CHAPTER 25 The Failed Uni
 Despite advances in prosthetic component design, newly developed instrumentation and surgical technique, and appropriate patient selection, failure after unicompartmental knee arthroplasty can occur. As the number of unicompartmental knee arthroplasties performed continues to rise, so too will the number of failures.
Despite advances in prosthetic component design, newly developed instrumentation and surgical technique, and appropriate patient selection, failure after unicompartmental knee arthroplasty can occur. As the number of unicompartmental knee arthroplasties performed continues to rise, so too will the number of failures. The current recommendation for management of the failed unicompartmental arthroplasty is conversion to total knee arthroplasty. In the majority of cases, the conversion of unicondylar arthroplasty to total knee arthroplasty can successfully be performed with the same approach used in primary total knee arthroplasty.
The current recommendation for management of the failed unicompartmental arthroplasty is conversion to total knee arthroplasty. In the majority of cases, the conversion of unicondylar arthroplasty to total knee arthroplasty can successfully be performed with the same approach used in primary total knee arthroplasty. Failure mode can be predictive of complexity of the conversion of unicompartmental arthroplasty to total knee arthroplasty. Failure modes have included polyethylene wear, progression of arthritis, patellofemoral symptoms, aseptic loosening, malpositioned implants, medial tibial collapse, poor patient selection, and technical factors.
Failure mode can be predictive of complexity of the conversion of unicompartmental arthroplasty to total knee arthroplasty. Failure modes have included polyethylene wear, progression of arthritis, patellofemoral symptoms, aseptic loosening, malpositioned implants, medial tibial collapse, poor patient selection, and technical factors. Polyethylene wear, with or without loosening, and progressive arthritis have been the most common failure modes reported with contemporary unicompartmental knee arthroplasty designs. When unicompartmental knees fail through these modes, the revision procedures are straightforward with minimal bone loss.
Polyethylene wear, with or without loosening, and progressive arthritis have been the most common failure modes reported with contemporary unicompartmental knee arthroplasty designs. When unicompartmental knees fail through these modes, the revision procedures are straightforward with minimal bone loss. When failure occurs in unicompartmental knee arthroplasty due to early collapse of the medial tibial plateau, there are more significant bone defects, and revisions are technically more demanding than that seen with other aseptic failure mechanisms such as polyethylene wear.
When failure occurs in unicompartmental knee arthroplasty due to early collapse of the medial tibial plateau, there are more significant bone defects, and revisions are technically more demanding than that seen with other aseptic failure mechanisms such as polyethylene wear. Early failure is typically related to inappropriate patient selection, infection, medial tibial collapse, or poor surgical technique leading to ligament instability, malpositioning of the implant, or component loosening. The more common modes of failure include polyethylene wear, progression of tricompartmental arthritis, or component loosening, and will occur late after the first or second decade.
Early failure is typically related to inappropriate patient selection, infection, medial tibial collapse, or poor surgical technique leading to ligament instability, malpositioning of the implant, or component loosening. The more common modes of failure include polyethylene wear, progression of tricompartmental arthritis, or component loosening, and will occur late after the first or second decade. In general, late failures are less demanding and can usually be converted using a cruciate-retained or posterior-stabilized primary total knee arthroplasty, without supplemental stabilization or constraint.
In general, late failures are less demanding and can usually be converted using a cruciate-retained or posterior-stabilized primary total knee arthroplasty, without supplemental stabilization or constraint. The surgical approach follows the same principles of primary total knee arthroplasty using standard primary total knee arthroplasty instrumentation. One of the most important technical aspects of the procedure is to leave the unicompartmental arthroplasty implants intact as long as possible.
The surgical approach follows the same principles of primary total knee arthroplasty using standard primary total knee arthroplasty instrumentation. One of the most important technical aspects of the procedure is to leave the unicompartmental arthroplasty implants intact as long as possible. Resection of the patella can be performed first in order to facilitate the exposure to the distal femur. This will also avoid eversion of the patella, which will minimize the soft tissue trauma to the extensor mechanism.
Resection of the patella can be performed first in order to facilitate the exposure to the distal femur. This will also avoid eversion of the patella, which will minimize the soft tissue trauma to the extensor mechanism.Introduction
The popularity of unicompartmental knee arthroplasty has continued to grow over the last decade and is one of the main treatment alternatives for isolated degenerative arthritis of the knee.1–3 Since its introduction, unicondylar arthroplasty has been an alternative to total knee arthroplasty or high tibial osteotomy for the treatment of unicompartmental knee arthritis. The benefits of this procedure are attributed to the ability to provide a more rapid rehabilitation time, greater range of motion, preservation of bone stock, and more normal knee kinematics with the retention of both the anterior and posterior cruciate ligaments. With improvements in component design, surgical technique, and patient selection criteria, improved clinical outcomes have been reported in the literature. Berger et al. reported on a prospective study of 62 unicompartmental knee arthroplasties with a mean follow-up of 12 years.3 They noted no loose components or periprosthetic osteolysis, with a 10-year survival rate of 98%. Price et al. also noted a 93% 10-year survival using the Oxford unicompartmental knee implant.4 Because of these encouraging results, the prevalence of unicompartmental knee arthroplasty has increased significantly over the years. Between 1996 and 1997, unicondylar knee arthroplasty comprised only 1% of the U.S. total knee market.5 This increased to 6% of all total knees performed in the United States between 2000 and 2001. Between 1998 and 2005, there has been a 10% per year increase in the number of unicompartmental knee arthroplasty procedures performed in the United States alone.6 This growth rate is approximately three times that for total knee arthroplasty, and presently it is estimated that 12% of all total knees performed in the United States are unicompartmental knee arthroplasties.
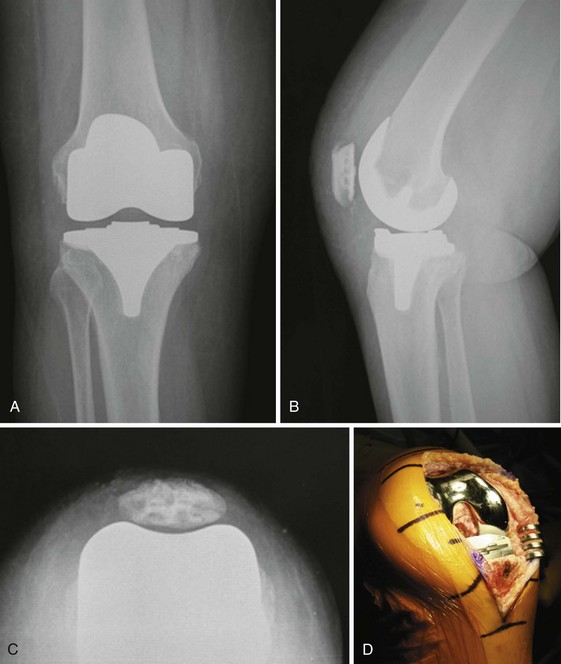
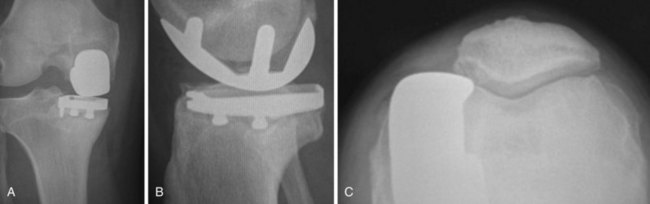
Although early midterm studies cite a high rate of satisfactory results after unicompartmental knee arthroplasty, long-term survivorship and outcome continue to be a concern. Long-term survivorship of unicompartmental knee arthroplasty has been improving with the advancement in prosthetic component design, newly developed instrumentation and surgical technique, and appropriate patient selection. Despite advances, failure after unicompartmental knee arthroplasty can occur. When compared with total knee arthroplasty as an index arthroplasty procedure, however, the cumulative revision rate for unicompartmental knee arthroplasty tends to be higher.7,8 Gioe et al. evaluated more than 5000 total knee arthroplasties in a community registry and noted that unicondylar arthroplasty was 7.2 times as likely to fail compared to an all-polyethylene cemented total knee arthroplasty.9 The Norwegian Arthroplasty Registry echoed some of these same concerns, noting two times the revision rate with unicompartmental arthroplasty versus total knee arthroplasty in their evaluation of more than 2200 unicondylar knees.10 In the Swedish Registry, Lindgren et al. found a greater than 10% cumulative revision rate at 10 years for unicondylar arthroplasty, with only a 5% cumulative revision rate for total knee arthroplasty.11 In the Australian Registry, results were equally concerning with their 5-year revision rate of 8.9%.12 As the number of unicompartmental knee arthroplasties performed continues to rise, so too will the number of failures. Early investigations reported technical difficulty during conversion of unicompartmental knee arthroplasty to total knee arthroplasty, citing substantial bone loss requiring bone grafting, stemmed revision components, or the need for custom implants.8,13 More recently, with improvement in surgical technique and prosthetic designs, conversion of unicompartmental knee arthroplasty to total knee arthroplasty has been described as less technically demanding than a revision total knee arthroplasty with results comparable to the results of primary total knee arthroplasty, in terms of both function and survivorship14 (Figs. 25–1 and 25–2).
Clinical Evaluation and Preoperative Planning
The current recommendation for management of the failed unicompartmental arthroplasty is conversion to total knee arthroplasty.15 In the majority of cases, the conversion of unicondylar arthroplasty to total knee arthroplasty can successfully be performed with the same approach used in primary total knee arthroplasty. Primary total knee arthroplasty components and instrumentaion can be used. In most cases, however, it is essential to be prepared for any technical difficulties that may arise requiring stem fixation, metal augments, bone grafting, or a more constrained component (Figs. 25–3 and 25–4). Preoperative evaluation is critical in the planning process. Berend et al. have shown that the mode of failure is predictive in determining complexity of conversion and can assist in the planning for special instrumentation, or more complex reconstructive options.15
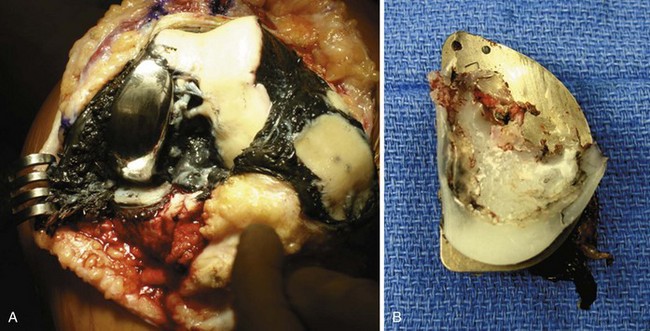
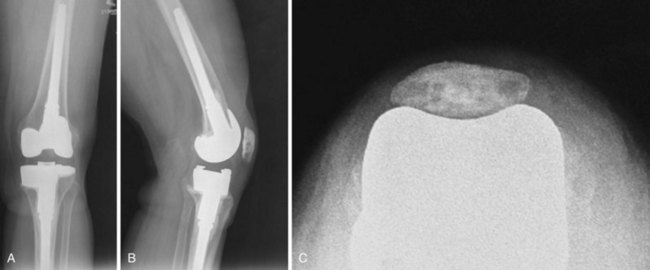
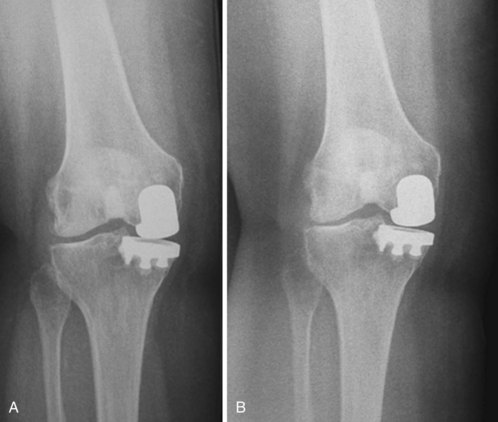
Factors leading to unicompartmental knee arthroplasty failure have been shown to differ based on whether failure has occurred early or late. Early failure is typically related to inappropriate patient selection, infection, medial tibial collapse, or poor surgical technique leading to ligament instability, malpositioning of the implant, or component loosening. The more common modes of failure include polyethylene wear, progression of tricompartmental arthritis, or component loosening, and will occur late after the first or second decade16 (Fig. 25–5). In general, late failures are less demanding and can usually be converted using a cruciate-retained or posterior-stabilized primary total knee arthroplasty, without supplemental stabilization or constraint.17 If failure occurs secondary to medial tibial collapse or excessive resection of tibial bone, a more complex reconstruction will typically be required. Aleto et al., in a retrospective review of 32 knees converted to total knee arthroplasty, found that the most common mode of failure was related to medial tibial collapse (47% of the study group)16 (see Fig. 25–1). Of these, 87% were an all-polyethylene design, and 7 of 15 failed in less than 16 months and required a more complex reconstruction with stems, augments, and screws. In addition, they also found tibial component slope to be associated with the direction of the collapse of the implant into the tibia. Excessive posterior tibial component slope, with a mean of 12.0°, was associated with posterior failure. When failure mode is related to medial tibial collapse, more significant bone loss can be expected, and most likely will require a more complex reconstruction (Fig. 25–6).
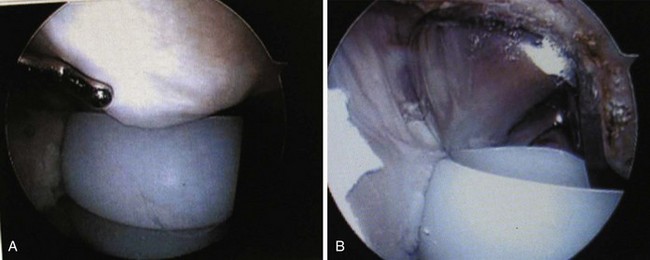
A thorough evaluation prior to surgery should be undertaken with all patients to accurately determine the cause of failure. This should include a detailed history, physical examination, radiographic evaluation, knee fluid analysis, and appropriate laboratory assessment. As in all knee arthroplasty patients, with any type of failure, it is important to consider septic arthritis until proven otherwise. Initial screening methods should be performed as in total knee arthroplasty with joint fluid analysis, including cell count, culture and sensitivity, Gram stain, and assessment for crystals. Peripheral blood evaluation should also be performed, including complete blood count, erythrocyte sedimentation rate, and C-reactive protein, as well as bone scan and sulfur colloid technetium bone scanning if indicated. A detailed physical examination should also be conducted to rule out elements of instability, with particular reference to the anterior cruciate ligament as well as the collateral ligaments. Injury or deficiency of the anterior cruciate ligament or medial collateral ligament can compromise function of the knee in the setting of unicompartmental knee arthroplasty. Lateral joint line tenderness with associated joint effusion may indicate meniscal pathology involving the opposite compartment and sometimes can be addressed with arthroscopic methods alone. Similarly, intra-articular scarring may cause impingement within the joint space, which can contribute to persistent postoperative pain and many times can be treated successfully with knee arthroscopy (Fig. 25–7).
