Chapter 11. The knee
SUMMARY
This chapter presents the anatomy of the knee relating to commonly encountered lesions. The commentary which follows explores the relevant points of history, aiding diagnosis, and the suggested method of objective examination adheres to the principles of selective tension. The lesions, their treatment and management are then discussed.
ANATOMY
Inert structures
The lower end of the femur consists of two large femoral condyles which articulate with, and transfer weight to, corresponding surfaces on the tibial condyles at the tibio-femoral joint. The two femoral condyles are separated posteriorly and inferiorly by the intercondylar notch or fossa. The anterior aspect of the femur bears an articular surface for the patella to form the patellofemoral joint.
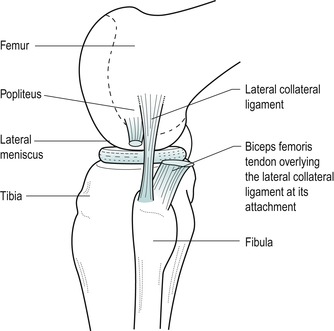
The lateral femoral epicondyle gives attachment to the proximal end of the lateral (fibular) collateral ligament. Below this lies a smooth groove which contains the tendon of popliteus in full flexion of the knee. The medial femoral condyle displays a prominent adductor tubercle on the medial supracondylar line and just below this the medial epicondyle gives origin to the medial (tibial)collateral ligament. Posteriorly, the heads of gastrocnemius originate from the femoral condyles.
The tibia has an expanded upper end which overhangs the shaft posteriorly. The upper weight-bearing surface bears two shallow tibial condyles divided by the intercondylar area. Below the posterolateral tibial condyle lies an oval facet for articulation with the head of the fibula at the superior (proximal) tibiofibular joint. Anteriorly lies the prominent tibial tuberosity which gives insertion to the infrapatellar tendon (ligamentum patellae). Gerdy’s tubercle lies anterolaterally and marks the insertion of the iliotibial tract (Kapandji 1987, Burks 1990).
The upper end of the fibula is expanded to form the head, which articulates with the tibia on its superomedial side, at the superior tibiofibular joint. The apex of the head of the fibula gives attachment to the lateral collateral ligament and the biceps femoris tendon. The common peroneal nerve winds round the neck of the fibula.
The patella, the largest sesamoid bone in the body, lies within the quadriceps tendon and articulates with the lower end of the femur at the patellofemoral joint. It is a flat triangular-shaped bone with its base uppermost and apex pointing inferiorly (see Fig. 11.3). It has anterior and posterior surfaces and upper, medial and lateral borders. Its anterior surface shows vertical ridges produced by fibres of the quadriceps which pass over it. This surface is separated from the skin by a synovial-lined potential space, the subcutaneous prepatellar bursa. It contains minimal fluid and is only obvious when inflamed (Pope & Winston-Salem 1996).
Rectus femoris and vastus intermedius insert into the base of the patella, and the roughened posterior aspect of the apex gives attachment to the proximal end of the infrapatellar tendon (ligamentum patellae). A subcutaneous superficial infrapatellar bursa lies between the infrapatellar tendon and the skin; a deep infrapatellar bursa lies deep to the distal portion of the infrapatellar tendon and the underlying tibia and has no communication with the knee joint (LaPrade 1998). It is located by palpation on the lateral side of the infrapatellar tendon in extension, just proximal to the tibial tubercle; a point of access for injection (LaPrade 1998). Several fat pads are interposed between the knee joint capsule and synovial lining. The infrapatellar fat pad of Hoffa lies between the infrapatellar tendon and the knee joint and may be subjected to trauma or impingement (Jacobson et al 1997).
The vastus medialis and lateralis muscles send tendinous insertions to the medial and lateral borders of the patella in the form of quadriceps expansions (or the patella retinacula). The lateral expansion receives a distinct extension from the iliotibial tract and the quadriceps expansions together are responsible for transverse stability of the patella. The medial quadriceps expansion blends with the anterior fibres of the medial collateral ligament (Fig. 11.3).
The posterior articulating surface of the patella is covered with thick articular cartilage which is divided by a vertical ridge into medial and lateral articular facets for articulation with the femur, with an ‘odd’ facet on the medial side.
The knee joint consists of the tibiofemoral, patellofemoral and superior tibiofibular joints. The former two articulations exist within the same capsule but each has a different function:
• Tibiofemoral joint: involved in weight-bearing activities
• Patellofemoral joint: the joint of the extensor mechanism of the knee
The tibiofemoral joint is a synovial hinge joint between the convex condyles of the femur and the slightly concave articular surfaces of the tibia. Mobility is not normally compatible with stability in a joint, but the incongruent joint surfaces of the knee make it a mobile joint, while the shape of the articular surfaces and the interaction of muscles, tendons and strong ligaments all contribute to stability.
Two semilunar cartilages, the menisci, deepen the tibial articulating surface and contribute to the congruency of the joint. The menisci facilitate load transmission, shock absorption, lubrication and stability (Bessette 1992, Bikkina et al 2005). The peripheral rim of each meniscus is attached to deep fibres of the capsule which secure it to the edge of the tibial condyles. These deep capsular fibres are known as the coronary ligaments ( corona, Latin=crown) or meniscotibial ligaments (Fig. 11.1). They are difficult to separate from the adjacent capsule and collateral ligament and attach several millimetres below the articular cartilage (Bikkina et al 2005). They are strong, but lax enough to allow axial rotation to occur at the meniscotibial surface. The lateral coronary ligaments are longer than the medial to allow for the greater excursion of the lateral meniscus (Burks 1990).
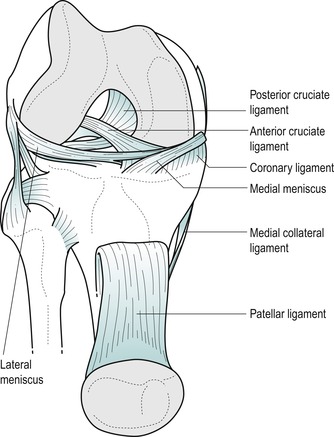 |
| Figure 11.1 Anterior view of the knee with patella reflected showing Coronary (meniscotibial) ligaments. |
The menisci are composed of collagen fibres. The superficial collagen fibres are oriented radially and the deep fibres are circumferential (Bessette 1992). The orientation of the collagen fibres facilitates dispersion of compressive loads by the circumferential fibres and resistance to longitudinal stresses by the radial fibres; the fibre orientation at the surface of the meniscus is a random meshwork thought to be important for distributing shear stress (Greis et al 2002). Injury usually involves rotational strains and may result in longitudinal or transverse splitting of the fibrocartilage, or separation of the thinner inner part of the meniscus from the thicker outer portion, forming a ‘bucket handle’ lesion.
The medial meniscus is the larger of the two and is almost semicircular in shape. Its periphery has a definite attachment to the deep part of the medial collateral ligament, which forms part of the fibrous capsule of the knee joint. The lateral meniscus is almost circular but it is separated from the capsule of the knee joint at its periphery by the tendon of popliteus, to which it is attached. Posteriorly, the lateral meniscus contributes a ligamentous slip to the posterior cruciate ligament, known as the posterior meniscofemoral ligament.
The fibrous capsule of the knee joint is strongly supplemented by expansions from the tendons that cross it, plus ligamentous thickenings and independent ligamentous reinforcements. The medial collateral ligament, in particular, provides a strong integral reinforcement of the capsule, attaching also to the medial meniscus. The anterior capsule is reinforced by the quadriceps expansions and an extension from the iliotibial band. Independent ligaments such as the lateral collateral ligament and cruciates also have a strong stabilizing effect on the joint.
The cylindrical fibrous capsule is invaginated posteriorly and lined with synovial membrane. The synovium is reflected upwards anteriorly under the quadriceps, approximately three fingers’ breadth, to form the suprapatellar bursa. The articularis genu muscle connects vastus intermedius and the upper part of the suprapatellar bursa, maintaining the bursal cavity during extension of the knee. Plicae (folds of synovium that protrude inwards) exist in the knee joint and may be responsible for symptoms. Three are usually recognized: the superior plica, thought to be an embryological remnant of the division between the suprapatellar bursa and the joint; the inferior plica, located in the intercondylar notch anterior to the anterior cruciate ligament; and a medial plica, a vertical fold, varying from a small ridge to a cord-like structure adjacent to the medial border of the patella (Boles & Martin 2001).
As well as the bursae associated with the patella and patellar tendon as described above, numerous bursae are associated with the knee, facilitating the function of the tendons which are running more or less parallel to the bones, to exert a lengthwise pull across the joint (Palastanga et al 2006). Posteriorly, a bursa sits under each head of origin of gastrocnemius. Laterally, bursae lie either side of the lateral collateral ligament, cushioning it from biceps femoris and popliteus, as well as between popliteus and the lateral femoral condyle. Medially, the pes anserine bursa sits between the distal medial collateral ligament and the tendons of sartorius, gracilis and semitendinosus, known collectively as the pes anserinus. The semimembranosus bursa lies between the tendon of semimembranosus and the medial tibial condyle of the tibia and a variable number of small bursae lie deep to the medial collateral ligament.
The ligaments of the knee provide a dynamic guide during movement and act as a passive restraint to abnormal translations (Barrack & Skinner 1990). Each ligament is oriented in a direction to produce stability, and force is dissipated at the insertion by a gradual transition from ligament, to fibrocartilage, to bone (Woo et al 1990).
The medial collateral ligament is a strong, broad, flat band lying posteriorly over the medial joint line. The posteromedial position of the medial collateral ligament means that its anterior border may be palpated running perpendicular to and approximately halfway along the medial joint line, the ligament itself lying roughly two and a half fingers’ width behind this point. Passing from the medial femoral epicondyle just distal to the adductor tubercle, it descends vertically across the joint line and runs forwards to its attachment on the medial condyle and shaft of the upper tibia approximately 5 cm below the joint line, posterior to the pes anserinus insertion. As the ligament crosses over the knee joint its anterior fibres blend with fibres of the medial patellar retinaculum (El-Dieb et al 2002). It is the primary static stabilizer of the medial aspect of the knee joint and is assisted by the quadriceps expansions and the tendons of sartorius, gracilis and semitendinosus, which cross over its lower part, and from which it is separated by the pes anserine bursa.
The medial collateral ligament is composed of superficial and deep layers. The superficial part of the ligament, often referred to as the tibial collateral ligament, consists of fibres which pass directly from the femur to the tibia (Staron et al 1994, Schweitzer et al 1995). These fibres are relatively strong and provide 80% of the resistance to valgus force (Schenck & Heckman 1993). Under the superficial medial collateral ligament the capsule is thickened to form the deep medial collateral ligament which is firmly anchored to the medial meniscus (Pope & Winston-Salem 1996). This part of the ligament is relatively weaker. The capsule is further thickened by superior fibres, the meniscofemoral ligaments, which attach the meniscus to the femur, and inferior fibres, the meniscotibial ligaments, more commonly known as the coronary ligaments, which attach the meniscus to the tibia (Burks 1990, Staron et al 1994).
The primary stabilizing role of the medial collateral ligament is to support the medial aspect of the knee joint preventing excessive valgus movement. Its secondary stabilizing role is in preventing lateral rotation of the tibia, anterior translation of the tibia on the femur and hyperextension of the knee. Most of the ligament is taut in full extension preventing hyperextension, but it also remains taut throughout flexion (Pope & Winston-Salem 1996). Mechanisms of injury commonly include a rotation stress to the knee and the ligament is often injured together with the anterior cruciate ligament and medial meniscus. Valgus injuries occur through direct impact to the lateral aspect of the knee.
The lateral collateral ligament in isolation is a shorter, cord-like ligament separated from the capsule of the knee joint by the tendon of popliteus. It is approximately 5 cm long and roughly the size of half a pencil (Evans 1986, Palastanga et al 2006). It runs from the lateral femoral epicondyle to the head of the fibula where it blends with the insertion of biceps femoris to form a conjoined tendon which is an important lateral stabilizer.
However, the lateral collateral ligament may be more complex than that. Anatomically it is closely related to the underlying iliotibial band which is similar in width and direction to the medial collateral ligament and may indeed provide dynamic stability to the lateral aspect of the knee joint. Posteriorly the lateral collateral ligament has a relationship with the arcuate popliteal ligament and the popliteus tendon (Pope & Winston-Salem 1996). Its primary stabilizing role is to restrain varus movement, supporting the lateral aspect of the knee (Burks 1990), with a secondary stabilizing role in controlling posterior drawer and lateral rotation of the tibia. Injuries to the lateral collateral ligament complex are not as common as those to the medial aspect, but, if they do occur, they are more disabling and difficult to diagnose. Mechanisms of injury include a varus force applied to the knee in flexion and/or medial rotation, an unusual position for the knee accounting for the relative rarity of this injury (El-Dieb et al 2002).
The cruciate ligaments are strong intracapsular, but extrasynovial, ligaments said to be about as thick as a pencil (Evans 1986, Bowditch 2001). They are called cruciate ( crux, Latin=cross) because of the way they cross in the intercondylar fossa and are named anterior or posterior by their tibial attachments (see Figure 11.1 and Figure 11.2). Their primary stabilizing role is to resist anterior and posterior translation of the tibia under the femur. Their secondary stabilizing function is to act as internal collateral ligaments controlling varus, valgus and rotation (Schenck & Heckman 1993).
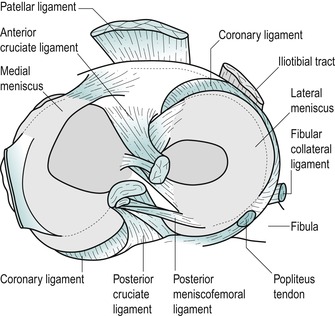 |
| Figure 11.2 Cruciate ligament attachments on the tibial plateau. |
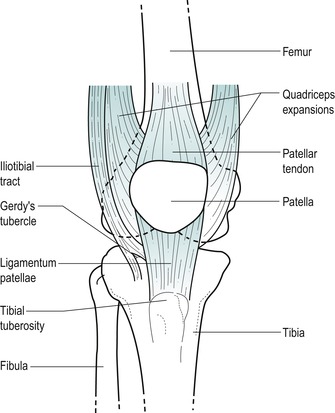 |
| Figure 11.3 Anterior aspect of the knee. |
The anterior cruciate ligament passes from the anterior tibial intercondylar area upwards, posteriorly and laterally, twisting as it goes, to attach to the posteromedial aspect of the lateral femoral condyle. Anatomically it can be divided into two parts: an anteromedial band which is taut in flexion and a posterolateral band which is taut in extension. Functionally, the ligament has a stabilizing effect throughout the range of movement (Katz & Fingeroth 1986, Perko et al 1992). Its primary stabilizing role resists anterior translation and medial rotation of the tibia on the femur. A secondary stabilizing role relates it to the collateral ligaments in resisting valgus, varus and hyperextension stresses (Evans 1986). A study by Butler et al (1980) showed the anterior cruciate ligament to provide 86% of the total resisting force to anterior translation, with other ligaments and capsular structures making up the remaining secondary restraint (Katz & Fingeroth 1986). The most common mechanism of injury to the anterior cruciate ligament is lateral rotation combined with a valgus force applied to the fixed tibia. Less common mechanisms may include hyperextension, medial rotation in full extension or anterior translation produced by direct injury to the calf. Most tears occur within the ligament itself, with 20% involving either bony attachment (El-Dieb et al 2002). Complete ruptures of the anterior cruciate ligament most commonly result in disruption of all fibres and synovial coverings leading to a haemarth-rosis. With partial tears the synovial envelope may not be disrupted, leading to a contained haematoma without a haemarthrosis (Bowditch 2001).
The posterior cruciate ligament passes upwards, anteriorly and medially from the posterior intercondylar area, to attach to the anterolateral aspect of the medial femoral condyle. The ligament is said to be twice as strong and less oblique than the anterior cruciate ligament and its close relationship to the centre of rotation of the knee joint makes it a principal stabilizer (Palastanga et al 2006). As well as controlling posterior translation of the tibia on the femur, it seems to have a role in producing and restraining rotation of the tibia, since posterior translation occurs with concomitant lateral rotation of the tibia. Injury to the posterior cruciate ligament is not as common as to its anterior partner. Forced posterior translation of the tibia on the flexed knee, the typical ‘dashboard’ injury, is the most common mechanism of injury, but it may also be injured in forced hyperextension (El-Dieb et al 2002).
The main function of the knee joint is weight-bearing; therefore symptoms are usually produced on weight-bearing activities. During the gait cycle, the forces across the tibiofemoral joint amount to two to five times body weight according to position and activity. However, the forces may increase to 24 times body weight during activities such as jumping (Palastanga et al 2006).
The range of movement at the knee joint is greatest in the sagittal plane with an active range from 0° extension to 140° of flexion. Approximately 5–10° of passive extension is usually available and up to 160° of passive flexion, which is halted when the calf and hamstring muscles approximate and the heel reaches the buttock. During flexion and extension, the menisci stay with the tibia so that these movements occur as the femoral condyles roll and slide over the menisci.
Active and passive axial rotation occur with the knee joint in flexion and the range available is greatest at 90° of flexion. Active lateral rotation amounts to approximately 45° and medial rotation of 35°, with a little more movement in each direction available passively. During axial rotation, the menisci now stay with the femur and rotation occurs as the femoral condyles and menisci roll and glide over the tibial condyles. The coronary ligaments are lax enough to permit this movement.
A few degrees of automatic, involuntary rotation occurs to achieve the locked or unlocked positions of the knee. During the last 20° or so of knee extension, lateral rotation of the tibia on the femur occurs to produce the terminal ‘screw-home’ or ‘locking’ phase of the knee. This achieves the close packed position of the knee joint, where it is most stable, and rotation and accessory movements are impossible to perform on the normal extended knee. The knee is unlocked by the action of popliteus medially rotating the tibia on the femur.
The locking mechanism of the knee occurs because the medial femoral condyle is slightly longer than the lateral and the shape of the tibial condyles allows the lateral femoral condyle to glide more freely and over a greater distance than the medial. The ligaments around the knee contribute to stability in extension when most fibres are under tension.
The patellofemoral joint is the joint between the posterior aspect of the patella and the anterior surface of the femur. It is the joint of the extensor mechanism of the knee and therefore gives rise to symptoms on antigravity activities. The patella performs two important biomechanical functions at the knee (Nordin & Frankel 2001):
• It produces anterior displacement of the quadriceps tendon throughout movement, assisting knee extension by increasing the lever arm of the quadriceps muscle force.
• It increases the area of contact between the patellar tendon and the femur, distributing compressive forces over a wider area.
The articular cartilage on the back of the patella is said to be the thickest in the body, at 5–6 mm thick (Evans 1986). It is divided into areas for articulation with the medial and lateral femoral condyles in varying degrees of flexion and extension. The patella glides caudally approximately 7 cm and rotates as the knee moves from full extension to full flexion. The patella eventually sinks into the intercondylar groove in full knee flexion (Nordin & Frankel 2001).
Patellofemoral symptoms may arise from instability, maltracking, malalignment, biomechanical causes, subluxation and dislocation, which may lead to eventual chondromalacia patellae and osteoarthrosis of the joint. There is a tendency for the patella to slip laterally, particularly as the knee moves towards full extension, and this is counteracted by:
• The high lateral border of the patellar groove on the femur
• The active muscle pull of the oblique fibres of vastus medialis
• The medial quadriceps expansion.
The superior tibiofibular joint is a synovial plane joint between the lateral tibial condyle and the head of the fibula; it communicates with the knee joint in 10% of adults (Bozkurt et al 2003). The joint capsule is reinforced by anterior and posterior tibiofibular ligaments. Small accessory movements are possible at this joint which is mechanically linked to the inferior tibiofibular joint and dissipates torsional stress applied to the ankle. It is therefore influenced by movements at the ankle joint (Bozkurt et al 2003).
Contractile structures
The contractile structures at the knee consist of muscles which originate from the hip region and insert at the knee, or originate at the knee and insert below the ankle. The muscles will be described in relationship to the knee and the reader is referred to the chapters on the hip and ankle for further discussion of the muscle groups.
Quadriceps femoris (femoral nerve L2–L4) is composed of four muscles: rectus femoris, vastus lateralis, vastus medialis and vastus intermedius, uniting around the patella to form the infrapatellar tendon, which passes from the apex of the patella to insert into the tibial tuberosity.
Rectus femoris originates above the hip joint and inserts into the base of the patella (upper border) with fibres continued over and on each side of the patella contributing to the infrapatellar tendon.
Vastus lateralis passes down from the upper anterolateral femur to form a broad tendon which eventually tapers as it inserts into the lateral border of the patella as the lateral quadriceps expansion. Vastus lateralis contributes to the main quadriceps tendon, passing over the patella, as well as blending with fibres of the iliotibial tract to form a lateral extension and to support the anterolateral joint capsule.
Vastus medialis passes from the upper anteromedial femur downwards, to join the common quadriceps tendon and the medial border of the patella as the medial quadriceps expansion. The medial quadriceps expansion is a strong sheet of fibres on the anteromedial aspect of the knee with fibres continuing to run inferiorly and posteriorly to insert onto the tibia beside the fibres of the medial collateral ligament (Greenhill 1967). The lower fibres of the muscle, which continue to form the medial expansion, run more horizontally and have their origin from adductor magnus, with which they share a nerve supply. These fibres are commonly known as the vastus medialis obliquus (VMO). The VMO traditionally has a role in the ‘screwing home’ of the tibia in the final locking stage of knee extension (Greenhill 1967).
Vastus intermedius is the deepest part of the quadriceps and inserts with rectus femoris into the base of the patella as the suprapatellar tendon.
Quadriceps femoris is the main extensor muscle of the knee joint. Vastus medialis is believed to be particularly active during the later stages of knee extension, when it exerts a stabilizing force on the patella to prevent it slipping laterally. Although quiet in standing, the quadriceps femoris muscle contracts strongly in such activities as climbing.
The hamstrings (sciatic nerve L5, S1–S2), comprising biceps femoris, semimembranosus and semitendinosus, are responsible for flexion of the knee and medial and lateral rotation of the knee when flexed in the mid-position.
Biceps femoris inserts into the head of the fibula, splitting around the lateral collateral ligament as it does so, with which it forms a conjoined tendon. Semimembranosus has its main attachment into the posterior aspect of the medial tibial condyle, but sends slips on to blend with other structures to support the posteromedial capsule. Semitendinosus curves around the medial tibial condyle to the upper surface of the medial tibia together with sartorius and gracilis to form the pes anserine tendon complex. These tendons blend with the medial capsule, lending it some support. The pes anserine tendon complex is responsible for flexion of the knee and medial rotation of the tibia on the femur (Valley & Shermer 2000).
The iliotibial tract inserts into Gerdy’s tubercle on the anterolateral aspect of the upper tibia and blends with the lateral capsule and the lateral quadriceps expansion; functionally it is related to the lateral collateral ligament. Tensor fascia lata, acting with gluteus maximus, tightens the tract and assists extension of the knee.
Popliteus (tibial nerve L4–L5, S1) originates within the capsule of the knee joint as a tendon arising from the groove on the lateral aspect of the lateral femoral condyle. It separates the lateral collateral ligament from the fibrous capsule of the knee joint and, as it passes downwards, backwards and medially, it sends tendinous fibres to the posterior horn of the lateral meniscus. It forms a fleshy, triangular muscle belly and attaches to the posterior aspect of the tibia above the soleal line. Popliteus is the primary medial rotator of the knee, medially rotating the tibia on the femur and unlocking the knee joint from the close packed position. Some consider that, through its attachment to the lateral meniscus, it pulls the meniscus backwards during rotatory movements, possibly preventing it from being trapped (Safran & Fu 1995). Its complex attachment to the lateral meniscus, arcuate ligament, posterior capsule and lateral femoral condyle provides an appreciable role in dynamic stability, particularly in preventing forwards displacement of the femur on the tibia (Burks 1990, Safran & Fu 1995, El-Dieb et al 2002).
Gastrocnemius (tibial nerve S1–S2) arises by two heads from the posterior aspect of the medial and lateral femoral condyles and together with soleus and plantaris forms the triceps surae. As well as its action at the ankle, gastrocnemius is a strong flexor at the knee, but is unable to act strongly at both joints simultaneously.
A GUIDE TO SURFACE MARKING AND PALPATION
Anterior aspect (Fig. 11.3)
Locate the patella at the front of the knee and identify its base (upper border), apex (lower border), medial and lateral borders. With the knee extended and relaxed you should be able to shift the patella from side to side to palpate the insertion of the quadriceps expansions under the edge of each border. Tilt the base and apex to locate the suprapatellar and infrapatellar tendons respectively.
Follow the infrapatellar tendon down to its insertion onto the tibial tuberosity, which lies approximately 5 cm below the apex of the patella in the flexed knee.
Palpate and mark in the knee joint line with the knee in flexion. The anterior articular surface of each femoral condyle and the anterior articular margins of the tibia should be palpable at either side of the patella. Both can be followed round onto the medial and lateral aspects, but it is not possible to palpate the joint line posteriorly since it is covered by many musculotendinous structures.
With the knee joint flexed, the apex of the patella marks the approximate position of the joint line. In extension, the apex of the patella lies approximately one finger’s breadth above the joint line. This information may provide a useful guide if the joint is very swollen, making it difficult to palpate the joint line.
The quadriceps muscle forms the major anterior muscle bulk. On static contraction of this muscle, locate rectus femoris, which forms the central part of the muscle bulk. Vastus lateralis forms an obvious lateral muscle bulk, while vastus medialis terminates in oblique fibres which form part of the medial quadriceps expansion.
Lateral aspect (Fig. 11.4)
On the anterolateral surface of the tibia, approximately two-thirds of the way forward from the head of the fibula to the tibial tuberosity, palpate for Gerdy’s tubercle, which gives attachment to the iliotibial tract. The tract should be obvious as the quadriceps contracts.
 |
| Figure 11.4 Lateral aspect of the knee. |
Palpate the head of the fibula just below the posterior part of the lateral condyle of the tibia where it forms the proximal tibiofibular joint. The common peroneal nerve can be rolled over the neck of the fibula.
Place the leg into the FABER position of flexion, abduction and external (lateral) rotation, and palpate the lateral aspect of the knee joint line. You should be able to roll the cord-like lateral collateral ligament under your fingers.
Medial aspect (Fig. 11.5)
Palpate the medial condyle of the femur and locate the prominent adductor tubercle on the upper part of the condyle. Deep palpation is necessary and the tubercle will feel tender to palpation.
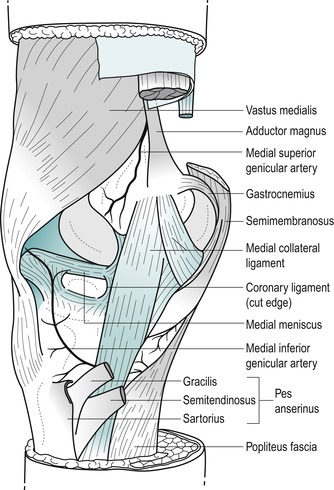 |
| Figure 11.5 Medial aspect of the knee. |
Move directly distally from the adductor tubercle until you are over the joint line and see if you can identify, by palpation, the anterior edge of the medial collateral ligament. This ligament is approximately 8–10 cm long (Palastanga et al 2006) and two and a half fingers wide as it broadens to cross the joint line. Its anterior border may be palpated in most people and is usually in line with or just behind the central axis of the joint.
Visualize the position of the sartorius, gracilis and semitendinosus tendons (the pes anserine complex) as they cross the lower part of the medial collateral ligament to their insertion on the upper part of the medial tibia.
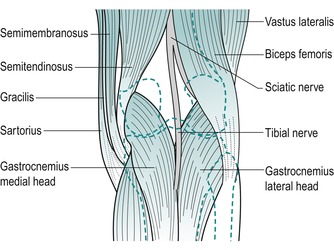
Posterior aspect (Fig. 11.6)
Resist knee flexion and palpate the hamstrings, which form the muscle bulk of the posterior thigh. The point at which the medial and lateral hamstrings separate can be identified, with biceps femoris forming the lateral wall of the popliteal fossa and semitendinosus lying on semimembranosus forming the medial wall.
 |
| Figure 11.6 Posterior aspect of the knee. |
Biceps femoris can be followed down to its insertion onto the head of the fibula.
On the medial side of the popliteal fossa, semitendinosus can be felt as an obvious tendon. Medial to it is gracilis, made more prominent by adding resisted medial rotation. Deeper to this is semimembranosus, remaining more muscular as it blends into its aponeurotic attachment.
Posteriorly, locate the two heads of gastrocnemius as they originate above the knee joint from the medial and lateral femoral condyles.
COMMENTARY ON THE EXAMINATION
Observation
A general observation is made of the patient’s face and overall posture, but as the knee is a weight-bearing joint, particular attention is paid to the gait pattern. Note if an antalgic posture or gait has been adopted; a limp will be evident during gait if the patient has an abnormal stride length or is not weight-bearing evenly. Toeing in or out, together with abnormalities of foot posture, should also be noted.
History (subjective examination)
A detailed history is required at the knee since it gives important diagnostic clues, including typical injury patterns, which may be confirmed by clinical examination. It also assists in the identification of lesions which may be better suited for specialist referral.
The age, occupation, sports, hobbies and lifestyle of the patient are particularly relevant.
Some conditions affect certain age groups. Knee pain in children is commonly referred from the hip and it is necessary to carry out a thorough examination of both joints. Meniscal lesions are unusual in children and increase in incidence from adolescence onwards. A gradual onset of knee pain in adolescents may be related to patellofemoral joint syndromes or Osgood–Schlatter’s disease which presents as a localized pain felt over the tibial tuberosity due to traction apophysitis of the tibial tubercle.
The young adult, particularly male, may present with traumatic meniscal lesions associated with rotational injury during sporting activities (Greis et al 2002). Females tend to present with instability, subluxation or episodes of dislocation of the patella.
Rheumatoid arthritis may affect the knee and onset usually occurs between the ages of 30 and 40. Degenerative osteoarthrosis affects the older age group, but may occur earlier if predisposed by previous injury or through overuse in sporting activity. It is important to remember that osteoarthrosis can affect both the patellofemoral and tibiofemoral joints. Degenerative meniscal lesions occur more commonly in males in the fourth to sixth decades and can develop in association with degenerative joint disease (Greis et al 2002).
The lifestyle of the patient will reflect whether occupational or recreational activities are a contributing factor to their condition. Sport in particular may be responsible for traumatic incidents to the relatively unstable knee, especially in positions of flexion. Progressive microtrauma may be the result of incorrect training or overtraining, muscle imbalances or poor joint biomechanics.
The site of the pain indicates whether it is local or referred. Superficial structures tend to give local pain and point tenderness; therefore lesions of the medial collateral ligament, coronary ligaments or the tendinous insertions of the muscles around the knee give reasonably accurate localization of pain. Acutely inflamed lesions or deep lesions, such as of the tibiofemoral joint, menisci or cruciate ligaments, produce a vague, more widely felt, deep pain, with the patient unable to localize the lesion accurately.
The spread of pain generally indicates the severity of the lesion. While referred pain is expected distally to the site of the lesion, the knee as a central limb joint may also produce some proximal pain in the thigh. Pain referred from the hip or lumbar spine can be felt at the knee and both may need to be eliminated as a cause of pain.
Anterior knee pain is a description of the symptoms felt by the patient, although the term is often misused as a diagnosis. It usually indicates patellofemoral joint involvement, but must not be considered to be due to it exclusively. Chondromalacia patellae is a softening of articular cartilage that can be explored with magnetic resonance imaging (MRI) to establish the nature of the lesion. A bipartite patella is a normal asymptomatic variant which is often bilateral; it can occasionally become painful due to overuse or acute injury. The most common site for the lesion is the superolateral corner at the insertion of vastus lateralis. Stress fracture of the patella is a rare cause of anterior knee pain.
Several causes of anterior knee pain can be identified with MRI following anterior cruciate ligament reconstruction including contracture of the retropatellar fat pad and patellar tendon, fibrous hyperplasia or scarring in the peripatellar tissues and the so-called ‘Cyclops lesion’, with bone and/or fibrous tissue lying in front of the anterior cruciate ligament graft in the tibial tunnel (Llopis & Padrón 2007).
The anatomy at the knee makes the structures susceptible to direct and indirect trauma. The menisci and ligaments are often the sites of acute lesions, while the contractile structures are susceptible to overuse as well as acute trauma. The superior tibiofibular joint is mechanically linked to its inferior counterpart and influenced by mechanisms of injury at the foot and ankle.
The onset of the pain is extremely relevant to lesions at the knee. Trauma is a common precipitating cause and the sudden nature of the injury makes it easily recalled by the patient. A direct injury can cause muscular contusion and commonly involves the quadriceps. A direct blow to the patella, such as a fall on the flexed knee, may result in fracture, or may cause contusion of the periosteum or involvement of the prepatellar bursa. A direct blow to the anterior aspect of the upper tibia or, again, a fall on the flexed knee can injure the posterior cruciate ligament.
In contact sports such as rugby and football, the lateral side of the knee is vulnerable to impact, which may result in excessive valgus strain affecting the medial collateral ligament. Injury may be produced by excessive forces applied to the flexed knee while the foot is fixed, e.g. skiing injuries. The medial collateral ligament, anterior cruciate ligament and medial meniscus may be affected. The position of the coronary ligaments involves them in rotational injuries. Major ligamentous rupture, particularly of the anterior cruciate ligament, is usually accompanied by a ‘pop’ or tearing sound as the patient feels the ligament ‘go’ (Edwards & Villar 1993).
Hyperextension injuries can affect any of the ligaments, since all are taut in extension, but the anterior cruciate ligament and medial collateral ligament are most commonly affected. Recalling the exact onset of the injury, the forces involved and the position of the leg at the time of injury will give an idea of the likely anatomy involved in the lesion.
Muscle injuries are common around the knee, as the major muscle groups span two joints and may affect the origin, insertion or mid-belly. Strain results from eccentric contraction (attempting to contract when the muscle is on the stretch), when the muscle is unable to overcome the resistance. Explosive sprinting action affects the hamstrings and the quadriceps, and rectus femoris particularly may be affected by kicking against strong resistance. A direct blow to the quadriceps may cause severe haematoma. Patellar instability, subluxation or dislocation affects the medial quadriceps expansions, vastus medialis or the medial capsule.
Repetitive minor injury results in microtrauma, making the onset of the lesion difficult to recall, and the examiner will have to be aware of contributing factors such as overtraining, training errors, foot posture and faulty knee joint biomechanics. Lateral knee pain due to iliotibial band friction syndrome is common in long-distance runners. Infrapatellar tendinopathy is common in activities associated with jumping and the bursae can be inflamed if any structures passing over them are overused.
The duration of the symptoms will indicate the stage in the inflammatory process reached, or the recurrent nature of the condition. Different treatment approaches depend on the acute, subacute or chronic nature of a ligamentous sprain or muscle belly strain. Overuse lesions around the knee tend to be chronic in nature and are present for some considerable time before the patient seeks treatment.
Recurrent episodes of pain and swelling may be due to instability and derangement of the joint. Patellar subluxation, meniscal lesions or partial ligamentous tears may produce pain and joint effusion after use. Degenerative osteoarthrosis may be symptom-free until overuse triggers a synovitis with increased pain and swelling.
The symptoms and behaviour need to be considered. The behaviour of the pain and the symptoms described by the patient are very relevant to diagnosis at the knee. Immediate pain after injury indicates a severe lesion but pain developing or increasing slowly over several hours may indicate less serious pathology. The ability to continue with the sport or activity after the onset of pain is often indicative of minor ligamentous sprain, whereas major ligament disruption and muscle tears, meniscal lesions or cruciate rupture often result in the patient being totally incapacitated.
Total rupture of a ligament may produce severe pain at the time of injury but, following the initial injury, pain may not be a particular feature since the structure is totally disrupted. Partial ligamentous rupture continues to produce severe pain on movement.
The quality of the pain may indicate severity, but it is important to remember the subjective nature of pain. Aggravating factors can be activity, which indicates a mechanical or muscular lesion, or rest, which indicates a ligamentous lesion with an inflammatory component.
Postures such as prolonged sitting may affect the patellofemoral joint in particular. A pseudo-locking effect often occurs when the patient first gets up to weight-bear. This is not the same as true locking of the knee joint, but is a stiffness experienced by the patient which usually resolves after a few steps. It is thought to be due to excessive friction from changes in the articular cartilage of the patella. Walking, squatting and using stairs all aggravate patellofemoral conditions, particularly going downstairs, when the forces acting on this joint are increased to approximately three times body weight.
The tibiofemoral joint, as the weight-bearing joint, usually produces symptoms on weight-bearing activities, i.e. the stance phase of walking or running or prolonged standing. Pain produced on deep knee bends, rising from kneeling and rotational strains may indicate a meniscal lesion.
The other symptoms described by the patient give important clues to diagnosis. Swelling may be a symptom and it is important to know if it is constant or recurrent or provoked by activity. Swelling that usually occurs quickly within 2–6 h of injury is indicative of haemarthrosis. It can take up to 24 h to appear but this is not its normal presentation. The joint may feel warm to touch and the swelling may be tense. Structures responsible for a haemarthrosis are those with a good blood supply; the anterior cruciate ligament associated with torn synovium being the commonest cause of a haemarthrosis (Shaerf & Banerjee 2008).
Amiel et al (1990) quoted a study by Noyes in which over 70% of patients presenting with acute haemarthrosis of the knee had an acute tear of the anterior cruciate ligament. In children, however, haemarthrosis is more likely to be indicative of an osteochondral fracture than an anterior cruciate ligament injury (Baker 1992). The forces required for rupture of the posterior cruciate ligament are great and therefore the posterior capsule usually tears as well with blood escaping into the calf, where swelling and bruising may have been noticed by the patient.
Swelling which develops more slowly over 6–24 h is synovial in origin due to traumatic arthritis. Structures with a relatively poor blood supply tend to produce this traumatic arthritis, e.g. meniscal lesions, the deep part of the medial collateral ligament involving the capsule of the knee joint and subluxation or dislocation of the patella.
Activity may provoke swelling in conditions such as degenerative joint disease, chronic instability or internal derangement. This may be confirmed after the objective examination which may stir up the condition. Localized swelling may indicate bursitis, e.g. prepatellar bursitis, Baker’s cyst (synovial effusion into the gastrocnemius or semimembranosus bursa due to effusion in the knee joint) or meniscal cyst, which more commonly affects the lateral meniscus.
The presence of an effusion may affect the gait pattern and limit full extension. Reflex inhibition of the quadriceps muscle and an inability to lock the knee gives a feeling of insecurity on weight-bearing with the patient complaining of a sensation of ‘giving way’. Giving way on weight-bearing may also be due to a loose body or meniscal lesion; it is momentary and occurs together with a twinge of pain. Muscle imbalances, particularly involving VMO, may produce a feeling of apprehension as the knee feels as if it will give way. This may occur when weight-bearing after sitting for prolonged periods or walking downstairs.
True locking of the knee is indicative of a meniscal lesion and usually occurs in conjunction with a rotary component to the injury. It has a tendency to recur. The locking may resolve spontaneously over several hours or days or it may need to be manipulatively unlocked. Locking usually occurs at 10–40° short of full extension (Hartley 1995). Meniscal lesions occurring in isolation may present with acute pain and swelling and the patient may report locking or catching. Degenerative meniscal lesions occur in older patients who present with an atraumatic history, mild swelling, joint line pain and mechanical symptoms (Greis et al 2002). A ruptured anterior cruciate ligament can cause locking as the ligamentous flap catches between the joint surfaces. True locking must be distinguished from the pseudo-locking associated with the patellofemoral joint after prolonged sitting.
Provocation of pain on the stairs is important. The patellofemoral joint characteristically produces more pain on coming downstairs, due to the greater joint reaction force, although the pain may also have been provoked while walking upstairs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








