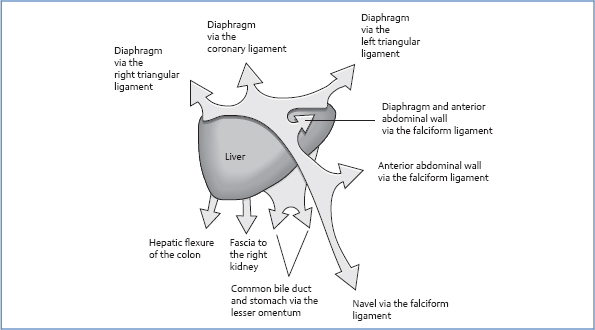
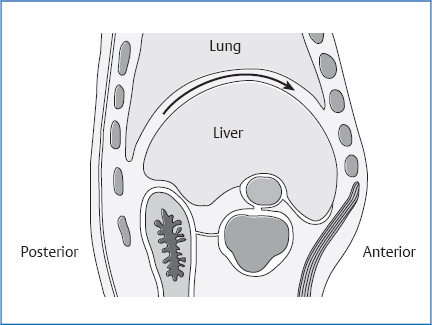
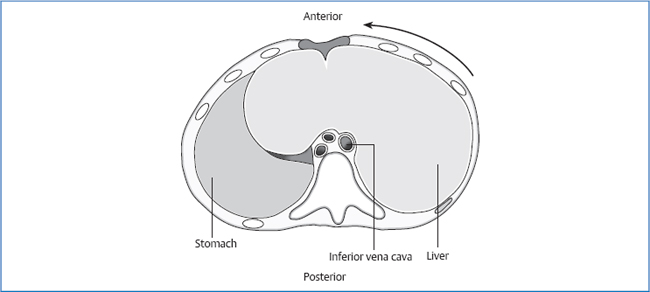
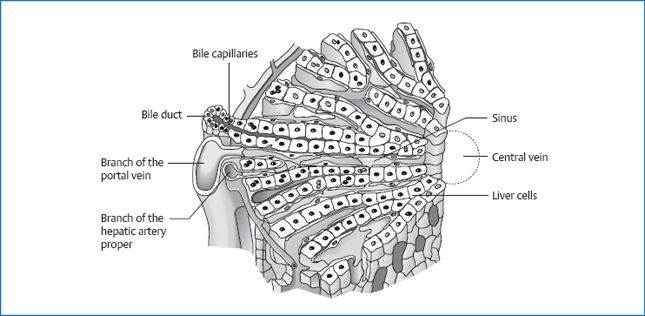
II Osteopathy of the Individual Organs 16 The Uterus/Fallopian Tubes/Ovaries Macroscopic subdivision of the liver is into: The liver is covered by peritoneum, except for the “bare area,” which is directly connected to the diaphragm. It weighs about 1.5–2.5 kg, although the effective weight is only about 400 g because the gravitational force of the thoracic organs (vacuum in the thorax), on the one hand, and the abdominal organ pressure, on the other, reduce it. Blood flow through the liver is about 1.5 L/min. The liver is located in the right upper abdomen below the diaphragm. Fig. 5.1 Attachments of the liver. Hepatic artery proper from the celiac trunk. The lymphatic vessels run parallel to the blood vessels. Maximal time: 1–3a.m. Minimal time: 1–3p.m. Organs and teeth have a relationship to each other that is comparable to the system of connective tissue zones on the back or the foot reflex zones. Disorders or even just functional disturbances of an organ are reflected in the weakening of a tooth, the adjoining gum, or the nearby mucous membranes. The tooth can hurt without a corresponding lesion being present. Likewise, it is possible that the tooth, gums, or mucous membranes are inflamed. Similarly, a damaged tooth also affects the corresponding organ. This can reach the point where an organic disturbance can be cured only after the tooth or gums have healed up. For osteopaths, it is therefore important to know the interrelationships of each organ and tooth, and to take countermeasures against misdiagnoses and mistreatments early on. For this reason, the tooth associated with the organ is identified here. In this context, always remember that the adjoining gum and mucous membranes are part of this relationship as well. The liver displays mobility in three planes, as follows. Fig. 5.2 Mobility and motility of the liver in the frontal plane. During inhalation, the diaphragm leads the lateral parts of the liver inferiorly to medially. Looked at from the front, the liver rotates in a counterclockwise direction. The axis of movement is a sagittotransverse axis through the left triangular ligament. In this plane, the liver tilts with the cranial parts anteriorly while at the same time shifting the caudal edge posteriorly. The frontotransverse axis of movement runs approximately through the coronary ligament. Fig. 5.3 Mobility and motility of the liver in the sagittal plane. The liver carries out a leftward rotation along a frontosagittal axis through the inferior vena cava as an approximate anatomic landmark. Looked at from above, this is a counterclockwise rotation. The motions of motility correspond in direction and axis to those of mobility. Fig. 5.4 Mobility and motility of the liver in the transverse plane. The liver metabolizes all three basic elements of food (carbohydrates, fats, and proteins) in different ways, therefore playing a dominant role in intermediary metabolism. Definition. The deposition of bilirubin causes a yellow coloration in blood plasma and connective tissue. With regard to connective tissue, the sclerae turn yellow first, followed by the skin. This phenomenon occurs when the concentration of bilirubin in the plasma exceeds 0.30–5 mmol/L. Types Fig. 5.5 Microscopic anatomy of the liver. The oxygenrich blood from the branch of the hepatic artery proper and the oxygen-deficient but nutrient-rich blood from the portal vein together flow into the central vein. The numerous metabolic processes of the liver take place in the liver cells. The cells receive the necessary oxygen and “building blocks” from the mixed blood in the sinus of the liver. Definition. Infection of the body with a pathogenic virus that affects the liver cells. Infection. The hepatitis A virus (HAV) is most often transmitted fecally or orally, although sexual or perinatal transmission is also possible. One risk factor is traveling to southern vacation areas: even in Europe, a clear north-south divide exists in the spread of hepatitis A infection. Clinical. The period of incubation is 14–40 days. Most frequently, we see a prodromal stage with flulike and gastrointestinal symptoms (feeling of fullness, lack of appetite, nausea, diarrhea, fever, joint pain). This is followed by the organ manifestation with icterus, sensitivity to pressure in the liver, signs of liver cell degradation, and in a fifth of all cases splenomegaly. The course of the disease is an average of 4–8 weeks; life-long immunity remains. This type has neither virus carriers nor chronification. Infection. In the case of the hepatitis B virus (HBV), the path of transmission is parenteral (plus needle puncture wounds), sexual contact, or perinatal. Worldwide, about 200 million people are infected. Clinical. The period of incubation is 60–120 days. A nonspecific preliminary stage can be missing; organ manifestation runs a much more serious and drawn-out course than in hepatitis A. Nevertheless, most hepatitis B infections are asymptomatic. In 5–15% of infections, the acute form turns into the chronic form, which can lead to cirrhosis of the liver or a primary liver cell carcinoma. The disease takes a lethal course in 2–15% of all cases, but there are also healthy and infectious virus carriers. Active immunization is advised. Infection. The delta virus is attached to the B virus and utilizes parts of the HBV for its own reproduction. The path of infection is parenteral or by sexual contact. Endemic regions are southern Italy, the Balkans, the Near East, Africa, and South America. Clinical. The period of incubation for simultaneous infection with HBV is 12–15 weeks. If a patient with persistent HBV is infected, the incubation period is clearly shorter, around 3 weeks. The infection entails a serious negative effect on the liver, and not uncommonly also liver failure. Approximately 80% of hepatitis D virus (HDV) infections become chronic. Protection against this infection is achieved by immunization against HBV. Infection. The hepatitis C virus (HCV) is spread via injection or sexual transmission. It is found in 0.5–1.5% of all blood donors. Anti-HCV is clearly more common in people who have experienced an HBV infection. Clinical. The period of incubation is 5–12 weeks. Asymptomatic courses are possible. Nevertheless, 50% of infections take a chronic course, and transition to cirrhosis or hepatocellular carcinoma is not uncommon. There is no immunization. Infection. The path of transmission for the hepatitis E virus (HEV) is fecal-oral. In developing countries, it is held responsible for epidemics of HEV infection. Clinical. The course is identical to that of hepatitis A. There are no chronic courses or healthy virus carriers. Women who become infected with HEV in the last trimester of pregnancy die in about 25% of cases. This condition refers to inflammatory liver disorders that persist for 6 months or longer without improvement. Aggressive chronic hepatitis manifests in a disease progression with not only nonspecific symptoms but also signs of liver cirrhosis, e.g., esophageal varices. Definition. Fatty liver refers to an increase of fat deposits in the liver cells. If more than 50% of the cells are affected, we talk about a fatty liver. If less than 50% of cells are affected, we call the condition fatty degeneration of the liver. Causes Clinical. In most cases, hepatomegaly manifests with no complaints. The symptoms depend on the cause. Definition. Toxic effect on the liver as a result of excess alcohol or alcohol abuse. Clinical Definition. Irreversible change in normal liver tissue with fibrosis and destruction of the physiologic microscopic lobe structure. Causes Clinical. Liver insufficiency with: Estrogen dominance with: Portal hypertension with: General symptoms: Definition. Increased pressure in the portal vein system of more than 15 mmHg. Causes. The blood flow in the portal vein system is blocked. This obstruction in blood flow can be prehepatic, intrahepatic, or posthepatic. Possible causes include: Clinical. Development of portacaval bypass circuits with: Definition. This is the most common malignant liver tumor. It develops from degenerated liver cells. Make sure that you distinguish it from liver metastases of extrahepatic tumors. Causes Clinical

5 The Liver
Anatomy
General Facts
 left and right lobe
left and right lobe
 caudate lobe
caudate lobe
 quadrate lobe
quadrate lobe
Location
Cranial Boundary
 anterior: fifth intercostal space (ICS) on the right to the sixth ICS on the left
anterior: fifth intercostal space (ICS) on the right to the sixth ICS on the left
 on the left side; extending roughly to a vertical line through the body via the center of the left inguinal ligament
on the left side; extending roughly to a vertical line through the body via the center of the left inguinal ligament
 posterior: T8–T9
posterior: T8–T9
Caudal Boundary
 anterior: lower costal arch ascending from right to left past the center line
anterior: lower costal arch ascending from right to left past the center line
 posterior: T11-T12
posterior: T11-T12
Topographic Relationships
 dorsolateral and anterior on the right: abdominal wall and ribs 8–11
dorsolateral and anterior on the right: abdominal wall and ribs 8–11
 diaphragm
diaphragm
 gallbladder
gallbladder
 hepatic/cystic/common bile duct
hepatic/cystic/common bile duct
 inferior vena cava
inferior vena cava
 portal vein
portal vein
 proper hepatic artery
proper hepatic artery
 stomach
stomach
 right adrenal gland
right adrenal gland
 right kidney
right kidney
 duodenum: superior and descending part
duodenum: superior and descending part
 right colic flexure
right colic flexure
 indirect contact to pleura, lung, pericardium, and heart
indirect contact to pleura, lung, pericardium, and heart
Attachments/Suspensions
 pressure in the abdominal cavity
pressure in the abdominal cavity
 turgor
turgor
 coronary ligament
coronary ligament
 left and right triangular ligament
left and right triangular ligament
 falciform ligament
falciform ligament
 round ligament of the liver
round ligament of the liver
 lesser omentum (hepatoduodenal and hepatogastric ligaments)
lesser omentum (hepatoduodenal and hepatogastric ligaments)
 hepatorenal ligament
hepatorenal ligament
 inferior vena cava
inferior vena cava
Circulation
Arterial
Venous
 portal vein (collects blood from the spleen, distal esophagus, stomach, small intestine, colon, upper rectum, pancreas, and gallbladder)
portal vein (collects blood from the spleen, distal esophagus, stomach, small intestine, colon, upper rectum, pancreas, and gallbladder)
 inferior vena cava
inferior vena cava
Lymph Drainage
Innervation
 sympathetic nervous system from T7 to T10 via the greater and lesser splanchnic nerve
sympathetic nervous system from T7 to T10 via the greater and lesser splanchnic nerve
 switchover in the celiac plexus
switchover in the celiac plexus
 vagus nerve
vagus nerve
 The liver capsule is innervated via the phrenic nerve (C3–C5).
The liver capsule is innervated via the phrenic nerve (C3–C5).
Organ Clock
Organ–Tooth Interrelationship
Movement Physiology according to Barral
Mobility
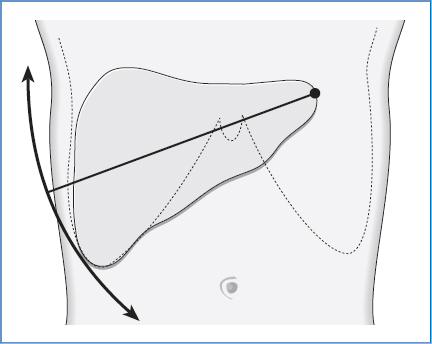
Frontal Plane
Sagittal Plane
Transverse Plane
Motility
Physiology
Metabolic Functions of the Liver
 lipolysis (metabolism of fatty acids up to coenzyme A)
lipolysis (metabolism of fatty acids up to coenzyme A)
 production of ketone bodies from fat, e.g., in hunger periods or in badly adjusted diabetes mellitus with bad breath smelling of acetone
production of ketone bodies from fat, e.g., in hunger periods or in badly adjusted diabetes mellitus with bad breath smelling of acetone
 lipogenesis (production of triglycerides)
lipogenesis (production of triglycerides)
 glycogenesis and glycogenolysis
glycogenesis and glycogenolysis
 gluconeogenesis (synthesis of glucose from lactate or amino acids)
gluconeogenesis (synthesis of glucose from lactate or amino acids)
 formation of proteins from amino acids (e.g., albumin, globulin, fibrinogen, prothrombin, vitamin K-dependent coagulation factors)
formation of proteins from amino acids (e.g., albumin, globulin, fibrinogen, prothrombin, vitamin K-dependent coagulation factors)
 breakdown of proteins, e.g., estrogen
breakdown of proteins, e.g., estrogen
 production of urea from brain—toxic ammonia, the product of protein breakdown
production of urea from brain—toxic ammonia, the product of protein breakdown
 breakdown and excretion of exogenous toxins, e.g., medications
breakdown and excretion of exogenous toxins, e.g., medications
 storage organ, e.g., for glycogen, or vitamin A or B12
storage organ, e.g., for glycogen, or vitamin A or B12
 production and excretion of bile
production and excretion of bile
 synthesis and processing of cholesterol
synthesis and processing of cholesterol
 location of blood production up to the sixth fetal month
location of blood production up to the sixth fetal month
Pathologies
Symptoms that Require Medical Clarification
Icterus
Acute Hepatitis
Hepatitis A
Hepatitis B
Hepatitis D
Hepatitis C
Hepatitis E
Chronic Hepatitis
Definition
Causes
 HBV infection
HBV infection
 HCV infection
HCV infection
 HDV infection
HDV infection
 autoimmune hepatitis
autoimmune hepatitis
 toxins (alcohol, medications)
toxins (alcohol, medications)
Fatty Liver
 alcohol abuse
alcohol abuse
 adiposity
adiposity
 diabetes mellitus
diabetes mellitus
 pregnancy
pregnancy
 toxins, e.g., poisonous mushrooms
toxins, e.g., poisonous mushrooms
Liver Damage from Alcohol
 fatty liver
fatty liver
 steatosis hepatitis or acute alcohol hepatitis with signs of liver insufficiency to the point of liver failure with:
steatosis hepatitis or acute alcohol hepatitis with signs of liver insufficiency to the point of liver failure with:
 alcoholic liver cirrhosis
alcoholic liver cirrhosis
Cirrhosis of the Liver
 alcohol
alcohol
 HBV, HCV, HDV
HBV, HCV, HDV
 medications
medications
 cystic fibrosis
cystic fibrosis
 chronic right cardiac insufficiency
chronic right cardiac insufficiency
 structural tissue change: enlargement of the liver with hardening and bumpy surface (the liver shrinks terminally) and hypoperfusion of the liver
structural tissue change: enlargement of the liver with hardening and bumpy surface (the liver shrinks terminally) and hypoperfusion of the liver
 icterus
icterus
 hepatic encephalopathy
hepatic encephalopathy
 ascites and ankle edema (albumin deficiency)
ascites and ankle edema (albumin deficiency)
 anemia
anemia
 a bleeding tendency
a bleeding tendency
 spider angioma
spider angioma
 men with loss of chest hair, abdominal baldness, testicular atrophy
men with loss of chest hair, abdominal baldness, testicular atrophy
 palmar erythema
palmar erythema
 gynecomastia
gynecomastia
 hypersplenism with bone marrow changes and pancytopenia and hemorrhagic diathesis
hypersplenism with bone marrow changes and pancytopenia and hemorrhagic diathesis
 splenomegaly
splenomegaly
 esophageal varices
esophageal varices
 caput medusae
caput medusae
 external hemorrhoids
external hemorrhoids
 ascites
ascites
 fatigue
fatigue
 reduced productivity
reduced productivity
 nonspecific upper abdominal complaints
nonspecific upper abdominal complaints
 cachexia
cachexia
Portal Hypertension
 prehepatic: portal vein thrombosis
prehepatic: portal vein thrombosis
 intrahepatic: cirrhosis of the liver
intrahepatic: cirrhosis of the liver
 posthepatic: right cardiac insufficiency
posthepatic: right cardiac insufficiency
 esophageal varices
esophageal varices
 caput medusae
caput medusae
 external hemorrhoids
external hemorrhoids
 ascites (transudation of plasma fluid, e.g., via the mesenteric veins)
ascites (transudation of plasma fluid, e.g., via the mesenteric veins)
 splenomegaly
splenomegaly
Primary Hepatocellular Carcinoma
 alcohol abuse
alcohol abuse
 chronic HBV and HCV
chronic HBV and HCV
 aflatoxin poisoning (ergot alkaloids)
aflatoxin poisoning (ergot alkaloids)
 symptoms of a decompensated liver cirrhosis
symptoms of a decompensated liver cirrhosis
 cachexia
cachexia
Osteopathic Practice
Cardinal Symptoms
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






