Chapter 6. The elbow
SUMMARY
To aid diagnosis and accurate treatment, the chapter begins by outlining the relevant anatomy and provides guidelines for palpation. A commentary on the history and objective sequence follows, leading to discussion of the lesions that may be encountered, with suggestions for their effective treatment and management.
ANATOMY
Inert structures
Together with the shoulder, the elbow functions to position the hand in space. Anatomically the elbow consists of two articulations, the elbow joint proper and the superior radio-ulnar joint, both contained within the same joint capsule.
The elbow joint proper is a synovial hinge joint between the distal end of the humerus, comprising the capitulum and trochlea, and the proximal ends of the radius and ulna. The articular capsule surrounds the articular margins, originating anteriorly around the coronoid and radial fossae of the humerus and inserting into the annular ligament and anterior border of the coronoid of the ulna. Posteriorly it attaches to the olecranon fossa of the humerus and the olecranon of the ulna.
In common with other synovial hinge joints, the relatively weak articular capsule is reinforced by strong collateral ligaments. The medial collateral ligament fans out from the medial epicondyle, where it is closely related to the common flexor tendon and primarily resists valgus stresses. The lateral collateral ligament is a strong triangular band fanning out from the lateral epicondyle, where it underlies and shares a close anatomical relationship with the common extensor tendon. It runs on to blend with the annular ligament below. The radial collateral ligament stabilizes the radial head, preventing varus stresses, and the annular ligament stabilizes the superior radioulnar joint. The elbow joint has two axes of motion and thus a greater inherent stability than the shoulder (Miyasaka 1999).
The capitulum is roughly hemispherical in shape and articulates with the radial head. The trochlea is pulley- or spool-shaped and extends from the anterior aspect of the distal end of the humerus to the olecranon fossa posteriorly. Its prominent medial ridge provides a valgus tilt which contributes to the carrying angle of the elbow joint. It articulates with the trochlear notch of the ulna.
On the distal anterior surface of the humerus sit the radial and coronoid fossae, accommodating the rims of the radial head and coronoid process of ulna in full flexion. The olecranon fossa of the humerus accepts the olecranon process of the ulna in full extension. The proximal end of the radius consists of a head, neck and tuberosity. The radial head is cup-shaped superiorly for articulation with the capitulum. The periphery of the head is an articulating surface for the superior radioulnar joint, articulating with the inner surface of the annular ligament. The radial tuberosity gives insertion to the biceps tendon.
At the proximal end of the ulna is the massive, hook-shaped olecranon process. Anteriorly, the coronoid process arises with the radial notch on its medial side for articulation with the radius at the superior radioulnar joint. The elbow joint itself permits flexion and extension coupled with a small amount of adjunct rotation (Standring 2009). About 160° of passive flexion exists as the bones become almost parallel and the radial and coronoid fossae allow for extra functional movement by accommodating the flexor muscle bulk. The normal end-feel of elbow flexion is soft due to approximation of the flexor muscles. Passive extension is achieved by locking the olecranon into the olecranon fossa; it corresponds to a 180° angle and has a hard end-feel due to bone contact.
The elbow joint receives a nerve supply from the musculocutaneous, median and radial nerves anteriorly, and the ulnar and radial nerves posteriorly (C5–C8).
The superior (proximal) radioulnar joint is a uniaxial pivot joint permitting the movements of pronation and supination. These movements occur between the circumference of the radial head in the fibro-osseous ring created by the annular ligament and the radial notch of the ulna. The annular ligament is covered internally by a thin layer of articular cartilage.
Movement occurring at the superior and inferior radio-ulnar joints is rotation of the radius around the ulna to produce pronation and supination. The range of passive pronation is approximately 85° and passive supination 90°, normally with an elastic end-feel.
The carrying angle (cubitus valgus) is evident in the anatomical position. The medial end of the distal humerus projects more distally and anteriorly than the lateral, pushing the ulna laterally to produce this valgus angle. It is approximately 10–15° in men and 20–25° in women (Palastanga et al 2006). Miyasaka (1999) cites several references suggesting that the carrying angle in women is 13–16° and noting that one large study demonstrated no difference in the carrying angle between men and women.
The cubital fossa is situated on the anterior aspect of the elbow. Its proximal border is an imaginary line drawn between the two epicondyles of the humerus; its lateral border is brachioradialis and its medial border is pronator teres. On the floor of the fossa lies supinator and biceps and the roof is formed by the overlying skin and fascia. The contents of the cubital fossa, from lateral to medial, are the tendon of the biceps in the centre, the brachial artery and the median nerve.
Contractile structures
Biceps brachii (musculocutaneous nerve C5–C6) has two heads of origin. The muscle ends in a stout tendon which attaches deeply to the posterior aspect of the radial tuberosity. As the tendon passes to its insertion it twists so that its anterior surface comes to rest laterally. The tendon is separated from the anterior aspect of the radial tuberosity by the subtendinous bicipital bursa. The bicipital apo-neurosis arises anteromedially from the distal end of the tendon and sweeps medially to blend with the antebrachial fascia. Biceps is a powerful elbow flexor. Its secondary action, due to its insertion on the medial aspect of the radius, is to assist supinator in supination of the forearm, particularly with the elbow joint in 90° of flexion; it has no supinating action in the extended elbow.
Brachialis (musculocutaneous nerve C5–C6) takes origin from the anterior aspect of the lower half of the shaft of the humerus and inserts into the coronoid process of the ulna. As it crosses the elbow joint some of its deep fibres insert into the capsule of the elbow joint. Its action is to flex the elbow in either pronation or supination.
Brachioradialis (radial nerve C5–C7) passes from a long attachment on the upper two-thirds of the lateral supracondylar ridge of the humerus to the distal end of the radius just above the styloid. It flexes the elbow, being most effective in the mid-pronation–supination position.
Triceps (radial nerve C6–C8) has three heads of origin above the elbow, with its tendon inserting into the olecranon process. It is the main elbow extensor and is involved in pushing and thrusting activities as well as raising body weight on semiflexed elbows, as in getting up from a chair.
Pronator teres (median nerve C6–C7) has two heads of origin: a humeral head from just above the medial epicondyle, the coronoid process and from the common flexor tendon, and an ulnar head from the medial side of the coronoid process. It passes down and laterally to insert into a roughened area along the lateral aspect of the shaft of the radius. Its main action is to pronate the forearm, especially against resistance.
Pronator quadratus (median nerve C8, T1) binds the lower parts of the radius and ulna and is the principal pronator of the forearm.
Supinator (posterior interosseous nerve C5–C6) has its proximal attachment from the supinator crest of the ulna, lateral epicondyle of the humerus and the radial collateral and annular ligaments. It wraps round the elbow obliquely, laterally and distally, to insert into the proximal third of the radius, and supinates the forearm, bringing the palm of the hand to face upwards, whatever the degree of flexion at the elbow.
Extensor carpi radialis longus (radial nerve C6–C7) takes its main origin from the lower third of the lateral supracondylar ridge, in part deep to the origin of brachioradialis, and some origin from the common extensor tendon. It passes to the radial side of the base of the second metacarpal.
Extensor carpi radialis brevis (posterior interosseous nerve C7–C8) takes its main origin from the lateral epicondyle via the common extensor tendon, in part deep to extensor carpi radialis longus, and inserts into the radial side of the base of the third metacarpal. It is very commonly involved in tennis elbow.
Extensor carpi radialis longus and brevis extend the wrist and produce radial deviation. They work synergistically with the finger flexor tendons by holding the wrist in extension, allowing the finger flexors to form an effective grip (Palastanga et al 2006).
Other muscles which share the origin from the common extensor tendon with extensor carpi radialis brevis and are also responsible for wrist extension are extensor digitorum, extensor digiti minimi and extensor carpi ulnaris (which also produces ulnar deviation). All of these muscles are supplied by the posterior interosseous nerve (C7–C8).
Flexor carpi radialis (median nerve C6–C7) arises from the medial epicondyle via the common flexor tendon and becomes tendinous above the wrist, before passing through its own lateral compartment under the flexor retinaculum. It inserts into the bases of the second and third metacarpals.
Palmaris longus (median nerve C7–C8), often absent, arises from the medial epicondyle via the common flexor tendon and passes over, not under, the flexor retinaculum, attaching to the distal flexor retinaculum and the palmar aponeurosis.
Flexor digitorum superficialis (median nerve C7–C8, T1) lies in a slightly deeper plane than the above flexor muscles and has a humeral head from the medial epicondyle via the common flexor tendon and a small radial head. It divides to pass under the flexor retinaculum before entering the fingers to attach to the middle phalanx of each.
Flexor carpi ulnaris (ulnar nerve C7–C8) has two heads of origin: a small humeral head from the medial epicondyle via the common flexor origin and an ulnar head from the ulna. It passes over the retinaculum into pisiform.
GUIDE TO SURFACE MARKING AND PALPATION
Lateral aspect (Fig. 6.1)
Palpate the lateral supracondylar ridge, which is a sub-cutaneous sharp ridge, giving part origin to extensor carpi radialis longus and brachioradialis.
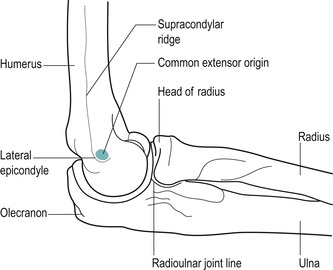 |
| Figure 6.1 Lateral aspect of the elbow in mid-position. |
The lateral supracondylar ridge terminates in the lateral epicondyle, a small bony projection which you will palpate more easily if the elbow is flexed.
Visualize the small facet on the anterolateral aspect of the lateral epicondyle which gives origin to the common extensor tendon of the superficial wrist extensor muscles. This facet is approximately the size of the patient’s little finger nail. This appears to impose a mechanical dis-advantage, since large forces are transmitted through the common extensor tendon to this small site, leading to possible strain. The area may also be vulnerable to shearing stresses during all movements of the forearm.
Palpate the head of the radius on the lateral side of the extended forearm; it is located in a posterior depression just distal to the lateral epicondyle. Confirm the correct position by rotating the forearm to feel the radial head move under your finger.
Move proximally a short distance to palpate the radiohumeral joint line, just above the radial head. It can also be palpated by dropping into the dimple on the posterolateral aspect of the olecranon. The gap between the head of the radius and the capitulum of the humerus should be obvious; flex your elbow and feel the joint open, providing the most accessible point for an intra-articular injection. Flexion past 45° tightens the joint capsule, making the joint line less obvious. Identify brachioradialis, the most superficial forearm muscle on the lateral side of the forearm, by flexing the elbow against resistance in the mid-pronation–supination position.
Medial aspect (Fig. 6.2)
Palpate the medial supracondylar ridge which ends in the rounded knob of the medial epicondyle. Identify the medial epicondyle, which is subcutaneous and most easily felt with the elbow in extension. Palpate the anterior aspect of the medial epicondyle, which provides the attachment for the common flexor tendon of the superficial wrist flexor muscles.
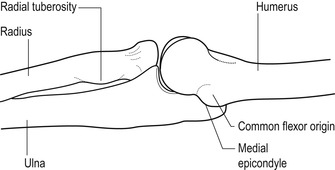 |
| Figure 6.2 Medial aspect of the elbow in extension. |
Visualize the position of the superficial wrist flexor muscles by placing the thenar eminence of one hand onto the opposite medial epicondyle, and spread the digits down the forearm to represent the following tendons (Fig. 6.3):
• Thumb: pronator teres
• Index: flexor carpi radialis
• Middle: palmaris longus
• Ring: flexor digitorum superficialis (deeper than the others and not so obvious)
• Little: flexor carpi ulnaris.
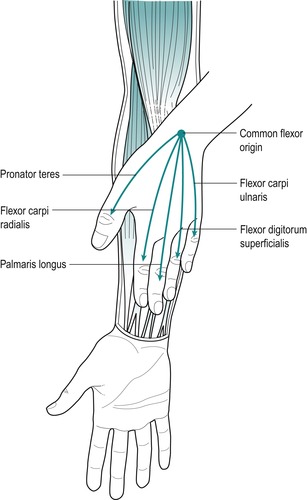 |
| Figure 6.3 The position of the muscles arising from the common flexor origin. |
Anterior aspect
It is not possible to palpate the joint line of the elbow anteriorly because of the position of the flexor muscles, but it can be visualized approximately 1 cm below the elbow flexor crease that connects the medial and lateral epicondyles (Miyasaka 1999, Palastanga et al 2006).
Locate the tuberosity of the radius by flexing the elbow to make the tendon of the biceps more obvious. Follow the tendon down to its insertion onto the radial tuberosity. The tendon of the biceps will be easily palpable as it passes deep into the cubital fossa, but the tuberosity may not feel distinct to the palpating finger, although it is tender to deep palpation.
Place the arm in the anatomical position of elbow extension and supination and note the obvious valgus angle, known as the carrying angle. It should be symmetrical bilaterally.
Posterior aspect
COMMENTARY ON THE EXAMINATION
Observation
Before proceeding with the history, a general observation of the patient’s face, posture and gait will alert the examiner to abnormalities and serious illness. The acute elbow is usually held in a position of flexion and a degree of supination, with medial rotation at the shoulder and the patient nursing the arm in a position of comfort.
Lesions commonly found at the elbow are due to overuse when abnormalities of posture are not usually observed.
History (subjective examination)
The age, occupation, sports, hobbies and lifestyle of the patient may give an indication of the nature of the onset and cause of the injury, and will alert the examiner to possible postural or overuse problems. It may also give an indication of whether the source of the problem is in the cervical spine.
Age may be relevant, as certain conditions affect particular age groups, for example conditions such as ‘pulled elbow’ (a subluxation of the small radial head in the relatively immature annular ligament), which affects children in the 1–4 years age group. Degenerative osteo-arthrosis generally affects the elderly, while rheumatoid arthritis may involve the elbow at any age. Loose bodies can occur in adolescents, associated with osteochondritis dissecans, or in the middle-aged/elderly group, associated with degenerative changes in the articular cartilage. The overuse lesions of tennis and golfer’s elbow tend to be a problem of middle age as the ageing process causes the tendinous material to become less extensible and more prone to injury.
The elbow joint and surrounding structures are situated within the C5–C7 and T1 dermatomes. However, the site of pain is usually well localized, indicating a less severe, superficial lesion. A spread of pain would indicate a more irritable lesion and possibly referral of pain from a deeper, more proximal structure.
The patient may report local tenderness with an olecranon bursitis or, more commonly, with a tennis or golfer’s elbow, which may produce a diffuse reference of pain into the forearm, as well as point tenderness over either the lateral or medial epicondyle, respectively.
The onset of the symptoms may be sudden, due to trauma, or gradual, due to overuse or arthritis. If the onset is traumatic in nature the mechanism of injury should be deduced. Acute injuries include dislocations and fractures of the radial head, olecranon and distal humerus (Safran 1995).
Hyperextension injuries may cause a capsulitis, or a fall on the out-stretched hand may cause fracture (e.g. supracondylar, distal radius or ulna) and/or dislocation. Possible neurovascular complications, secondary to trauma, should be kept in mind.
A sudden onset of pain associated with locking of the elbow could indicate a loose body.
The duration of the symptoms may be long-standing. The most common lesions at the elbow are due to chronic overuse and result in the enthesiopathies of tennis elbow (lateral epicondylar tendinopathy) and golfer’s elbow (medial epicondylar tendinopathy). The common tendons of the forearm flexors and extensors are susceptible to excessive use because they function across two joints. The causative factors may be intrinsic overload, from the force of muscle contraction; extrinsic overload, through excessive joint torque forces stressing the connective tissue, stretching and eventually disrupting it; or a combination of intrinsic and extrinsic forces (Safran 1995).
These overuse injuries are often associated with the middle-aged racquet sports player or individuals participating in throwing activities. Throwing motions may produce a valgus stress on the medial elbow and compressive forces at the lateral elbow. Such repetitive actions may result in microtrauma to the joint or surrounding tissues (Nicola 1992).
Climber’s elbow affects brachialis, as climbing involves the use of the semi-flexed pronated forearm (Safran 1995). Overuse may cause friction between the radial tuberosity and the biceps tendon, resulting in inflammation of the biceps subtendinous bursa, or an overuse lesion in the tendon itself.
The duration of symptoms indicates the stage of the lesion in the inflammatory process and will also give an indication for the likely length of treatment, with more chronic lesions usually taking longer to resolve. The common presentation of tennis or golfer’s elbow is pain of weeks’ or even months’ duration, while the less common loose body has recurrent episodes of twinging, often resolving spontaneously. Arthritis is characterized by recurrent episodes of exacerbation of symptoms and has usually been present for months or years.
The symptoms and behaviour need to be considered. The behaviour of the pain indicates the nature of the lesion: mechanical lesions are eased by rest and aggravated by repeated movements, particularly those involved in the mechanism of the lesion. For example, tennis elbow gives an increase of pain on gripping activities – simple things such as lifting a cup or pulling up bedclothes. Patients often report that knocking the lateral aspect of the elbow can give excruciating pain and it is very tender to touch. Other symptoms described by the patient could include twinges of pain with locking of the elbow, usually just short of full extension, which would indicate a possible loose body. A twinge of pain in the forearm on gripping is also associated with a tennis elbow, causing the patient to drop the object and giving an apparent feeling of muscle weakness.
Paraesthesia may be indicative of nerve involvement and the exact location of these symptoms should be ascertained. Paraesthesia may be referred distally from the cervical spine, but as the ulnar nerve lies in an exposed location behind the medial epicondyle, it is occasionally subject to direct trauma.
Both the posterior interosseous nerve (passing between the two heads of supinator) and the median nerve (passing between the two heads of pronator teres) are susceptible to muscular compression. This may complicate the clinical presentation of either tennis or golfer’s elbow and may be a reason for a poor response to treatment.
An indication of past medical history, other joint involvement and medications will establish whether contraindications to treatment exist, or that the lesion is part of an ongoing inflammatory arthritis. As well as past medical history, establish any ongoing conditions and treatment. Explore other previous or current musculoskeletal problems with previous episodes of the current complaint, any treatment given and the outcome of treatment.
Inspection
An inspection is conducted in standing with the upper limb resting in the anatomical position, if this can be achieved. Assess the overall posture from above down, looking for any bony deformity, noting the position of the head, the lordosis in the cervical spine, the position of both shoulders and the scapulae. Assess the carrying angle in the anatomical position, comparing it with the other side for symmetry.
Inspect for colour changes, including contusions and abrasions which are associated with direct trauma. These may be located at the point of the elbow or over either epicondyle. Bruising over the biceps or triceps muscles can occur in contact sports where a direct blow is possible. Abrasions may be a site of entry for bacteria, with septic olecranon bursitis being a possible result of such infection.
Muscle wasting may be evident in the forearm if a patient has a long or recurrent history of tennis elbow. Other muscle wasting would be unusual and would probably be a neurological sign associated with cervical pathology.
Swelling is usually associated with trauma. It may be diffuse, engulfing the elbow area, in which case the elbow will be fixed in the position of ease, to accommodate the swelling with minimal pain. The dimples seen at the back of a flexed elbow are obliterated if swelling is present, as here the capsule is lax and usually accommodates excess fluid.
Immediate swelling indicates bleeding and a possible haemarthrosis. Swelling developing 6–24 h after trauma indicates synovial irritation and capsular involvement. Local swellings are associated with direct trauma. A localized soft, boggy, fluctuating swelling may be seen over the point of the elbow and is indicative of an olecranon bursitis. Occasionally patients complain of swelling over the lateral epicondyle in tennis elbow, but this is not always evident clinically.
Palpation
Since the elbow is a peripheral joint, the joint is palpated for signs of activity. Heat indicates an active inflammation (Fig. 6.4), as does synovial thickening which is most easily palpable over the radial head in the more chronic state (Fig. 6.5). Swelling is usually most apparent in the dimples at the back of the elbow and may be palpated in that area. Other swellings such as that associated with olecranon bursitis or nodules can also be palpated to assess whether they are hard or soft.
 |
| Figure 6.4 Palpation for heat. |
 |
| Figure 6.5 Palpation for synovial thickening. |
State at rest
Before any movements are performed, the state at rest is established to provide a baseline for subsequent comparison.
Examination by selective tension (objective examination)
The suggested sequence for the objective examination will now be given, followed by a commentary including the reasoning in performing the movements and the significance of the possible findings. Comparison should always be made with the other side.
It is important to screen other joints that may refer symptoms to the region. The 5th, 6th and 7th dermatomes pass over the elbow joint region and symptoms of cervical and/or shoulder origin should be considered and ruled out as necessary. Consider too the widespread area of referral associated with cardiac pathology.
The elbow joint and the superior radioulnar joint are assessed by four passive movements looking for pain, range and end-feel. In the normal patient passive flexion has a ‘soft’ end-feel and passive extension has a ‘hard’ end-feel. At the superior radioulnar joint, passive pronation and supination have an ‘elastic’ end-feel. The signs elicited will establish whether or not the capsular pattern exists.
Elbow and superior radioulnar joints
• Resisted pronation (Fig. 6.12 a–c)
 |
 |
 |
| Figure 6.12 (a–c) Hand and body positioning for resisted pronation and supination. |
• Resisted supination (Fig. 6.12 a–c)
Pain provocation tests for tennis and golfer’s elbow
• Resisted wrist extension for tennis elbow (Figure 6.13 and Figure 6.15)
 |
| Figure 6.13 Resisted wrist extension. |
• Resisted wrist flexion for golfer’s elbow (Figure 6.14 and Figure 6.15)
 |
| Figure 6.14 Resisted wrist flexion. |
 |
| Figure 6.15 Examples of further provocative tests: (a) resisted wrist extension from the flexed position; (b) resisted wrist flexion from the extended position. |
Palpation
• Once a diagnosis has been made, the structure at fault is palpated for the exact site of the lesion
A loose body in the elbow joint produces a non-capsular pattern of movement with either limitation of passive flexion, or extension, but not both. The limited movement has an abnormal ‘springy’ end-feel.
The resisted tests are conducted for the muscles around the elbow, looking for pain and power. Resisted elbow flexion tests biceps and resisted elbow extension tests triceps. Resisted pronation tests pronator quadratus and pronator teres, but since pronator teres takes origin from the common flexor tendon, this may be an accessory sign in golfer’s elbow. Resisted supination tests biceps, since it is assessed with the elbow flexed, and supinator.
Two provocative resisted tests are conducted at the wrist to assess the common extensor and common flexor tendons for tendinopathy. Resisted wrist extension and resisted wrist flexion are assessed with the elbow joint fully extended. Since they are not required to stabilize the elbow in this close packed or locked position, they contract strongly to resist the wrist movements and allow minor lesions to be detected. To provoke pain, further provocative tests can be applied for tennis elbow, e.g. passive wrist flexion, resisted wrist extension from the flexed position, resisted radial deviation and resisted middle finger extension. For golfer’s elbow, resisted wrist flexion can be assessed from the extended position.
CAPSULAR LESIONS
The capsular pattern indicates the presence of arthritis in the joint which, at the elbow, is frequently rheumatoid arthritis. Degenerative osteoarthrosis is of itself symptom-free, but traumatic arthritis may be secondary to overuse or trauma of a restricted joint. Treatment of choice is a corticosteroid injection into the elbow joint.
Sit the patient with the elbow flexed to approximately 45° and the forearm pronated (Fig. 6.16). Locate the radiohumeral joint line on the posterolateral aspect of the elbow. Insert the needle between the head of the radius and the capitulum (Fig. 6.17). Once intra-articular, deliver the injection as a bolus. The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 6.16 Injection of the elbow joint. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree














