The Essentials of the Needle EMG Exam
Vivek Kadyan
Ernest W. Johnson
Denise L. Davis
Why Request an EMG?
An electromyographic (EMG) examination is a functional evaluation of the motor unit. It can assess the location, severity, chronology, and prognosis of injuries, diseases, or other compromises of the motor unit. The motor unit is made up of the anterior horn cell, its axon, and all of the muscle fibers innervated. Some wish to characterize electrodiagnosis as synonymous with EMG, and that is historically and conventionally correct, if not correct technically. Most electromyographers in the United States understand that when an EMG is requested, the referring physician desires a comprehensive electrodiagnostic examination, which is a specialty medical consultation that includes EMG testing. This testing is performed either by or under the personal supervision of the physician, and is guided by the clinical information of the interview and clinical examination. Another important point is that the functional evaluation provided by electrodiagnostic evaluation is complementary to imaging’s structural evaluation, and electrodiagnosis is essential to evaluate any trauma or disease affecting the motor unit.
What Conditions Suggest that EMG Would Be useful in Diagnosis and Management?
If the patient complains of pain, weakness, fatigue, or numbness (paresthesia) that results in a differential diagnosis including problems affecting the motor unit or sensory nerves, then an EMG may be useful. The most frequent complaint of patients presenting in a primary care office is “pain.” Pain is commonly caused by:
Radiculopathy
Entrapped nerve
Neuritis (generalized or localized)
A variety of nonneurologic causes
Weakness can be seen as either localized or generalized, and this clinical impression will affect the choice of electrodiagnostic tests. Fatigue is differentiated from weakness as the gradual loss of strength during repeated or continuous use of muscle(s).
Paresthesias (numbness) also can be either localized or generalized to multiple limbs and is a very common condition leading to EMG.
What is Electromyography?
Electromyography literally means recording the electrical activity of the muscle cell membrane. With a needle electrode inserted in the muscle, the motor unit potential (MUP) can be recorded. This represents the summated electrical activity of action potentials of all of the muscle fibers making up that motor unit. In the normal situation, the motor unit (MU) is “all or none” in its expression as a MUP. In certain circumstances the action potential
of individual muscle cell membranes can be recorded. This portion of the EMG is described in more detail below in the section on Needle EMG. In more recent usage, the word “electromyography” encompasses all the techniques used in evaluating the function of the peripheral nervous system, including the lower motor neuron and its innervated muscle fibers (the MU), and the associated sensory nerve fibers. In conditions that affect the muscle fibers primarily, this MUP will be smaller and of shorter duration. If the anterior horn cell or its axon is impaired, then the MUP will be absent. Also, if the axon is damaged or the sheath (myelin) is defective, then the resulting MUP will be delayed in onset, unstable in appearance, or altered in shape (i.e., increased duration or reduced amplitude).
of individual muscle cell membranes can be recorded. This portion of the EMG is described in more detail below in the section on Needle EMG. In more recent usage, the word “electromyography” encompasses all the techniques used in evaluating the function of the peripheral nervous system, including the lower motor neuron and its innervated muscle fibers (the MU), and the associated sensory nerve fibers. In conditions that affect the muscle fibers primarily, this MUP will be smaller and of shorter duration. If the anterior horn cell or its axon is impaired, then the MUP will be absent. Also, if the axon is damaged or the sheath (myelin) is defective, then the resulting MUP will be delayed in onset, unstable in appearance, or altered in shape (i.e., increased duration or reduced amplitude).
Another alteration in the MUP will occur if there is a disease or injury to the endplate area (where the motor axon terminal synapses on the muscle fiber). This contact of axon to muscle is referred to as the neuromuscular junction, and in certain conditions (e.g., myasthenia gravis, Lambert-Eaton syndrome, or botulism) the nerve impulse can be intermittently delayed or blocked in reaching the muscle fiber, thus changing the MUP‘s characteristic stability.
What is Nerve Conduction Velocity?
When the motor nerve is maximally stimulated, all of the MUs in that muscle respond by depolarizing, and a surface electrode will record the electrical activity as a compound muscle action potential (CMAP), which is a fairly good measure of the number of motor axons and their MUAPs responding. Some electromyographers (mostly in Europe) call this procedure “neurography.” While they maintain this is more accurate, in motor conduction it is mostly dependent on the appearance of the CMAP as well as the latency; thus, myography is appropriate. We therefore prefer to use the shortened but historically valid and generally accepted term “electromyography” as a reasonable compromise for all of these neurophysiologic studies. With the inclusion of late waves such as the F wave, H reflex, A wave, blink reflex, and somatosensory evoked potentials (SEP) in some examinations, one must also consider using central and peripheral action potentials in the description.
When a nerve is stimulated the resulting action potentials can be recorded with surface electrodes or with “near nerve” needle recording either proximal or distal to the stimulation site. The conduction velocity can be calculated by dividing the distance by the latency time to onset of the response. A semiquantitative measure of the number of functioning axons is represented by the amplitude of the nerve action potential. If a purely sensory nerve, it is referred to as the sensory nerve action potential (SNAP); if recorded over a mixed nerve, it is referred to as the compound nerve action potential (CNAP). For greater accuracy, one should subtract 0.1 ms from the latency before division—this is the “latency of activation,” technically the time between application of stimulus and activation of the axon (i.e., velocity = distance [in mm]/[latency – 0.1 (in ms)]). This time does not present a significant consideration in adults except in very short distances. However, in newborns it could make a difference in small hands with 1.5- to 2-ms latencies.
Needle EMG
There are over 400 separate muscles in the body that could be investigated with a needle electrode. With knowledge of anatomy and the probable causes of weakness or pain, one can plan the needle
examination to minimize the number of muscles explored and narrow the diagnostic probabilities. There are five steps to this needle EMG exam to be performed and analyzed as each muscle is explored with the needle electrode.
examination to minimize the number of muscles explored and narrow the diagnostic probabilities. There are five steps to this needle EMG exam to be performed and analyzed as each muscle is explored with the needle electrode.
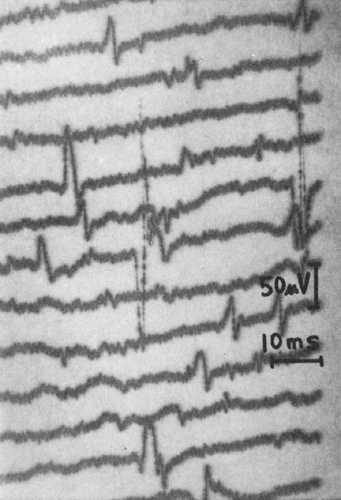
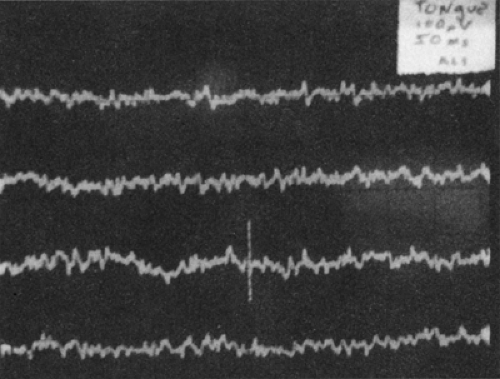 Figure 2-1 • A small, isolated fasciculation potential is recorded in a patient with amyotrophic lateral sclerosis. Total time duration of the recording is 2 s (gain = 100 μV, sweep = 50 ms). |
Step I: Needle in Quiet Muscle (at Rest)
Note spontaneous electrical activity:
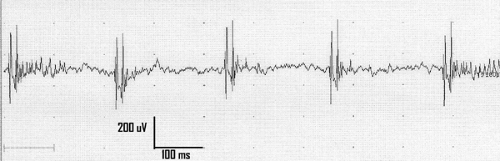
Fasciculation potentials: these are recognized by their irregular and slow rate of spontaneous firing (Figs. 2-1 and 2-2) and classified by their shape: simple (usually diphasic or triphasic); complex (either the usual polyphasic MUP or repetitive discharge polyphasic); myokymic discharges (groups of MUPs firing together) (Fig. 2-3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree