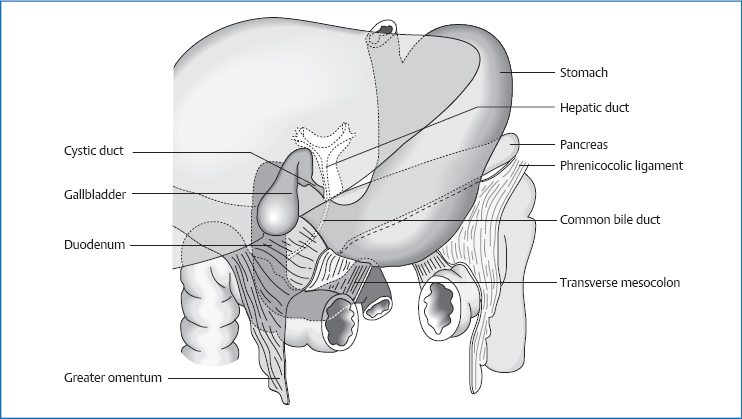
6 The Gallbladder The gallbladder is a hollow pear-shaped organ that measures 8–12cm in length and 4–5cm in width. Its capacity lies around 40–70 mL; it is the storage organ for the bile. It is divided into: The hepatic duct (drainage path from the liver for the bile) and cystic duct (drainage path from the gallbladder) combine to form the common bile duct, which via the ampulla of Vater (major duodenal papilla) leads to the descending part of the duodenum. The hepatic duct is 3–4cm long and measures 3–4mm in diameter. The common bile duct is about 6cm long and measures 5–6mm in diameter. At the mouth it narrows to about half this. The mucous membrane of the neck of the gallbladder is folded into spirally shaped creases. This prevents an uncontrolled excretion of bile. Fig. 6.1 Location of the gallbladder. The gallbladder is located intraperitoneally on the posterior side of the liver. The axis of the gallbladder runs from caudal, anterior right, to cranial, posterior left. The fundus of the gallbladder is found at the Murphy point: draw a line connecting the navel to the right nipple or the medioclavicular point on the right. The fundus of the gallbladder can be palpated at the point where this line crosses the lower costal arch on the right. In children, this point is located further medially. The cystic duct and hepatic duct combine to form the common bile duct in the hepatoduodenal ligament at the height of the lower edge of L1. The common bile duct lies about 10–15cm below the anterior torso wall. Its initial part still runs inside the ligament, i.e., intraperitoneally. At the upper edge of the superior part of the duodenum, it crosses to the posterior side of the duodenum; here its location becomes retroperitoneal. It forms an arch to the right, crosses the head of the pancreas, enters the descending part of the duodenum from posteriorly, and ends at the major duodenal papilla at approximately the height of L3. It forms a crease that is about 2cm long on the posterior side of the descending part before it ends there. Cystic artery (from the proper hepatic artery). Fig. 6.2 Topographic relationships of the gallbladder. Cystic vein (to portal vein). Maximal time: 11 p.m.–1 a.m. Minimal time: 11 a.m.–1 p.m. For basic information, see page 34. In its mobility, the gallbladder is coupled to the mobility of the liver. We do not find any separate mobility. The common bile duct performs an S-shaped movement: during exhalation, we first detect a movement in a posterior–medial and then in an anterior–lateral direction; during inhalation, it is in the opposite direction. The gallbladder is motorically coupled to the liver. The liver produces 800–1000mL of bile per day. This bile is concentrated 10- to 12-fold in the gallbladder by removing water and electrolytes stored there. The bile salts are produced in the liver from cholesterol and the amino acids glycine and taurine. They activate lipase in the small intestine and pancreas and, as separate molecules, possess hydrophilic (amino acids) and lipophilic (cholesterol) sides. In the intestinal lumen, the bile salts combine with the products of lipolysis (glycerin and fatty acids) to form micelles. In this form, the fatty acids, which have a low solubility in water, can be emulsified in the watery environment of the intestines and absorbed by the mucous membranes of the small intestine. In the terminal ileum, the bile salts are reabsorbed, transported back to the liver, and again excreted into the bile (enterohepatic cycle). A bile salt molecule runs through this cycle about 18 times. If bile salts are not reabsorbed in the ileum, they increase the water permeability of the epithelium in the colon (chologenic diarrhea). Bilirubin is a product of the breakdown of hemoglobin from the erythrocytes. Hemoglobin is broken down in the liver into water-soluble bilirubin (conjugated with glucuronic acid) and excreted into the bile. In the intestines, bilirubin is broken down by bacteria through several intermediate stages to urobilin and stercobilin. These end-products are responsible for the normal coloration of stools. If the passage through the intestines is too quick, the bacteria do not have enough time to break the bilirubin down completely—the stool is yellow. In cases of cholestasis, bilirubin is lacking in the intestines and the stool is gray. Some of the bilirubin and its metabolites are introduced into an enterohepatic cycle and finally excreted with the urine. This is the reason for the typical yellow color of urine. The secretion of bile from the liver is steered by concentration of bile salts in the blood plasma—insulin, glucagon, secretin, and cholecystokinin (CCK). The vagus nerve, secretin, gastrin, and CCK direct the voiding of the gallbladder. CCK is the strongest stimulus for the gallbladder’s contraction: when mashed food arrives in the duodenum, it is stretched. As a result, CCK is secreted into the blood, and a parasympathetic stimulus causes the muscular contraction of the gallbladder, which leads to voiding. At the sphincter of Oddi, the parasympathetic stimulus causes a drop in tonicity—the sphincter opens. However, the flow of bile from the gallbladder starts even before the food arrives in the stomach: peristalsis in the esophagus reflexively triggers the contraction of the gallbladder and relaxation of the sphincter of Oddi (enteroenteral reflex). The direction of bile flow into the gallbladder or duodenum is guided by the pressure conditions in the sphincter of Oddi, bile ducts, and the gallbladder. During the interdigestive phase, the sphincter of Oddi is closed and the pressure there is greater than in the bile ducts and gallbladder. As a result, the bile that is secreted in the liver flows through the cystic duct into the gallbladder. Gallbladder contractions cause the pressure in the gallbladder to rise to the point where it surpasses the pressure in the sphincter. Bile from the liver and gallbladder flows into the intestines. In addition, the hormonally guided gallbladder contractions also lower tonicity in the sphincter of Oddi—so the pressure there drops at the same time as the gallbladder is voided. The ampulla of Vater also runs into the pancreatic duct. Normally, the pressure in this duct is so great that bile juices cannot flow into the pancreas. When the ampulla is blocked, e.g., by a gallstone, this can cause the flow of bile to reverse in the direction of the pancreas. Definition. Formation of cholesterol, pigment, or calcium stones in the gallbladder, or intra- or extrahepatic bile ducts; 99% of these stones are cholesterol stones. Causes. Predisposing factors include: Clinical. Approximately 50% of cases run their course silently. There is abnormal, right-sided, upper abdominal pain after eating. If a stone is stuck in the bile ducts, colic pain in the right upper abdomen radiates into the right shoulder. Definition. Inflammation of the wall of the gallbladder, most commonly the result of cholelithiasis. Definition. In most cases, we are dealing with adenocarcinomas.
Anatomy
General Facts
 the fundus
the fundus
 the body
the body
 the neck
the neck
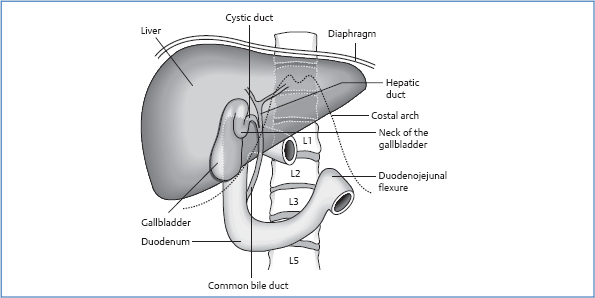
Location
Projection onto the Wall of the Torso
Topographic Relationships
Gallbladder
 liver
liver
 duodenum
duodenum
 greater omentum
greater omentum
 lesser omentum
lesser omentum
 peritoneum
peritoneum
Common Bile Duct
 hepatoduodenal ligament
hepatoduodenal ligament
 proper hepatic artery
proper hepatic artery
 portal vein
portal vein
 posterior side of the superior part of the duodenum
posterior side of the superior part of the duodenum
 pancreas
pancreas
 major duodenal papilla and descending part of the duodenum
major duodenal papilla and descending part of the duodenum
 inferior vena cava
inferior vena cava
Attachments/Suspensions
 turgor
turgor
 organ pressure
organ pressure
 connection to the liver via connective tissue
connection to the liver via connective tissue
Circulation
Arterial
Venous
Innervation
 sympathetic nervous system from T7 to T10 via the greater and lesser splanchnic nerve
sympathetic nervous system from T7 to T10 via the greater and lesser splanchnic nerve
 switchover in the celiac plexus
switchover in the celiac plexus
 vagus nerve
vagus nerve
 phrenic nerve, sensory branch
phrenic nerve, sensory branch
Organ Clock
Organ–Tooth Interrelationship
Movement Physiology according to Barral
Mobility
Motility
Physiology
Composition of Bile in the Gallbladder
 water and salt in isotonic proportions; the pH value is neutral to lightly alkaline
water and salt in isotonic proportions; the pH value is neutral to lightly alkaline
 phlegm
phlegm
 bile pigments (bilirubin; also in small amounts biliverdin)
bile pigments (bilirubin; also in small amounts biliverdin)
 bile salts
bile salts
 cholesterol
cholesterol
 steroid medications and other foreign substances
steroid medications and other foreign substances
Pathologies
Symptoms that Require Medical Clarification
Cholelithiasis
 diabetes mellitus
diabetes mellitus
 cirrhosis of the liver
cirrhosis of the liver
 diseases of the terminal ileum
diseases of the terminal ileum
 pregnancy
pregnancy
 oral contraceptives
oral contraceptives
Cholecystitis
Causes
 impacted stones
impacted stones
 invasion by intestinal germs
invasion by intestinal germs
Clinical
 nausea
nausea
 vomiting
vomiting
 fever
fever
 scleral icterus
scleral icterus
 positive Murphy sign
positive Murphy sign
Gallbladder Carcinoma
Causes
 cholelithiasis (in 95 % of diseases, this is the previous medical history)
cholelithiasis (in 95 % of diseases, this is the previous medical history)
 adenomas of the gallbladder
adenomas of the gallbladder
Clinical
 obstructive icterus
obstructive icterus
Osteopathic Practice
Cardinal Symptom
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




