Chapter 10 The Hip
The hip is a ball-and-socket joint in which the femoral head articulates deeply into the acetabulum. This deep fit, combined with thick ligamentous and muscular supporting structures, makes the hip extremely stable but relatively inaccessible. Therefore, the diagnosis of disorders of the hip is sometimes difficult.
Anatomy
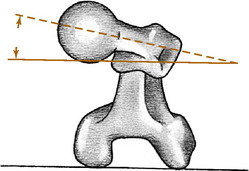
The proximal portion of the femur consists of a head, neck, and greater and lesser trochanters. The axes of the neck and femoral shaft form an angle in the anteroposterior plane: the neck–shaft angle, or “angle of inclination.” This normally measures 125 to 130 degrees. An increase in this angle is termed coxa valga, and a decrease is termed coxa vara. The neck and shaft also form an angle in the transcondylar plane that is referred to as the angle of femoral torsion (Fig. 10-1). Normal femoral torsion is 40 degrees in children, and this decreases to 15 to 20 degrees in adults. Excessive femoral torsion is termed anteversion or antetorsion and is sometimes responsible for in-toeing. A decrease in the normal femoral torsion is termed retroversion or retrotorsion and may cause an out-toeing gait.
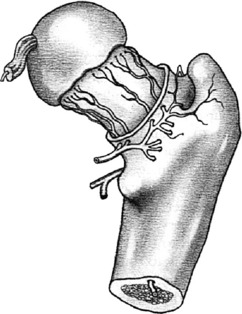
The vascular anatomy of the femoral head is of critical importance in many disorders of the hip. The main sources of blood supply are the retinacular and intramedullary vessels, both of which course from the intertrochanteric region proximally to nourish the femoral head (Fig. 10-2). Diseases or injuries that compromise the circulation may damage the viability of the femoral head and lead to avascular necrosis.
Among the nerves that supply the hip joint is the obturator nerve. This nerve also supplies a sensory branch to the medial side of the thigh and motor supply to some of the hip adductors. Irritation of this nerve from hip joint disease may result in referred pain along the inner aspect of the knee and thigh that may cause confusion with disorders of the knee joint. Therefore, complaints of pain in this area in the absence of physical findings in the knee should always draw attention to the hip joint.
Examination
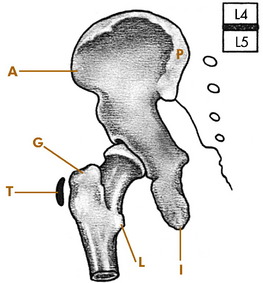
Several bony landmarks are available for orientation on physical examination. The anterior and posterior superior iliac spines and iliac crest are easily palpable because they are not crossed by any muscles (Fig. 10-3). The proximal portion of the iliac crest lies at the level of the fourth lumbar vertebra. The greater trochanter is palpable laterally, and the pubic symphysis is palpable anteriorly. The femoral head lies approximately 2.5 cm distal and lateral to the point where the femoral artery passes beneath the inguinal ligament. This relationship should be recalled when performing venipuncture from the femoral vein. A needle passed through the vein may enter the hip joint and introduce infection into the hip. All femoral venipuncture sites should therefore be meticulously scrubbed and prepared before needle insertion.
Roentgenographic Anatomy
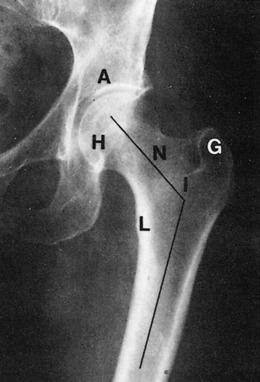
The roentgenographic study of the hip joint should include views in the anteroposterior and lateral planes (Fig. 10-4). The lateral view maybe either a “true” lateral or a “frog leg” exposure that is taken with the hips in maximum external rotation.
Developmental Dysplasia of the Hip
DDH is frequently bilateral, and although the cause is unknown, heredity appears to play a role. Females are affected nine times more often than males, and although the condition may affect both hips, the left is three times more often involved. Firstborn children or children born by breech deliveries also have a higher incidence of the disorder. It is occasionally present in association with clubfoot and congenital muscular torticollis deformities.
CLINICAL FEATURES
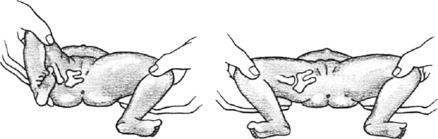
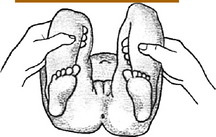
There are no symptoms in the newborn, but most cases are detectable at birth. The clinical picture of the unstable hip will range from minimal findings to obvious frank dislocation, depending on the age of the child. In the newborn, provocative maneuvers, such as Barlow’s and Ortolani’s tests, are commonly used to detect instability. The tests are similar. The Ortolani test refers to the gentle reduction of the dislocated hip by abduction of the flexed hip (Fig. 10-5). This is often accompanied by a soft “clunk,” sometimes called the click of entry. In Barlow’s test, the hip is purposely dislocated by gentle downward pressure of the flexed, adducted hip. With posterior pressure, the femoral head will be displaced out of the acetabulum if the hip is unstable, sometimes called the click of exit. The head is then reduced by gentle abduction of the flexed hip by performing Ortolani’s maneuver. Barlow’s test should not be performed excessively, because it could make the problem worse. Occasionally, this maneuver may result only in a sensation of excessive gliding without an obvious dislocation. This may be an indicator that the hip is subluxable and therefore unstable. Soft clicks sometimes felt during abduction–adduction movements are not considered pathologic unless other findings are present.
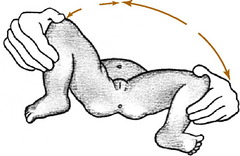
If the diagnosis is made late, the hip is less flexible, and the ability to reduce the dislocated hip by the provocative maneuvers is lessened. At this time, the physical findings may include asymmetry of the skin folds and limited abduction (Fig. 10-6). If the hip is dislocated, it may not be reducible, and other signs may be present, such as shortening of the extremity (Fig. 10-7).
The roentgenographic examination is usually not very helpful when the patient is younger than 3 months of age unless a complete dislocation is present. After this age, a delay in the ossification of the femoral head is frequently noted (Fig. 10-8). The acetabulum may be more inclined vertically, and the acetabular index is often increased. If subluxation or dislocation has occurred, upward and outward displacement of the femoral head will be seen.
Ultrasonography is useful in congenital hip dysplasia, especially in high-risk infants (such as those who are breech delivered or who have a positive family history) or those with uncertain clinical findings. Among its benefits is the elimination of exposure to radiation. Magnetic resonance imaging (MRI) may eventually be helpful, but the diagnosis can usually be established by other means.
TREATMENT
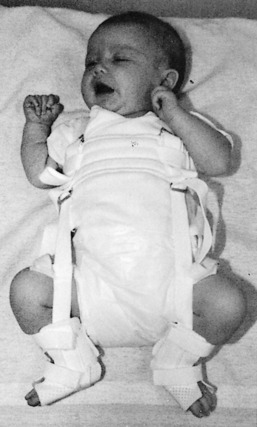
The objective of treatment is to reduce the femoral head into the acetabulum and maintain that reduction. By maintaining the hip in the reduced position, normal development of the hip joint structures and deepening of the acetabulum are encouraged. A variety of external devices are available for the treatment of hip dysplasia or dislocation, the most functional of which is the Pavlik harness (Fig. 10-9). The brace is usually worn for several weeks until the hip is stable.
Legg–Calvé–Perthes Disease
The disease is frequently divided into three stages. The early stage of the disease is characterized by synovitis of the hip joint and early ischemic changes in the ossific nucleus of the femoral head. Roentgenograms taken at this stage reveal joint swelling that may result in lateral displacement of the femoral head. An increase in the opacity of the ossific nucleus is usually present (Fig. 10-10).
TREATMENT AND PROGNOSIS
Referral is indicated whenever the diagnosis is suspected. Treatment recommendations continue to evolve. The ultimate goal of treatment is to prevent deformity of the femoral head while healing is progressing. If a deformity can be prevented, the chances of degenerative joint disease developing at a later date are lessened. The initial goals of treatment are the relief of pain and maintenance of joint motion, which are accomplished by rest to control synovitis. Many children younger than 6 years of age with minimal involvement have a good prognosis and require only symptomatic care. The older child who is at risk for having a poor outcome may require treatment. In these children, treatment is aimed at keeping the femoral head centered in the acetabulum. If the head is contained in the acetabulum while it is re-forming, the acetabulum will “mold” the head and prevent significant deformity from occurring. These goals of treatment are usually accomplished by the use of an abduction brace that allows motion but contains the head in the acetabulum (Fig. 10-11). The brace must be worn continuously for up to 2 years, although the results of specific forms of treatment remain inconclusive, and some investigators advocate only nighttime bracing. Surgery may be necessary in select cases.
Slipped Capital Femoral Epiphysis
Slipped capital femoral epiphysis is a disorder of unknown cause in which weakening of the epiphyseal plate of the upper femur occurs and results in upward and anterior displacement of the femoral neck. The actual amount of displacement varies. In most cases, the slippage is gradual, and some elements of healing are usually present. The condition is seen most commonly in boys between the ages of 11 and 16 years during their rapid growth spurt. The disorder is bilateral in 25% of cases and frequently occurs in two distinct body types. The first is the slender, tall, rapidly growing boy, and the second is the large, obese boy with underdeveloped sexual characteristics. The presence of the disorder in these two body types suggests a hormonal cause, but none has been proved.
CLINICAL FEATURES
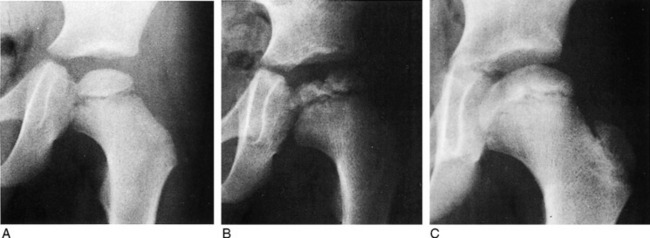
In the early “preslipping” stage, the roentgenogram characteristically reveals irregular widening of the epiphyseal plate and joint swelling (Fig. 10-12). As displacement occurs, a line drawn along the superior or anterior neck of the femur will transect less of the femoral head than normal. This may be more readily seen on the lateral view. More severe degrees of slippage are usually easily diagnosed.
A condition similar to slipped capital femoral epiphysis is termed acute traumatic separation of the upper femoral epiphysis (Fig. 10-13). This is actually an epiphyseal fracture and has a much poorer prognosis than the gradual slippage that occurs in slipped capital femoral epiphysis.
TREATMENT
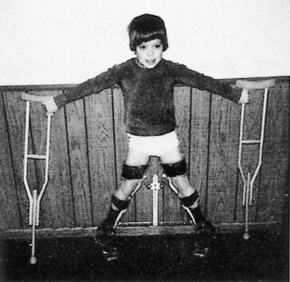
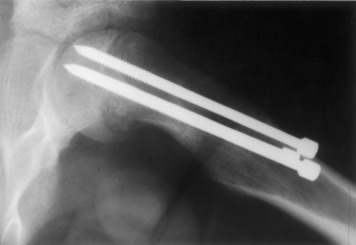
As soon as the diagnosis is made, a referral for surgery is indicated. The patient is immediately placed on crutches, and weight bearing is prohibited. Traction in the hospital may be necessary to reduce the acute component of the slippage. To prevent further slippage from occurring, the femoral head is fixed to the neck, generally by using small pins (Fig. 10-14). Weight bearing is prohibited for several months until the epiphyseal plate closes. Severe deformities may also require osteotomy of the femur.
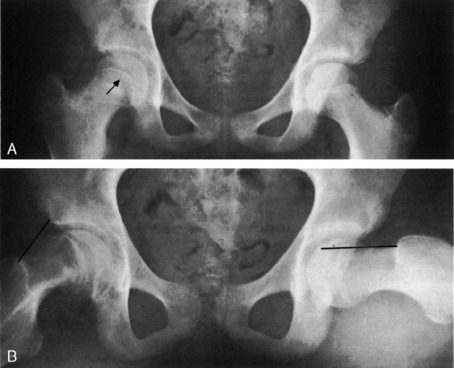
The prognosis is usually good, except in those cases with acute traumatic separation. The chronic form may result in slight shortening of less than 1.25 cm along with a mild external rotation deformity. In cases with acute traumatic separation, avascular necrosis of the femoral head is a common complication, and this usually results in severe traumatic arthritis of the hip (Fig. 10-15). The more common chronic slippage does not usually cause avascular necrosis.
Transient Synovitis (Irritable Hip)
CLINICAL FEATURES
The roentgenograms may reveal swelling of the capsule and adjacent soft tissue but are usually normal. Slight widening of the joint space may be present, but there are no changes in bone texture. Ultrasonography may help determine the presence of excessive joint fluid.