a pattern of gradually worsening and increasing episodes of pain usually emerges.
The mechanisms whereby the disc herniation can cause pain have been discussed earlier in this chapter. The typical pattern of pain from disc herniation is usually one of a central pain which moves laterally. As the pain moves laterally, the central pain usually ceases or reduces. A gradually increasing central pain accompanied by an increasing leg pain is indicative of serious pathology and this pain is usually not altered by either rest or activity.
The daily pattern of pain is important and typically a disc lesion produces either a pattern of pain that is better first thing in the morning after rest, becoming worse as the day goes on, or, since the disc imbibes water overnight, the patient may experience increased pain on weight-bearing first thing in the morning due to increased pressure on sensitive tissues. Patients can sleep reasonably well at night as they are usually able to find a position of ease.
Mechanical pain can cause an on/off response through compression or distortion of pain-sensitive structures. This can involve the annulus itself or structures in the vertebral canal. The patient with a disc lesion usually complains of pain on movement easing with rest. Changing pressures in the disc affect the pain and it tends to be worse with sitting and stooping postures than when standing or lying down. In an acute locked back, small movements can create exquisite twinging pain.
Herniated disc material may produce an inflammatory response resulting in chemical pain. Chemical pain is characteristically a constant ache associated with morning stiffness. Sharper pain can also be associated with chemical irritation as the nerve endings become sensitized and respond to a lower threshold of stimulation. It is important to differentiate mechanical back pain from inflammatory arthritis and sacroiliac joint lesions through consideration of other factors, since they also produce pain associated with early-morning stiffness.
Radicular pain is generally a severe lancinating pain, often burning in nature, which is felt in the distribution of the dermatome associated with the nerve root. Sciatica is commonly associated with lumbar disc pathology and will occur if the L4–L5, S1 or S2 nerve roots are involved. If the higher levels are involved, pain will similarly be referred into the relevant segment.
The language used by patients to describe the quality of their pain will indicate the balance between the physical and emotional elements of their pain. Words such as ‘throbbing’, ‘burning’, ‘twinging’ and ‘shooting’ describe the sensory quality of the pain; emotional characteristics are expressed in such words as ‘sickening’, ‘miserable’, ‘unbearable’ and ‘exhausting’ or vocal complaints such as moans, groans and gasps (Waddell 1992, 1998).
The other symptoms described by the patient provide evidence for differential diagnosis, contraindications to treatment and the severity or irritability of the lesion. An increase in pressure through coughing, sneezing, laughing or straining can increase the back pain and this is the main dural symptom. Paraesthesia is usually felt at the distal end of the dermatome and is a symptom of nerve root compression. Confirmation of this is made through the objective compression signs of muscle weakness, altered sensation and reduced or absent reflexes.
Specific questions must be asked concerning pain or paraesthesia in the perineum and genital area as well as bladder and bowel function. The presence of any of these symptoms indicates compression of the S4 nerve root at the preganglionic extent which could produce irreversible damage, and indicates immediate referral for surgical opinion. A transition zone exists in the preganglionic region between the peripheral and central nervous systems and repair cannot occur across the transition zone if the nerve is disrupted (Huang et al 2007). This study examines the possibility of surgical repair of the nerve to encourage regeneration but the repair has been performed in rats only at this stage.
Manipulation is absolutely contraindicated in these cases. The symptoms of difficulty in passing water, inability to retain urine or lack of sensation when the bowels are opened are important. It is not unusual to find urinary frequency or difficulty in defecating associated with effort in hyperacute lumbar pain.
Bilateral sciatica with objective neurological signs and bilateral limitation of straight leg raise suggest a massive central protrusion compressing the cauda equina through the posterior longitudinal ligament, with possible rupture of the ligament (Cyriax 1982). It is an absolute contraindication to manipulation, since a worsening of the situation could lead to irreversible damage to the cauda equina, as mentioned above. The symptoms of cauda equina compression should be distinguished from multisegmental, dural reference of pain into both legs, where there may be bilateral limitation of straight leg raise but no neurological signs.
Questioning the patient about other joint involvement will indicate whether inflammatory arthritis exists or if there is a tendency towards degenerative osteoarthrosis.
The past medical history and the patient’s current general health will help to eliminate possible serious pathology, past or present. An unexplained recent weight loss may be significant in systemic disease or malignancy. Visceral lesions can refer pain to the back, e.g. kidney, aortic aneurysm or gynaecological conditions. Infections should be obvious, with an unwell patient showing a fever. Malignancy can affect the lumbar and pelvic region but the pattern of the pain behaviour does not generally fit that of musculoskeletal origin. Past history of primary tumour may indicate secondaries as a possible cause of back pain. Serious conditions produce an unrelenting pain; night pain is usually a feature and is responsible for the patient looking tired and ill. As well as past medical history, establish any ongoing conditions and treatment. Explore other previous or current musculoskeletal problems with previous episodes of the current complaint, any treatment given and the outcome of treatment.
The medications taken by the patient will indicate their current medical state as well as alerting the examiner to possible contraindications to treatment. Anticoagulant therapy and long-term oral steroids are contraindications to manipulation. It is useful to know what analgesics are being taken and how frequently. This gives an indication of the severity of the condition and can be used as an objective marker for progression of treatment, with the need for less analgesia indicating a positive improvement. If patients are currently taking antidepressant medication, this may indicate their emotional state and possibly exclude them from manipulation. Care is needed in making this decision, however, since antidepressants can be used in low doses as an adjunct to analgesics in back pain.



 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

• Young: Under 20
• Elderly: First episode over 55
• Violent trauma
• Past medical history of malignancy
• Constant progressive pain
• Cauda equina syndrome
• Unremitting night pain
• Systemically unwell
• Unexplained weight loss
• Drug abuse and HIV
• Long-term systemic steroid use
• Widespread neurological signs and symptoms
• Gait disturbance
• Thoracic pain
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