It is important to note that the diagnosis of meniscal pathology, or intra-articular scarring, is based on history and clinical examination alone. It is therefore essential to first rule out all other causes for persistent pain and failure of unicompartmental arthroplasty. Standing weight-bearing radiographs are essential for evaluation of the femoral tibial joint space, which should include a standing bilateral anteroposterior view, a 45° flexion posteroanterior weight-bearing view, and lateral and skyline views. A long-leg standing weight-bearing (1.37 cm) axial alignment radiograph is also necessary to further evaluate the anatomic and mechanical axis of the knee (Fig. 25–8). Any progressive change of alignment may be an indication of medial tibial collapse, or possible progressive degeneration of the opposite compartment. Radiographic evaluation is also important in order to determine any evidence of radiolucent lines or concerns for component loosening or wear of polyethylene (Fig. 25–9). Serial comparison of radiographs over time is extremely helpful as changes in alignment, collapse of the tibia, or progression of arthritis can occur gradually, and sometimes can only be appreciated with prior comparison views (Fig. 25–10). Assessment of bone loss, on either the femoral or tibial side, is also important in planning the need for a more complex reconstruction requiring metal augments, stems, or a more constrained revision component. Templating the level of resection on radiographs can help in this planning process to more accurately predict the need for augmentation.
Setup and Technique
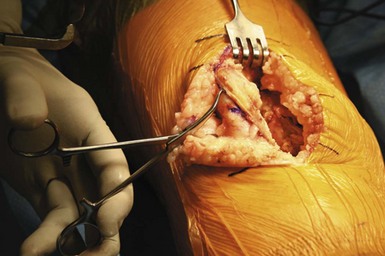
After confirmation of the preoperative plan, examination under anesthesia should be performed first. This will allow for further assessment of passive range of motion and collateral ligament stability, as well as the integrity of the anterior and posterior cruciate ligaments. The procedure is approached in a manner similar to that of primary total knee arthroplasty utilizing general or regional anesthesia. A short-acting spinal anesthetic with light sedation is preferable, as this will allow for a more successful approach with pain management. This has also been very beneficial in initiating early weight bearing and recovery of quadriceps muscle function within hours after the procedure. After induction of anesthesia, the patient is positioned in the supine position, with a small bolster placed at the foot of the bed to allow for knee flexion between 70° and 90° (Fig. 25–11). A specific leg holder is not necessary, and many times can cause further constraints of the tibia, affecting internal and external rotation during the surgical procedure.
Resection of the patella can be performed first in order to facilitate the exposure to the distal femur. This will also avoid eversion of the patella, which will minimize the soft tissue trauma to the extensor mechanism. Patellar resection is performed using the same principles followed in total knee arthroplasty with a measured resection approach. Using a towel clip, the patella can be easily everted and stabilized for preparation (Fig. 25–12). Removing the surrounding synovial tissue from the periphery of the patella is helpful in accurately identifying the level of resection. Once the periphery of the patella is cleared of synovial tissue to define its margins, a measured resection can be performed. It is important to restore the native patellar thickness to avoid overstuffing the patellofemoral joint, which can affect patellar articulation, patellar tracking, and range of motion. The patella should be measured using calipers in all four quadrants in order to retain the normal patellar height in the most accurate manner, and to avoid an oblique level of resection (Fig. 25–13). Transverse patellar osteotomy can be performed utilizing a freehand method or instrument method, depending on the surgeon’s preference (Fig. 25–14). The resection level should be parallel, and once again, assessment should be made with the caliper in all four quadrants to avoid the risk of an oblique cut, and any abnormality with patellar tracking (Fig. 25–15). Sizing of the patella can then be performed in the usual manner, taking care to medialize the patella to prevent any overhang beyond the margins of the bone (Fig. 25–16). The thickness of the patella should then be reassessed following insertion of the prosthetic component trial. Ideally the goal is to have the thickness of the remaining patella and the patellar prosthesis equal to the appropriate patellar thickness.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree